Abstract
Objective
Declining number of applicants and high attrition of residents are a dire reality. Surgeons in training are confronted to various stressors which interfere with their performance and may promote burnout. This study measures stress levels of Swiss surgical residents.
Methods
Swiss surgery residents taking the Surgical Basic Exam from 2016 to 2020 completed the Perceived Stress Scale 10 (PSS). The PSS measures how unpredictable, uncontrollable, and overloaded the respondents evaluate their work life. Scores up to 13 are normal, and scores around 20 are highly pathologic. High subscores of helplessness (PH) and lower subscores of self-efficacy (PSE) indicate distress.
Results
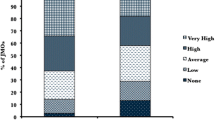
A total of 1694 questionnaires were evaluated (return rate 95.7%). Resident median (m) age was 29 years, 43.5% were female, and 72.7% of the residents were in their first 2 years of training. Residents reported a high PSS (m = 15), a high PH (m = 9), and an ordinary PSE (m = 5). Females reported worse PSS (p < 0.001), PH (p < 0.001), and PSE (p = 0.036). In multivariable analysis, male sex (p < 0.001), aiming at orthopedic (p = 0.017) or visceral surgery (p = 0.004), and French as mother tongue (p = 0.037) predicted lower stress levels, while graduating from a country not adjacent to Switzerland led to higher stress (p = 0.047).
Conclusion
Perceived stress levels are high in this prospective and representative cohort study of Swiss surgical residents. Females endured significantly worse stress and helplessness levels than males. These figures are worrisome as they may directly contribute to the declining attractivity of surgical residencies. Detailed sex-specific analysis and correction of stressors are urgently needed to improve residency programs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stress commonly describes the mental, emotional, or physical reaction caused by internal and external stimuli. Depending on the individual reaction, stress factors may cause positive (eustress) or negative (distress) stress [1]. If a situation is evaluated as overwhelming, uncontrollable and impossible to cope with, distress inevitably occurs [2]. The impact of chronic stress on all aspects of life has been studied extensively, including physical and psychological health, workplace performance, learning, and even mortality [3,4,5,6]. While there is a common understanding of the negative effects of chronic stress, its origin has various reasons, which are intensively researched. Consequently, many different assessment forms exist with emphasis on a biological, environmental, or psychological origin or a combination thereof [7,8,9,10,11].
The psychological approach focuses on individual appraisal of stress and reflects the individual significance of stress factors and the coping skills at hand [12]. The Perceived Stress Scale (PSS), a self-reporting measurement, was developed and published by Sheldon Cohen in 1983 [3]. It is one of the most frequently used and well-established psychological instruments for measuring perceived stress. The 10-item questionnaire (PSS-10) is designed to assess how unpredictable, uncontrollable, and overloaded the respondents value their work lives over the past month. The final result consists of two subscores, perceived helplessness and perceived self-efficacy (the ability to cope) [13]. The PSS-10 instrument has been translated in various languages, and it was used in a multitude of populations and cultures [14]. It is considered applicable for the majority of human populations and its different subgroups. In particular, both the German and French versions were extensively validated [15, 16]. Furthermore, it requires little time to be completed [17].
High levels of stress may occur within the healthcare environment. Countless studies have shown the negative impact of stress exposure on medicine, pharmacy, and nursing students and professionals [18, 19], including depression and suicide thoughts affecting medical students and physicians [20, 21]. However, very few studies have focused on surgical residents. Importantly, behavioral career patterns are often established in the first years of surgical training. Within this decisive time window, young surgeons are exposed to high expectations and various stressors, which may lead to gradual exhaustion, interfere with their clinical performance, and result in a burnout and residency attrition [22]. Hence, understanding and mitigating stress in surgical residents is critical to the maintenance of the surgical workforce with an expected shortage of tens of thousands of surgeons within a decade in Europe and North America [23].
Considering the steadily declining number of applicants for surgical specialties in Switzerland and Europe and a worrisome attrition rate in North America [24,25,26,27,28], investigations of the causes of the observed disenchantment, including the impact of the learning and workplace environments, are urgently needed [29,30,31,32,33].
The present study aims at measuring the perceived stress levels of surgical residents in Switzerland, considering sex, age, nationality, and country of graduation.
Methods
Participants and setting
Swiss residents who took the first step examination of surgical qualifications between 2016 and 2020 were offered to voluntarily and anonymously complete the PSS-10 either in its validated German or French translations while registering for the examination. Medical school is taught in German or French in Switzerland, while 90% of the hospitals operate in German or French and 10% in Italian.
Swiss board certification in a surgical discipline requires a two-part assessment. Passing the first part of the specialty examination is mandatory for residents in general surgery, thoracic surgery, cardiac surgery, vascular surgery, orthopedics, hand and plastic surgery, pediatric surgery, maxillofacial surgery, and urology. Residents are advised to take the written examination once they have completed their first 2 years of training (common trunk). The test focuses on medical and surgical knowledge common to all surgical disciplines, including perioperative management, elective and emergency procedures, and basic knowledge of oncology, immunology, infectiology, pathophysiology, law, and ethics. Once the Surgical Basic Exam has been passed and the 2-year common trunk completed, residents may opt for specialized training, e.g., urology or cardiac surgery, or stay in a broader discipline, e.g., general surgery or orthopedics. Residents then graduate after 4 more years of training and passing the second part of the specialty examination to become board certified.
PSS-10
The PSS is a validated tool to measure how unpredictable, uncontrollable, and overloaded the respondents evaluate their work life over the last month [3, 13,14,15,16, 34,35,36]. Each of the ten items is rated on a five-point Likert scale from 0 (never) to 4 (very often). Hence, individual scores can range from 0 to 40. A high PSS score indicates a high level of stress, with scores around 13 considered as average and scores around 20 as highly pathologic [36, 37]. Two subscores are included in the PSS [38, 39]: perceived helplessness (PH) and perceived self-efficacy (PSE, which has a reverse scale: High value indicates low level of perceived self-efficacy). PH emphasizes the individual’s reaction to stress, while PSE denotes the self-assessed ability to cope with these stressors. A high PSS score as well as a high “helplessness” subscore indicates distress, while a high “self-efficacy” subscore represents a lower ability to cope with stressors [15].
Statistical analyses
Descriptive statistics were used to summarize patients’ characteristics. Normality was assessed using graphical methods (Q–Q plots and histograms) and the Shapiro–Wilk test. Continuous variables were reported as mean and standard deviation (SD) or median and interquartile range (IQR) and compared between the two groups using two-sample independent t-tests or Mann–Whitney U test according to data distribution. For comparisons between more than two groups, the Kruskal–Wallis test was applied with post hoc analyses (Dunn’s post hoc test) of the subgroups and subsequent Bonferroni correction for multiple comparisons.
Paired continuous variables were compared using paired-samples t-test.
Categorical variables were summarized as frequencies (%) and compared using Pearson’s Chi-squared test or Fisher’s exact test where applicable. In cases of ≥10% missing information for a variable, the number of participants with complete information is reported.
Age was categorized as 5-year intervals (<25, 26–30, 31–35, 36–40, >40).
Multivariable linear regression analyses were conducted with PSS-10 score, PH score, and PSE score as dependent variables and age, sex, specialty aspired, position, native language, and duration of training as independent variables. Variable selection for univariable analysis was a priori determined based on clinical parameters and literature review [36, 40, 41]. Variables with a p-value less than 0.10 in univariable analysis were retained in the multivariable models.
Categorical variables were coded as dummy variables. Independent variables were entered simultaneously.
SPSS version 25 (IBM Corp., Armonk, NY) was used for data analysis. P-values ≤ 0.05 are considered statistically significant.
Ethical approval
Examinees taking the first part of the board examination and queried in the present study agreed to the use of their personal data. This study was approved by the regional ethical board (Ethikkommission Nordwest- and Zentralschweiz, Swissethics study ID 2019-00167). Data management was compliant with the Swiss Federal Data Protection Act.
Results
Out of 1770 distributed questionnaires over the study period of 5 years, 1694 (95.7%) were returned and included in the current analysis. Men accounted for 56.5% and women for 43.5% of the responders with a median age of 29 years (IQR 27.6–31.0 years). Distribution of the demographic characteristics of the responders did not differ from the overall examination takers. Median duration of training of all participants was 12 months (IQR 4–24), whereas 27% (n = 460) of the participants had more than two years of training. Orthopedic surgery (n = 406, 24%) and general surgery (n = 402, 23.8%) were the two specialties most sought for.
Men were slightly older (median 29.2 years, IQR 27.8–31.2 years) than women (28.7 years, IQR 27.2–30.1 years), p < 0.001. Males aimed predominantly at a specialty in orthopedic surgery (n = 285, 40.5%), while females preferred general surgery (n = 209, 41.1%). Only 38.7% of the surgical residents in Switzerland graduated from a Swiss medical school. Baseline demographics of the overall cohort are presented in Table 1.
Median PSS-10 score of the overall cohort was 15.0 points (IQR 11.0–19.0) with subscores of PH of 9.0 (IQR 6.0–13.0) and of PSE of 5.0 points (IQR 4.0–7.0). In univariate analysis, female sex was uniformly associated with worse stress levels across all dimensions. Aiming at a specialty in general surgery, having graduated in Italy and/or being an Italian was also related to worse stress scores, whereas being a French/having French as a native language and aspiring to a specialty in visceral surgery was protective. Last, stress scores were not affected by the duration of surgical training or the hierarchical position of the resident. Table 2 summarizes the PSS-10, the PH, and the PSE scores of the overall cohort and for several subgroups of the study population.
When compared to a contemporary, age-matched reference group of the general population [15], Swiss surgical resident demonstrated significantly worse summative PSS scores (15. 0 vs. 12.74, p < 0.001) and PH (9.0 vs. 7.6, p < 0.001). This observation holds true for both men and women. Noteworthy, Swiss residents scored better than the reference population in PSE (M 5.0 vs. M 5.8, p < 0.001).
In multivariable regression analysis, male sex independently predicted better PSS-10 (β = −1.201, p < 0.001) and PH score (β = −1.154, p < 0.001) when controlled for age (PH score only), specialty, nationality, country of graduation, hierarchical position, native language, and duration of training. Longer duration of training was an independent predictor for decreasing levels of PSS and PH, reaching statistical significance when the last year of residency was compared to the end of the common trunk (12–24 months of training).
Residents in orthopedic (β = −1.119, p = 0.003) and visceral surgery (β = −2.080, p = 0.001) and those who had more than 5 years of training (β = −2.190, p = 0.017) were less stressed out and were less prone to helplessness. Similarly, perceived self-efficacy was better in residents training in orthopedics, urology, and visceral surgery.
Conversely, Italian citizenship and native language, graduating from a country not adjacent to Switzerland, and one year or less of training exposed to higher stress and lower self-efficacy. Further, perceived helplessness was greater in German citizens and lower for the French national, French native speaker and graduate, and for those with more than 5 years training. Detailed results of all regression models are reported in Tables 3, 4, and 5.
Discussion
This study reported the first nationwide analysis on perceived stress levels, helplessness, and self-efficacy in surgical residencies, using an established and validated instrument and a representative sample of Swiss surgical residents queried over 5 years [42,43,44]. Two North American studies [45, 46] investigated stress levels in vascular and general surgeons, yet these reports are not representative of US surgical residencies at large. To the best of our knowledge, there are no similar studies available for European surgical residents.
The demographics of the present cohort match the overall medical demographics in Switzerland. Indeed, in 2020 practicing physicians in Switzerland (all medical specialties) were 56% male and 44% female, whereas 37.4% of the Swiss medical workforce graduated from a foreign medical school. Gender balance is roughly similar to the figures reported by most countries of the Organisation for Economic Cooperation and Development, but for the share of international medical graduates (IMG) for which Switzerland tops all ranking with 37.4% IMG, compared to 26% IMG in the USA, 11.5% in France and Germany, and 9.4% in Denmark [47, 48].
Chronic stress has a proven negative effect on health, performance, and learning [36, 49, 50]. Suboptimal working and learning environment have a negative impact on workplace efficiency, resident’s mental condition, and attrition [22, 51,52,53,54]. The present study reported markedly higher level of negative stress and helplessness in surgery residents when compared to the general population. The even worse scores demonstrated by female residents are a further major concern, as women represent the majority of medical graduates in many countries and a growing share of surgical residents. Indeed, 43.5% of the Swiss surgical residents in the present study were women. A study investigating first- and second-year residents workplace experience in the early 2000 in Switzerland already reported higher levels of effort–reward imbalance in females and in surgical specialties, than in males and in medical specialties [55]. In an American longitudinal study of surgical residents, female sex was the independent factor most strongly associated with residency attrition [56], while a meta-analysis including 19,821 American residents revealed an overall attrition prevalence of 18%, affecting predominantly female residents (25% vs. 15% in males, p = 008), whereas half of the residents left after their first postgraduate year [57]. In prior reports across different industries and countries, women also reported higher stress scores than males [16, 35, 58], in agreement with the present study. Hence, the present results are alarming at a time where many countries struggle to maintain their surgical workforce, in the Western world and in the developing world alike.
Switzerland is an immigration country with every fifth person living in the country not holding Swiss citizenship [36] and a high dependence of Swiss health care toward foreign healthcare workers, as illustrated by the fact that 37.4% of the Swiss medical workforce did not graduate in Switzerland [48]. In surgical residencies, dependence toward IMG is even greater: While in the prior decade 2002–2012 [59], a slight majority of surgical residents (55%) graduated from a Swiss medical school, in the present cohort the share of Swiss graduates decreased to 38.7% and seems to stabilize around 40% if one takes into account the data from the 2021 Surgical Basic Exam. In this context, the observed vulnerability of Italian nationals to stress, who represent 10% of the present cohort, is another concern, shared by foreign medical graduates not coming from a country adjacent to Switzerland. Indeed, migrant workers are confronted to acculturative stress in most industries and countries [60].
These findings should be addressed to improve medical training environments and create more supportive and inclusive residency programs. In this context, stress coping and stress reduction initiatives may prevent burnout and resident attrition, whereas these initiatives should be preferentially directed toward female and foreign residents [61, 62].
Earlier studies have classified stressors at medical school and residency into three main categories: academic pressures, social factors including age, sex, ethnicity, and relationship status, and financial problems [33, 36, 37, 40, 49, 62, 63]. This study found no association with age, while country of graduation and foreign mother language negatively affected stress level. Relationship and parental status were not investigated in the present study. US studies of residents’ well-being have shown that parenthood affected stress levels of surgical residents, women more than men, and this important point deserves further investigation and attention [61, 64,65,66]. Providing day care opportunities compliant with working schedules of residents, and shared parental responsibilities that allow a father to grow in his role are obvious steps, dearly requested yet rarely witnessed [61, 66].
Financial data were not collected, although debt and financial stress have been associated with attrition from surgical residency [67]. Yet, debt is uncommon for Swiss medical graduates as Swiss medical schools are virtually tuition-free while student grants are largely available to cover cost of living when needed. Furthermore, the average entry salary of a resident is higher than the median income in Switzerland, allowing for a stress-free living, in financial terms at least. Higher income and purchasing power in Switzerland is frequently reported as one of the reasons for an international medical graduate to seek employment and residency in Switzerland [68, 69].
Proper information of incoming residents on the structure, requirements, and overall organization of the residency programs is one of the easier actions to undertake with the potential to better align expectations with reality and avoid deception and attrition [70]. Mentorship and physician assistance programs are a further way to improve residency: They can be used to attract medical student toward surgical specialties and most importantly to retain residents in training. Structured assistance and counseling aimed at improving work–life balance, supporting family life, increasing access to mental health support, and supporting career transitions have improved residents’ attrition rate and well-being [71, 72].
While the present study was nationwide and hence representative, it did not investigate in more details further potential stressors in residency that may account for the higher level of stress reported. As discussed above, such a detailed analysis was performed in medical schools students [18, 45] and some of the reported student stressors could be investigated in the present study. Also, possible differences between academic and non-academic residency programs were not investigated, whereas prior reports suggested a higher attrition rate in academic institutions and during a research year [55, 73,74,75].
While internal consistency of the PSS-10 instrument was demonstrated, response and time bias may have affected self-reported measures. Yet, the magnitude of the differences presently measured and the focus of the PSS instrument over a 4-week period more than on a given point of time should minimize this possible bias.
Last, some of the respondents did repeat the Surgical Basis Exam and this could possibly affect the perceived stress levels. While the vast majority of the respondents were first takers within 2 years of residency training, full anonymization prevents a separate analysis of examination retakers. Yet, the influence of time spent in training was accounted for in uni- and multivariable analysis, with no statistical difference by postgraduation year when compared to the reference population of residents within the first 2 years of residency.
Further studies should investigate with greater granularity the working and learning environments of surgical residents in order to better understand and improve perceived stress levels. Female residents deserve particular attention in this matter, owing to the importance of the female population and to the stronger impact of the environment on the stress levels reported by women.
Conclusion
Perceived stress levels are high in both sexes in this large, prospective, and representative cohort study of Swiss surgical residents in their early years of training. This should warrant intervention, as chronic stress is detrimental and associated with burnout and residency attrition, in particular in the first 2 years of training [57, 73, 76, 77]. These worrisome figures may directly contribute to the declining attractivity of surgical residencies, as it was suggested in a previous survey of residents’ reasons for specialty choice [78, 79]. Importantly, sex differences were remarkable and should be further addressed. Females endured significantly worse stress and helplessness levels than males. IMG, representing a large group of surgical residents, were also struggling to adapt to surgical residencies and deserve dedicated attention.
Detailed analysis and correction of stressors are urgently needed to improve residency programs.
References
Cavallo P, Carpinelli L, Savarese G (2016) Perceived stress and bruxism in university students. BMC Res Notes 9:514
Selye H (1975) Confusion and controversy in the stress field. J Human Stress 1:37–44
Cohen S, Janicki-Deverts D, Miller GE (2007) Psychological stress and disease. JAMA 298:1685–1687
Nielsen NR, Kristensen TS, Schnohr P et al (2008) Perceived stress and cause-specific mortality among men and women: results from a prospective cohort study. Am J Epidemiol 168:481–491. (discussion 492–486)
Burger K, Samuel R (2017) The role of perceived stress and self-efficacy in young people’s life satisfaction: a longitudinal study. J Youth Adolesc 46:78–90
Opoku-Acheampong A, Kretchy IA, Acheampong F et al (2017) Perceived stress and quality of life of pharmacy students in University of Ghana. BMC Res Notes 10:115
Wong ML, Anderson J, Knorr T et al (2018) Grit, anxiety, and stress in emergency physicians. Am J Emerg Med 36:1036–1039
Crawford JR, Henry JD (2003) The Depression Anxiety Stress Scales (DASS): normative data and latent structure in a large non-clinical sample. Br J Clin Psychol 42:111–131
Lovibond PF, Lovibond SH (1995) The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther 33:335–343
Gomes AR, Teixeira PM (2016) Stress, cognitive appraisal and psychological health: testing instruments for health professionals. Stress Health 32:167–172
Carpenter R (2016) A review of instruments on cognitive appraisal of stress. Arch Psychiatr Nurs 30:271–279
Folkman S, Lazarus RS, Gruen RJ et al (1986) Appraisal, coping, health status, and psychological symptoms. J Pers Soc Psychol 50:571–579
Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24:385–396
Lee EH (2012) Review of the psychometric evidence of the perceived stress scale. Asian Nurs Res (Korean Soc Nurs Sci) 6:121–127
Klein EM, Brahler E, Dreier M et al (2016) The German version of the Perceived Stress Scale—psychometric characteristics in a representative German community sample. BMC Psychiatry 16:159
Lesage FX, Berjot S, Deschamps F (2012) Psychometric properties of the French versions of the Perceived Stress Scale. Int J Occup Med Environ Health 25:178–184
Kopp MS, Thege BK, Balog P et al (2010) Measures of stress in epidemiological research. J Psychosom Res 69:211–225
Shah MHS, Malik S, Sreeramareddy CT (2010) Perceived stress, sources and severity of stress among medical undergraduates in a Pakistani medical school. BMC Med Educ 10(1):2
Dahlin M, Joneborg N, Runeson B (2005) Stress and depression among medical students: a cross-sectional study. Med Educ 39:594–604
Tyssen R, Vaglum P, Grønvold NT et al (2001) Factors in medical school that predict postgraduate mental health problems in need of treatment. A nationwide and longitudinal study. Med Educ 35:110–120
Tyssen R, Vaglum P, Gronvold NT et al (2001) Suicidal ideation among medical students and young physicians: a nationwide and prospective study of prevalence and predictors. J Affect Disord 64:69–79
Wetzel CM, Kneebone RL, Woloshynowych M et al (2006) The effects of stress on surgical performance. Am J Surg 191:5–10
Colleges AoAM The Complexities of Physician Supply and Demand: Projections From 2018 to 2033, Washington, DC 20036, 2020;92
Yan Q, Jiang Z, Clothier WT et al (2021) Recruiting trainees to surgery in the United States and Canadian system—What strategies are effective? Am J Surg 221:410–423
Dow T, McGuire C, Crawley E et al (2020) Application rates to surgical residency programs in Canada. Can Med Educ J 11:e92–e100
Shweikeh F, Schwed AC, Hsu CH et al (2018) Status of resident attrition from surgical residency in the past, present, and future outlook. J Surg Educ 75:254–262
Bercot RM-F, A. (2007) La crise de recrutement des chirurgiens françaìs: entre mythes et réalités. Rev Fr Sociol 48:29
Schneider KN, Masthoff M, Gosheger G et al (2020) Generation Y in surgery-the competition battle for talent in times of talent shortage. Chirurg 91:955–961
Bartlett J (2018) Addressing the recruitment shortfall in surgery - How do we inspire the next generation? Ann Med Surg (Lond) 25:30–32
Marshall LL, Allison A, Nykamp D et al (2008) Perceived stress and quality of life among doctor of pharmacy students. Am J Pharm Educ 72:137
Wiegner L, Hange D, Bjorkelund C et al (2015) Prevalence of perceived stress and associations to symptoms of exhaustion, depression and anxiety in a working age population seeking primary care–an observational study. BMC Fam Pract 16:38
Sohail N (2013) Stress and academic performance among medical students. J Coll Physicians Surg Pak 23:67–71
Schmidt LE, Cooper CA, Guo WA (2016) Factors influencing US medical students’ decision to pursue surgery. J Surg Res 203:64–74
Al-Dubai SA, Alshagga MA, Rampal KG et al (2012) Factor structure and reliability of the Malay version of the Perceived Stress Scale among Malaysian medical students. Malays J Med Sci 19:43–49
Barbosa-Leiker C, Kostick M, Lei M et al (2013) Measurement invariance of the perceived stress scale and latent mean differences across gender and time. Stress Health 29:253–260
Zinurova E, DeHart R (2018) Perceived stress, stressors, and coping mechanisms among PGY1 pharmacy residents. Am J Pharm Educ 82:6574
Birks Y, McKendree J, Watt I (2009) Emotional intelligence and perceived stress in healthcare students: a multi-institutional, multi-professional survey. BMC Med Educ 9:61
Hewitt PL, Flett GL, Mosher SW (1992) The Perceived Stress Scale: factor structure and relation to depression symptoms in a psychiatric sample. J Psychopathol Behav Assess 14:247–257
Roberti JW, Harrington LN, Storch EA (2006) Further Psychometric support for the 10-item version of the Perceived Stress Scale. J Coll Couns 9:135–147
Silverstein ST, Tanbonliong T, Kritz-Silverstein D (2020) Stress and coping strategies in pediatric dental residents. J Dent Educ
Lala AI, Sturzu LM, Picard JP et al (2016) Coping behavior and risk and resilience stress factors in French regional emergency medicine unit workers: a cross-sectional survey. J Med Life 9:363–368
Gonzalez-Ramirez MT, Rodriguez-Ayan MN, Hernandez RL (2013) The perceived stress scale (PSS): normative data and factor structure for a large-scale sample in Mexico. Span J Psychol 16:E47
Chaaya M, Osman H, Naassan G et al (2010) Validation of the Arabic version of the Cohen Perceived Stress Scale (PSS-10) among pregnant and postpartum women. BMC Psychiatry 10:111
Leung DY, Lam TH, Chan SS (2010) Three versions of Perceived Stress Scale: validation in a sample of Chinese cardiac patients who smoke. BMC Public Health 10:513
Smeds MR, Janko MR, Allen S et al (2020) Burnout and its relationship with perceived stress, self-efficacy, depression, social support, and programmatic factors in general surgery residents. Am J Surg 219:907–912
Janko MR, Smeds MR (2019) Burnout, depression, perceived stress, and self-efficacy in vascular surgery trainees. J Vasc Surg 69:1233–1242
Association AM International Medical Graduates Section (IMGS), 2021
Hostettler SK, E. (2021) Statistique médicale 2020 de la FMH: la Suisse en comparaison internationale. Bulletin des Médecins Suisses 102:6
Backovic DV, Zivojinovic JI, Maksimovic J et al (2012) Gender differences in academic stress and burnout among medical students in final years of education. Psychiatr Danub 24:175–181
Kheiraoui F, Gualano MR, Mannocci A et al (2012) Quality of life among healthcare workers: a multicentre cross-sectional study in Italy. Public Health 126:624–629
Buddeberg-Fischer B, Klaghofer R, Stamm M et al (2008) Work stress and reduced health in young physicians: prospective evidence from Swiss residents. Int Arch Occup Environ Health 82:31–38
Loerbroks A, Weigl M, Li J et al (2016) Effort-reward imbalance and perceived quality of patient care: a cross-sectional study among physicians in Germany. BMC Public Health 16:342
Maher Z, Milner R, Cripe J et al (2013) Stress training for the surgical resident. Am J Surg 205:169–174
Goldman LI, McDonough MT, Rosemond GP (1972) Stresses affecting surgical performance and learning. I. Correlation of heart rate, electrocardiogram, and operation simultaneously recorded on videotapes. J Surg Res 12:83–86
Buddeberg-Fischer B, Klaghofer R, Abel T et al (2005) Junior physicians’ workplace experiences in clinical fields in German-speaking Switzerland. Swiss Med Wkly 135:19–26
Yeo HL, Abelson JS, Mao J et al (2017) Who makes It to the end? A novel predictive model for identifying surgical residents at risk for attrition. Ann Surg 266:499–507
Khoushhal Z, Hussain MA, Greco E et al (2017) Prevalence and causes of attrition among surgical residents: a systematic review and meta-analysis. JAMA Surg 152:265–272
Remor E (2006) Psychometric properties of a European Spanish version of the Perceived Stress Scale (PSS). Span J Psychol 9:86–93
Adamina MB, K; Lange, J; Westkämper, R Evaluation of the first step examination towards Swiss board certification in general surgery. In: Helvetica JdSGfCFMC editor, Bern, 2016;1
Liem A, Renzaho AMN, Hannam K et al (2021) Acculturative stress and coping among migrant workers: a global mixed-methods systematic review. Appl Psychol Health Well Being 13:491–517
Ouyang K, Huang IA, Wagner JP et al (2021) Persistence of gender bias over four decades of surgical training. J Surg Educ 78:1868–1877
Arya S, Franco-Mesa C, Erben Y (2022) An analysis of gender disparities amongst United States medical students, general surgery residents, vascular surgery trainees, and the vascular surgery workforce. J Vasc Surg 75:5–9
Schwartz CE, Powell VE, Rapkin BD (2017) When global rating of change contradicts observed change: examining appraisal processes underlying paradoxical responses over time. Qual Life Res 26:847–857
Chen MM, Yeo HL, Roman SA et al (2013) Life events during surgical residency have different effects on women and men over time. Surgery 154:162–170
Sullivan MC, Yeo H, Roman SA et al (2013) Striving for work-life balance: effect of marriage and children on the experience of 4402 US general surgery residents. Ann Surg 257:571–576
Castillo-Angeles M, Smink DS, Rangel EL (2022) Perspectives of general surgery program directors on paternity leave during surgical training. JAMA Surg 157:105–111
Dolan PT, Symer MM, Mao JI et al (2020) National prospective cohort study describing how financial stresses are associated with attrition from surgical residency. Am J Surg 220:519–523
Statistik Bf Monatlicher Bruttolohn (Median), 2018 - Wirtschaft insgesamt, 2018
Zürich V (2020) Zusammenfassung/Gegenüberstellung der derzeitigen kantonalen und städtischen Grundlohnsystematik der Assistenzärzt*innen
Abelson JS, Sosa JA, Symer MM et al (2018) Association of expectations of training with attrition in general surgery residents. JAMA Surg 153:712–717
Wothe J, Bosacker L, Nalluri H et al (2021) Improving mental health support, career transitions and access to health care for surgical residents. J Surg Educ
Champion C, Bennett S, Carver D et al (2015) Providing mentorship support to general surgery residents: a model for structured group facilitation. Can J Surg 58:372–373
Yeo H, Bucholz E, Ann Sosa J et al (2010) A national study of attrition in general surgery training: which residents leave and where do they go? Ann Surg 252:529–534. (discussion 534–526)
Sue GR, Bucholz EM, Yeo H et al (2011) The vulnerable stage of dedicated research years of general surgery residency: results of a national survey. Arch Surg 146:653–658
Kern M, Buia A, Tonus C et al (2019) Psychological stressors, resources and well-being of surgeons in Germany: a cross-sectional study. Chirurg 90:576–584
Sullivan MC, Yeo H, Roman SA et al (2013) Surgical residency and attrition: defining the individual and programmatic factors predictive of trainee losses. J Am Coll Surg 216:461–471
Yeo HL, Abelson JS, Symer MM et al (2018) Association of time to attrition in surgical residency with individual resident and programmatic factors. JAMA Surg 153:511–517
van der Horst K, Siegrist M, Orlow P et al (2010) Residents’ reasons for specialty choice: influence of gender, time, patient and career. Med Educ 44:595–602
Buddeberg-Fischer B, Klaghofer R, Abel T et al (2006) Swiss residents’ speciality choices–impact of gender, personality traits, career motivation and life goals. BMC Health Serv Res 6:137
Funding
Open access funding provided by University of Basel.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guglielmetti, L.C., Gingert, C., Holtz, A. et al. Nationwide Study on Stress Perception Among Surgical Residents. World J Surg 46, 1609–1622 (2022). https://doi.org/10.1007/s00268-022-06521-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06521-0