Abstract
Background
There has been longstanding uncertainty over whether lower healthcare spending in Canada might be associated with inferior outcomes for hospital-based care. We hypothesized that mortality and surgical complication rates would be higher for patients who underwent four common surgical procedures in Canada as compared to the US.
Design, Setting, and Participants
We conducted a retrospective cohort study of all adults who underwent hip fracture repair, colectomy, pancreatectomy, or spine surgery in 96 Canadian and 585 US hospitals participating in the American College of Surgeons National Surgical Quality Improvement Project (ACS-NSQIP) between January 1, 2015 and December 31, 2019. We compared patients with respect to demographic characteristics and comorbidity. We then compared unadjusted and adjusted outcomes within 30-days of surgery for patients in Canada and the US including: (1) Mortality; (2) A composite constituting 1-or-more of the following complications (cardiac arrest; myocardial infarction; pneumonia; renal failure/; return to operating room; surgical site infection; sepsis; unplanned intubation).
Results
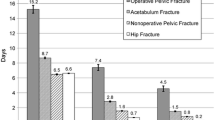
Our hip fracture cohort consisted of 21,166 patients in Canada (22.3%) and 73,817 in the US (77.7%), for colectomy 21,279 patients in Canada (8.9%) and 218,307 (91.1%), for pancreatectomy 873 (7.8%) in Canada and 12,078 (92.2%) in the US, and for spine surgery 14,088 (5.3%) and 252,029 (94.7%). Patient sociodemographics and comorbidity were clinically similar between jurisdictions. In adjusted analyses odds of death was significantly higher in Canada for two procedures (colectomy (OR 1.22; 95% CI 1.044–1.424; P = .012) and pancreatectomy (OR 2.11; 95% CI 1.26–3.56; P = .005)) and similar for hip fracture and spine surgery. Odds of the composite outcome were significantly higher in Canada for all 4 procedures, largely driven by higher risk of cardiac events and post-operative infections.
Conclusions
We found evidence of higher rates of mortality and surgical complications within 30-days of surgery for patients in Canada as compared to the US.




Similar content being viewed by others
References
Baicker K, Chandra A (2018) Challenges in understanding differences in health care spending between the United States and other high-income countries. JAMA 319(10):986–987. https://doi.org/10.1001/jama.2018.1152[publishedOnlineFirst:2018/03/15]
Padget M, Biondi N, Brownwood I. 2020 Methodological development of international measurement of acute myocardial infarction 30-day mortality rates at the hospital level: OECD.
Papanicolas I, Woskie LR, Jha AK (2018) Health care spending in the United States and other high-income countries. JAMA 319(10):1024–1039. https://doi.org/10.1001/jama.2018.1150[publishedOnlineFirst:2018/03/15]
Samsky MD, Ambrosy AP, Youngson E et al (2019) Trends in readmissions and length of stay for patients hospitalized with heart failure in Canada and the United States. JAMA Cardiol 4(5):444–453. https://doi.org/10.1001/jamacardio.2019.0766[publishedOnlineFirst:2019/04/11]
Cram P, Landon BE, Matelski J et al (2018) Utilization and short-term outcomes of primary total hip and knee arthroplasty in the United States and Canada: an analysis of New York and Ontario administrative data. Arthritis Rheumatol 70(4):547–554. https://doi.org/10.1002/art.40407[publishedOnlineFirst:2017/12/30]
Chung SC, Gedeborg R, Nicholas O et al (2014) Acute myocardial infarction: a comparison of short-term survival in national outcome registries in Sweden and the UK. Lancet 383(9925):1305–1312. https://doi.org/10.1016/s0140-6736(13)62070-x[publishedOnlineFirst:2014/01/28]
Rapsomaniki E, Thuresson M, Yang E et al (2016) Using big data from health records from four countries to evaluate chronic disease outcomes: a study in 114 364 survivors of myocardial infarction. European Heart Journal - Quality of Care and Clinical Outcomes 2(3):172–183. https://doi.org/10.1093/ehjqcco/qcw004
Cohen ME, Ko CY, Bilimoria KY et al (2013) Optimizing ACS NSQIP modeling for evaluation of surgical quality and risk: patient risk adjustment, procedure mix adjustment, shrinkage adjustment, and surgical focus. J Am Coll Surg 217(2):336–346. https://doi.org/10.1016/j.jamcollsurg.2013.02.027[publishedOnlineFirst:2013/05/01]
Hart A, Bergeron SG, Epure L et al (2015) Comparison of US and Canadian perioperative outcomes and hospital efficiency after total hip and knee arthroplasty. JAMA Surg. https://doi.org/10.1001/jamasurg.2015.1239[publishedOnlineFirst:2015/08/20]
American College of Surgeons. 2016 American College of Surgeons National Surgical Quality Improvement Program Users Guide.
Lawson EH, Louie R, Zingmond DS et al (2012) A comparison of clinical registry versus administrative claims data for reporting of 30-day surgical complications. Ann Surg 256(6):973–981. https://doi.org/10.1097/SLA.0b013e31826b4c4f[publishedOnlineFirst:2012/10/26]
Goyal A, Ngufor C, Kerezoudis P et al (2019) Can machine learning algorithms accurately predict discharge to nonhome facility and early unplanned readmissions following spinal fusion? analysis of a national surgical registry. J Neurosurg Spine 31(4):568–578. https://doi.org/10.3171/2019.3.Spine181367[publishedOnlineFirst:2019/06/08]
Maxwell BG, Mirza A (2019) Medical comanagement of hip fracture patients is not associated with superior perioperative outcomes: a propensity score-matched retrospective cohort analysis of the national surgical quality improvement project. J Hosp Med 14:E1-e7. https://doi.org/10.12788/jhm.3343[publishedOnlineFirst:2019/12/24]
Basques BA, McLynn RP, Lukasiewicz AM et al (2018) Missing data may lead to changes in hip fracture database studies: a study of the American College of Surgeons National Surgical Quality improvement program. Bone Joint J 100-B(2):226–232. https://doi.org/10.1302/0301-620x.100b2.Bjj-2017-0791.R1[publishedOnlineFirst:2018/02/14]
Xourafas D, Ashley SW, Clancy TE (2017) Comparison of perioperative outcomes between open, laparoscopic, and robotic distal pancreatectomy: an analysis of 1815 patients from the ACS-NSQIP procedure-targeted pancreatectomy database. J Gastrointest Surg 21(9):1442–1452. https://doi.org/10.1007/s11605-017-3463-5[publishedOnlineFirst:2017/06/03]
Daniel FE, Tamim HM, Hosni MN et al (2019) Short-term surgical morbidity and mortality of distal pancreatectomy performed for benign versus malignant diseases: a NSQIP analysis. Surg Endosc. https://doi.org/10.1007/s00464-019-07163-5[publishedOnlineFirst:2019/10/11]
Papageorge CM, Zhao Q, Foley EF et al (2016) Short-term outcomes of minimally invasive versus open colectomy for colon cancer. J Surg Res 204(1):83–93. https://doi.org/10.1016/j.jss.2016.04.020[publishedOnlineFirst:2016/07/28]
Nfonsam V, Aziz H, Pandit V et al (2016) Analyzing clinical outcomes in laparoscopic right vs. left colectomy in colon cancer patients using the NSQIP database. Cancer Treat Commun 8:1–4. https://doi.org/10.1016/j.ctrc.2016.03.006[publishedOnlineFirst:2016/10/25]
Cohen ME, Liu Y, Ko CY et al (2017) An examination of American College of Surgeons NSQIP surgical risk calculator accuracy. J Am Coll Surg 224(5):787–95.e1. https://doi.org/10.1016/j.jamcollsurg.2016.12.057[publishedOnlineFirst:2017/04/09]
Roos LL, Fisher ES, Brazauskas R et al (1992) Health and surgical outcomes in Canada and the United States. Health Aff 11(2):56–72. https://doi.org/10.1377/hlthaff.11.2.56[publishedOnlineFirst:1992/01/01]
Ko DT, Krumholz HM, Wang Y et al (2007) Regional differences in process of care and outcomes for older acute myocardial infarction patients in the United States and Ontario Canada. Circulation 115(2):196–203. https://doi.org/10.1161/circulationaha.106.657601[publishedOnlineFirst:2006/12/28]
Pilote L, Saynina O, Lavoie F et al (2003) Cardiac procedure use and outcomes in elderly patients with acute myocardial infarction in the United States and Quebec, Canada, 1988 to 1994. Med Care 41(7):813–822. https://doi.org/10.1097/01.mlr.0000068539.51969.36[publishedOnlineFirst:2003/07/02]
Cram P, Landon BE, Matelski J et al (2019) Utilization and outcomes for spine surgery in the United States and Canada. Spine 44(19):1371–1380. https://doi.org/10.1097/BRS.0000000000003083[publishedOnlineFirst:2019/07/02]
Ho V, Hamilton BH, Roos LL (2000) Multiple approaches to assessing the effects of delays for hip fracture patients in the United States and Canada. Health Serv Res 34(7):1499–1518
Cram P, Lix LM, Bohm E et al (2019) Hip fracture care in Manitoba, Canada and New York State, United States: an analysis of administrative data. CMAJ Open 7(1):E55–E62. https://doi.org/10.9778/cmajo.20180126[publishedOnlineFirst:2019/02/14]
Cram P, Ibrahim SA, Lu X et al (2012) Impact of alternative coding schemes on incidence rates of key complications after total hip arthroplasty: a risk-adjusted analysis of a national data set. Geriatr Orthop Surg Rehabil 3(1):17–26. https://doi.org/10.1177/2151458511435723[publishedOnlineFirst:2013/04/10]
Austin PC, van Walraven C, Wodchis WP et al (2011) Using the Johns Hopkins Aggregated Diagnosis Groups (ADGs) to predict mortality in a general adult population cohort in Ontario Canada. Med Care 49(10):932–939. https://doi.org/10.1097/MLR.0b013e318215d5e2[publishedOnlineFirst:2011/04/12]
Pang HYM, Chalmers K, Landon B et al (2021) Utilization Rates of Pancreatectomy, Radical Prostatectomy, and Nephrectomy in New York, Ontario, and New South Wales, 2011 to 2018. JAMA Netw Open 4(4):e215477. https://doi.org/10.1001/jamanetworkopen.2021.5477[publishedOnlineFirst:2021/04/20]
Doyle DJ, Goyal A, Bansal P, et al. 2020 American Society of Anesthesiologists Classification (ASA Class). StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2020, StatPearls Publishing LLC
Redelmeier DA, Thiruchelvam D, Daneman N (2008) Introducing a methodology for estimating duration of surgery in health services research. J Clin Epidemiol 61(9):882–889. https://doi.org/10.1016/j.jclinepi.2007.10.015[publishedOnlineFirst:2008/05/13]
Sun EC, Dutton RP, Jena AB (2018) Comparison of anesthesia times and billing patterns by anesthesia practitioners. JAMA Netw Open 1(7):e184288–e184388. https://doi.org/10.1001/jamanetworkopen.2018.4288
Yasaitis LC, Guan J, Ko DT et al (2020) Cardiac intervention rates for older patients with acute myocardial infarction in the United States and Ontario, 2003–2013: a retrospective cohort study. CMAJ Open 8(2):E437–E447. https://doi.org/10.9778/cmajo.20190190
Liu JB, Berian JR, Chen S et al (2017) Postoperative complications and hospital payment: implications for achieving value. J Am Coll Surg 224(5):779–86.e2. https://doi.org/10.1016/j.jamcollsurg.2017.01.041[publishedOnlineFirst:2017/02/01]
Eappen S, Lane BH, Rosenberg B et al (2013) Relationship between occurrence of surgical complications and hospital finances. JAMA 309(15):1599–1606. https://doi.org/10.1001/jama.2013.2773[publishedOnlineFirst:2013/04/18]
Simpson J (2012) Chronic Condition. Allan Lane, Toronto
Kreindler SA, Siragusa L, Bohm E et al (2017) Regional consolidation of orthopedic surgery: impacts on hip fracture surgery access and outcomes. Can J Surg 60(5):349–354. https://doi.org/10.1503/cjs.000517[publishedOnlineFirst:2017/09/21]
Grumbach K, Anderson GM, Luft HS et al (1995) Regionalization of cardiac surgery in the United States and Canada. Geographic access, choice, and outcomes. JAMA 274(16):1282–1288
Wijeysundera HC, Wong WW, Bennell MC et al (2014) Impact of wait times on the effectiveness of transcatheter aortic valve replacement in severe aortic valve disease: a discrete event simulation model. Can J Cardiol 30(10):1162–1169. https://doi.org/10.1016/j.cjca.2014.03.009[publishedOnlineFirst:2014/07/23]
Urbach DR, Bell CM, Austin PC (2003) Differences in operative mortality between high- and low-volume hospitals in Ontario for 5 major surgical procedures: estimating the number of lives potentially saved through regionalization. CMAJ 168(11):1409–1414
Aiken LH, Sloane DM, Bruyneel L et al (2014) Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet 383(9931):1824–1830. https://doi.org/10.1016/s0140-6736(13)62631-8[publishedOnlineFirst:2014/03/04]
Cram P, Chopra V, Soong C et al (2019) Reimagining inpatient care in Canadian teaching hospitals: bold initiatives or tinkering at the margins? J Hosp Med 14(4):251–253. https://doi.org/10.12788/jhm.3146[publishedOnlineFirst:2019/04/02]
Dunbar-Yaffe R, Wu RC, Oza A et al (2021) Impact of an internal medicine nocturnist service on care of patients with cancer at a large Canadian teaching hospital: a quality-improvement study. CMAJ Open 9(2):E667–E672. https://doi.org/10.9778/cmajo.20200167[publishedOnlineFirst:2021/06/20]
Schneider EC, Squires D (2017) From last to first - could the U.S. Health Care system become the best in the world? N Engl J Med 377(10):901–904. https://doi.org/10.1056/NEJMp1708704[publishedOnlineFirst:2017/07/15]
Auspitz M, Cleghorn MC, Tse A et al (2015) Understanding quality issues in your surgical department: comparing the ACS NSQIP with traditional morbidity and mortality conferences in a Canadian Academic Hospital. J Surg Educ 72(6):1272–1277. https://doi.org/10.1016/j.jsurg.2015.05.006[publishedOnlineFirst:2015/06/30]
Byrnes J (2016) Winning at quality and safety: do you need a chief quality officer? J Healthc Manag 61(6):391–395. https://doi.org/10.1097/00115514-201611000-00003[publishedOnlineFirst:2016/01/01]
Cram P, Girotra S, Matelski J et al (2020) Utilization of advanced cardiovascular therapies in the United States and Canada: an observational study of New York and Ontario administrative data. Circ Cardiovasc Qual Outcomes 13(1):e006037-e6137. https://doi.org/10.1161/CIRCOUTCOMES.119.006037[publishedOnlineFirst:2020/01/20]
Davis C, Rhodes DJ (1988) The impact of DRGs on the cost and quality of health care in the United States. Health Policy 9(2):117–131. https://doi.org/10.1016/0168-8510(88)90029-2[publishedOnlineFirst:1987/12/11]
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
See Table 2
Appendix 2
See Table 3
Appendix 3
See Table
Rights and permissions
About this article
Cite this article
Cram, P., Cohen, M.E., Ko, C. et al. Surgical Outcomes in Canada and the United States: An Analysis of the ACS-NSQIP Clinical Registry. World J Surg 46, 1039–1050 (2022). https://doi.org/10.1007/s00268-022-06444-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06444-w