Abstract
Background
According to the common tenet, tumour progression is a chronological process starting with lymphatic invasion. In this respect, the meaning of bone marrow micrometastases (BMM) in patients with lymph node negative colon cancer (CC) is unclear. This study examines the relationship of isolated tumour cells (ITC) in sentinel lymph nodes (SLN) and BMM in patients in early CC.
Methods
BM aspirates were taken from both pelvic crests and in vivo SLN mapping was done during open oncologic colon resection in patients with stage I and II CC. Stainings were performed with the pancytokeratin markers A45-B/B3 and AE1/AE3 as well as H&E. The correlation between the occurrence of ITC+ and BMM+ and their effects on survival was examined using Cox regression analysis.
Results
In a total of 78 patients with stage I and II CC, 11 patients (14%) were ITC+, 29 patients (37%) BMM+. Of these patients, only two demonstrated simultaneous ITC+ /BMM+. The occurrence of BMM+ was neither associated with ITC+ in standard correlation (kappa = − 0.13 [95% confidence interval [CI] = − 0.4–0.14], p = 0.342) nor univariate (odds ratio [OR] = 0.39, 95%CI:0.07–1.50, p = 0.180) or multivariate (OR = 0.58, 95%CI: 0.09–2.95, p = 0.519) analyses. Combined detection of ITC+ /BMM+ demonstrated the poorest overall (HR = 61.60, 95%CI:17.69–214.52, p = 0.032) and recurrence free survival (HR = 61.60, 95%CI: 17.69–214.5, p = 0.032).
Conclusions
These results indicate that simultaneous and not interdependent presence of very early lymphatic and haematologic tumour spread may be considered as a relevant prognostic risk factor for patients with stage I and II CC, thereby suggesting the possible need to reconsider the common assumptions on tumour spread proposed by the prevalent theory of sequential tumour progression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prognosis of patients with colon cancer is still limited despite improved surgical techniques, guidelines to assure an adequate lymph node yield and multimodal oncological therapy. Patients with node-negative disease (i.e. Union for International Cancer Control (UICC) stage I and II) and absence of risk factors (T4, perforation, bowel obstruction, < 12 LN analysed, poor histologic grade, peritumoral lymphovascular invasion (LVI)) are considered tumour-free after adequate surgery without indication for adjuvant therapy [1, 2]. Nevertheless, a significant number of patients still shows a clearly impaired survival [3, 4], thus suggesting occult tumour dissemination already at the initial histological staging.
According to the prevailing understanding of metastasis development as a sequential progression, tumour cells first spread to local lymph nodes (LN) where they form metastatic deposits and then eventually disseminate to higher tier LN and finally become blood borne with the formation of distant metastasis [5]. Histological staging identifies the earliest LN deposits as either isolated tumour cells (ITC) or micrometastasis [6]. In colon cancer, nodal micrometastases are thereby defined as tumour deposits of 0.2 mm to ≤ 2 mm and are classified as nodal positivity, upstaging tumours to stage III (since the 6th edition of the UICC: pN1(mi)) [7,8,9]. LN with ITC on the other hand are harbouring either single tumour cells or clusters of tumour cells of ≤ 0.2 mm and are considered as negative LN (pN0(i +)) [10]. Despite their small size, ITC have been reported to impact survival in early stage colon cancer [11, 12]. These “occult” metastases are difficult to find with standard histopathological techniques, and it has been demonstrated that sentinel lymph node (SLN) mapping with multilevel sectioning and immunohistochemical staining improves their detection rates [6, 13]. SLN have previously been shown to represent the first draining LN in the hierarchical lymphatic draining system from colon cancer and harbour metastases significantly more often than all other LN in a resected specimen [6, 14,15,16,17]. A more in depth-analysis of the SLN is therefore considered the best way to avoid understaging [18].
Interestingly, a considerable proportion of node negative patients nevertheless are diagnosed with metachronous distant metastases, challenging the hypothesis of sequential progression [19, 20]. In fact, data suggest that a synchronous lymphatic and haematologic spread might be an alternative hypothesis that would put into question much of the current tumour understanding and treatment strategies [21, 22]. It has been suggested that LN metastases serve only as an indicator of increased likelihood of metastasis, but that they are not themselves contributing to the seeding in the sense of a metastatic cascade [5, 23,24,25,26]. In fact, a review on the role of lymphadenectomy in a diversity of solid tumours concluded that lymphadenectomy does not improve overall survival but should be merely conceived as a tool of staging, regional control and as a prognostic indicator [27].
The role of circulating tumour cells in the peripheral blood and disseminated tumour cells, e.g. to the bone marrow (BM), are both considered early manifestations of subsequent overt metastasis and have been researched for many years and in a variety of tumours [28,29,30,31]. Nevertheless, the significance of such tumour cells in the BM in patients with node-negative colon cancer is not known and the very early cascade of tumour cell spread to LN and the BM remains unclear.
With this study, we wanted to investigate the prognostic relevance of early tumour cell presence in the first draining LN and tumour cells in the BM in patients with non-metastatic and node-negative colon cancer and the respective interdependent relationship in order to evaluate their respective prognostic impact, thereby analysing suggested evidence regarding early sequential or simultaneous tumour progression.
Patients and methods
Study settings
The here included patients represent a subgroup analysis of a prospective multicenter study (NCT00826579). More precisely, it is an analysis of the node-negative patients [32]. Node positive patients were excluded to obtain a homogenous group of patients with truly early colon cancer. Studying isolated tumour cells in patients with nodal macrometastases in other lymph nodes possibly would have influenced the results to an unpredictable degree. Nodal micrometastases defined as tumour deposits of 0.2 mm to ≤ 2 mm were thereby considered as positive lymph nodes and accordingly upstaging to stage III (since the 6th edition of the UICC: pN1(mi)) and not considered for this analysis [7,8,9]. A consort diagram is shown in Fig. 1. This study was performed at three academic and university-affiliated hospitals in Switzerland and patients were included from 05/2000 until 12/2006. The mean follow-up period was 6.5 years (IQR 5.3–8.3).
The study protocol was approved by the ethical committees of all participating centres. The inclusion and exclusion criteria for the study population have already been reported [30]. In summary, patients with preoperatively verified colon cancer were eligible for the study. Exclusion criteria were defined as stage IV disease, rectal cancer, history of other solid malignancies, and previous abdominal cancer surgery. Written informed consent was obtained prior to surgery. For the present study, only patients with stage I and II colon cancer were considered. Tumours were staged according to the 6th version of the tumour-node-metastasis (TNM) classification system [7]. Tumours with LN micrometastases (pN1(mi)) were therefore considered as stage III and were not considered for this analysis.
All patients received an open oncologic colon cancer resection. The technical details of SLN mapping and BM aspiration have been reported previously [33, 34]. In short, after induction of general anaesthesia and before the oncologic resection, BM aspirates were taken from both pelvic crests. [30, 34]. Detection of ≥ 1 tumour cells was considered as BMM+.
For the SLN mapping, isosulfan blue was injected in vivo into the subserosa around the tumour. All LN that coloured blue within 10 min were marked as SLN [6, 33]. Five serial sections were then obtained at 3 different levels of each SLN. These were stained with H&E and if H&E was negative, additional immunostainings with the pancytokeratin marker AE1/AE3 (DakoCytomation, Glostrup, Denmark) were performed.
Adjuvant chemotherapy was recommended for stage II patients featuring risk factors (i.e. < 12 LN analysed, T4 tumour, LVI, poor differentiation or perforation) [2]. ITC in the LN (and BMM+) were not deemed an indication for adjuvant chemotherapy. Postoperative surveillance was conducted following national surveillance guidelines [35, 36].
Statistical analyses
Analyses were done by the R statistical software (www.r-project.org). A two-sided p-value < 0.05 was considered statistically significant. Chi-Square statistics were used to analyse proportions and ANOVA tests to analyse continuous variables. The interrelationship of ITC+ and BMM+ was evaluated using Kappa statistics with the 95% confidence intervals [37]. Further, univariable and multivariable logistic regression analyses were conducted to analyse the predictive value of ITC+ for BMM+ and of BMM+ for ITC+. Due to complete and quasi-complete separation (occurrence empty categories), Firth’s correction to the likelihood (penalized maximum likelihood) was used [38, 39]. For logistic regression, p-values were computed by likelihood-ratio-tests and Wald-type confidence intervals were calculated. The impact of ITC+ and BMM+ as prognostic factors for overall and disease-specific survival was evaluated in univariable and multivariable Cox regression analyses. For Cox regression, p-values were calculated by likelihood-ratio-tests and Wald-type confidence intervals were estimated.
Results
In a total of 78 patients with stage I or II colon cancer, in vivo SLN mapping and BM aspiration were successfully performed. Patient demographics and histopathologic tumour data are shown in Table 1.
Overall, 28.2% of tumours were UICC stage I, while 71.8% were stage II. The median number of analysed LN was 23.5 (IQR 19.0–31.0). In 77 patients (98.7%), ≥ 12 LN were retrieved and analysed. In total, 12 patients (15.4%) received adjuvant chemotherapy because of present high risk factors [2] (Table 1).
For further analysis, the population was divided into four groups according to ± ITC and ± BMM status. Demographic information and tumour details of patients in the four groups are shown in Table 1. Overall, 51.3% were ITC− /BMM−, 11.5% of patients showed isolated ITC+ , while 34.6% patients showed BMM+. In two patients (2.5%) ITC+ /BMM+ were identified (Table 1).
Kappa analysis
In Kappa analysis no association between the presence of ITC+ and BMM+ in stage I and II colon cancer patients was observed (kappa = − 0.13, 95%CI = − 0.4–0.14, p = 0.342).
Multivariate Firth’s logistic regression analysis
In uni- and multivariable logistic regression analyses, the presence of BMM+ did not predict the occurrence of ITC in uni- and multivariable analyses (OR = 0.39, 95%CI: 0.07–1.50, p = 0.180 and OR = 0.74, 95%CI: 0.11–3.86, p = 0.730) (Table 2).
Conversely, the presence of ITC+ did not predict the occurrence of BMM+ (OR = 0.39, 95%CI: 0.07–1.50, p = 0.180 and OR = 0.58, 95%CI: 0.09–2.95, p = 0.519) (Table 2).
Higher UICC tumour stage (OR = 10.27, 95%CI:1.10–1727.27, p = 0.039) and present LVI (OR 10.44, 95%CI:1.24–151.56, p = 0.030) were independent predictors for the presence of ITC+ (Table 2).
Right-sided tumour localisation was predictive of BMM+ in univariate and multivariate analyses (compared to tumour localisation in the transverse colon: OR = 0.20, 95%CI:0.03–0.87 and tumour localisation in the left colon: OR 0.29, 95%CI:0.09–0.85, p = 0.023) (Table 2).
Multivariate survival analysis
In univariate and multivariate analyses for OS, no significant association of any of the analysed parameters was found (Table 3).
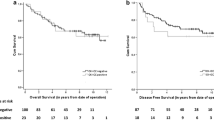
Univariate 5-year survival rates
Five-year survival rate regarding OS was 85.0 (74.6–96.8) for ITC– /BMM–, 76.2 (52.1–100.0) for ITC+ /BMM–, 77.8 (63.6–95.2) for ITC– /BMM+ and 0.0 for ITC+ /BMM+.
Five-year DSS was 85.0 (74.6–96.8) for ITC– /BMM–, 63.5 (37.7–100.0) for ITC+ /BMM–, 74.1 (59.3–92.6) for ITC– /BMM+ and 0.0 for ITC+ /BMM+.
Five-year RFS was 89.5 (80.2–99.8) for ITC– /BMM–, 71.4 (44.7–100.0) for ITC+ /BMM–, 88.3 (76.7–100.0) for ITC– /BMM+ and 0.0 for ITC+ /BMM+.
For ITC+ patients (n = 11) and ITC– patients (n = 67) the OS, DSS and RFS where 62.3 (38.9–99.9) vs. 82.1 (73.4–91.8) (p = 0.401), 51.9 (28.7–93.9) vs. 80.6 (71.7–90.6) (p = 0.277) and 71.4 (44.7–100.0) vs. 89.0 (81.6–97.0) (p = 0.581).
For BMM+ patients (n = 29) and BMM– patients (n = 49) OS, DSS and RFS where 72.4 (57.9–90.7) vs. 83.6 (73.9–94.7) (p = 0.426), 69.0 (54.0–88.0) vs. 81.5 (71.3–93.2) (p = 0.410), 88.6 (77.2–100.0) versus 86.9 (77.7–97.3) (p = 0.645).
Adjusted survival curves
Analysing ITC and BMM as one single factor (ITC– /BMM–, ITC+ /BMM–, ITC– /BMM+, ITC+ /BMM+) instead of fitting them as two independent factors (Table 3) reveals the impact of the simultaneous occurrence of ITC+ and BMM+ despite the low number of patients in this subgroup (n = 2). For OS and RFS, a distinctly worse survival is seen for patients with ITC+ /BMM+ compared to the three other groups (HR = 61.6; 95%CI:17.69–214.52; p = 0.032) (Fig. 2a) and (HR = 61.60; 95%CI:17.69–214.52; p = 0.032) (Fig. 2c). For DSS, no significant difference was observed between the four subgroups (HR = 34.55; 95%CI:10.30–115.85; p = 0.052) (Fig. 2b).
Discussion
The objective of the present study was to investigate the interdependent relationship and respective prognostic relevance of early tumour cell presence in the first draining LN (SLN) and the BM in patients with stage I and II colon cancer, thereby gaining insight into the first steps of tumour cell dissemination. The prevailing doctrine currently is that tumour cell spread occurs in a sequential order, first via LN and later systemically to distant sites. One of the first descriptions of this process was made almost two decades ago in patients with melanoma (incubator hypothesis) [24]. Nevertheless, this study shows that the appearance of ITC in SLN and BMM occurred independent from each other in patients with stage I and II colon cancer, suggesting an early, simultaneous and non-interdependent spread to the LN and the BM. Neither ITC in LN nor BMM are thereby recognised risk factors for patients with colon cancer. Still, we were able to show that patients with a simultaneous spread to both these sites had a significant worse OS and RFS.
According to the current tumour classification systems, patients with micrometastases in LN are considered node-positive while patients with ITC are considered node-negative [7,8,9]. As nodal status distinguishes stage I and II from stage III and therefore divides patients not automatically qualifying for adjuvant chemotherapy from patients routinely receiving chemotherapy, LN status has a huge impact on further oncologic treatment. The distinction of micrometastases and ITC had been introduced in the 6th edition of the TNM classification [7, 40]. However, evidence-based data supporting a cut-off at 0.2 mm are not available. In the meantime, the prognostic importance of ITC has been repeatedly demonstrated, challenging their attribution to node-negativity [11, 12, 15, 16, 41].
ITC detected in SLN might thereby represent the very earliest step of lymphatic tumour spread as SLN have been shown to represent the first draining LN in the hierarchical lymphatic draining system of colon cancer and harbour metastases significantly more often than all other LN [6, 14,15,16,17]. Mapping and in-depth analysis by immunohistochemical stainings of multi-level sections of SLN provides therefore a more accurate staging and triggers through stage migration (Will Rogers phenomenon) more homogenous groups that all show an improved outcome [42].
Analysis of BM in colon cancer patients is not routinely performed. This despite existing evidence that BMM are associated with worse DFS and OS in stage I–III colon cancer [30, 32, 43]. The reports focus on stage I–III colon cancer, leaving the possibility that stage III with macro-metastatic tumour spread to LN has influenced the results by representing an already established and advanced tumour spreading state. Narrowing the analysed population to only stage I and II reveals a more homogenous group possibly representing a similar biological state.
In accordance with the common understanding of tumour spread in colon cancer, stage (UICC stage I vs II) and LVI were predicting factors for ITC+ while BMM+ was only indicated by the tumour site and in particular not by stage or LVI. The correlation of LVI and early tumour spread, i.e. ITC+, supports current practice of assigning those patients to systemic adjuvant therapy [2]. The fact that right sided tumours were associated with BMM+ might help explain why those tumours are generally suspected to have a worse prognosis [44], although we have not observed in our population a difference in outcome in dependence of the tumour localisation.
ITC+ and BMM+ indicate two distinct ways of tumour spread which nevertheless occurred simultaneously even at this early stage. Therefore, the haematologic and prognostic relevant tumour spread in stage I and II colon cancer challenges the general tenet of metastatic tumour spread [5, 45]. Basic science and advances in molecular biology will certainly deepen our yet basic understanding of biology and tumour spread [21, 22, 25, 26, 46, 47]. Furthermore, genetic analysis could facilitate the determination of the origin of BMM and provide additional evidence in support of the theory of early metastatic spread.
Our study has limitations we want to acknowledge. On the one hand, this it is a cohort study and not a randomized clinical trial, so there may be confounding factors that we could not control for. However, patient groups are comparable in terms of baseline characteristics. Second, this analysis is a subset of a larger population, and in some groups only a few patients remained. In particular we underline that only two patients presented with ITC+ /BMM+. It might be that ITC+ /BMM+ combination represents a subgroup that is not seen that often. But as these patients show a distinct worse outcome compared to isolated ITC+ or BMM+ alone, or to no tumour cell spread, further research in the area is needed and should bring additional evidence.
This is, to our knowledge, the first study investigating risk factors for a worse prognosis in node-negative colon cancer patients who underwent SLN mapping and BM analysis. We have thereby been able to find evidence that the simultaneous presence of ITC in SLN and BMM might represent a significant risk factor for a decreased OS and RFS and certainly warrants further investigation.
Conclusions
Our results indicate that the simultaneous and not interdependent presence of ITC in SLN and tumour cells in the BM may be considered as a risk factor for patients with non-metastatic colon cancer.
Our findings suggest that relevant lymphatic and haematologic tumour spread occurs already at such early stages and significantly impairs prognosis, thereby challenging the prevalent theory of sequential tumour progression and proposing the possible need to reconsider the common assumptions on tumour spread. The results further underline the importance of in-depth analysis and assessment of additional risk factors in colon cancer patients like ITC in SLN and tumour cells in the BM.
References
Brenner H, Kloor M, Pox CP (2014) Colorectal cancer. Lancet 383(9927):1490–1502
Benson AB, Schrag D, Somerfield MR et al (2004) American Society of Clinical Oncology recommendations on adjuvant chemotherapy for stage II colon cancer. J Clin Oncol 22(16):3408–3419
Bockelman C, Engelmann BE, Kaprio T et al (2015) Risk of recurrence in patients with colon cancer stage II and III: a systematic review and meta-analysis of recent literature. Acta Oncol 54(1):5–16
Cronin KA, Lake AJ, Scott S et al (2018) Annual report to the Nation on the status of cancer, part I: National cancer statistics. Cancer 124(13):2785–2800
Sleeman J, Schmid A, Thiele W (2009) Tumor lymphatics. Semin Cancer Biol 19(5):285–297
Viehl CT, Guller U, Cecini R et al (2012) Sentinel lymph node procedure leads to upstaging of patients with resectable colon cancer: results of the Swiss prospective, multicenter study sentinel lymph node procedure in colon cancer. Ann Surg Oncol 19(6):1959–1965
Sobin LH, Wittekind C (2002) TNM classification of malignant tumours (UICC), 6th edn. John Wiley & Sons, New Jersey
UICC, I.U.A.C., International Union Against Cancer (2009) TNM classification of malignant tumours, 7th edn. Wiley-Blackwell, West-Sussex
Brierley JD, Wittekind C, International Union Against Cancer (UICC) (2017) TNM classification of malignant tumours, 8th edn. Wiley Blackwell, Oxford
Hermanek P, Hutter RV, Sobin LH, International Union Against Cancer et al (1999) Classification of isolated tumor cells and micrometastasis. Cancer 86(12):2668–2673
Weixler B, Warschkow R, Guller U et al (2016) Isolated tumor cells in stage I & II colon cancer patients are associated with significantly worse disease-free and overall survival. BMC Cancer 16:106
Mescoli C, Albertoni L, Pucciarelli S et al (2012) Isolated tumor cells in regional lymph nodes as relapse predictors in stage I and II colorectal cancer. J Clin Oncol 30(9):965–971
Weixler B, Rickenbacher A, Raptis DA et al (2017) Sentinel lymph node mapping with isosulfan blue or indocyanine green in colon cancer shows comparable results and identifies patients with decreased survival: a prospective single-center trial. World J Surg 41(9):2378–2386. https://doi.org/10.1007/s00268-017-4051-2
Saha S, Sehgal R, Patel M et al (2006) A multicenter trial of sentinel lymph node mapping in colorectal cancer: prognostic implications for nodal staging and recurrence. Am J Surg 191(3):305–310
Stojadinovic A, Nissan A, Protic M et al (2007) Prospective randomized study comparing sentinel lymph node evaluation with standard pathologic evaluation for the staging of colon carcinoma: results from the United States Military Cancer Institute Clinical Trials Group Study GI-01. Ann Surg 245(6):846–857
van der Pas MHGM, Meijer S, Hoekstra OS et al (2011) Sentinel-lymph-node procedure in colon and rectal cancer: a systematic review and meta-analysis. Lancet Oncol 12(6):540–550
van der Zaag ES, Bouma WH, Tanis PJ et al (2012) Systematic review of sentinel lymph node mapping procedure in colorectal cancer. Ann Surg Oncol 19(11):3449–3459
Bembenek A, Schneider U, Gretschel S et al (2005) Detection of lymph node micrometastases and isolated tumor cells in sentinel and nonsentinel lymph nodes of colon cancer patients. World J Surg 29(9):1172–1175. https://doi.org/10.1007/s00268-005-0094-x
Riihimaki M, Hemminki A, Sundquist J et al (2016) Patterns of metastasis in colon and rectal cancer. Sci Rep 6:29765
van Gestel YR, de Hingh IH, van Herk-Sukel MP et al (2014) Patterns of metachronous metastases after curative treatment of colorectal cancer. Cancer Epidemiol 38(4):448–454
Naxerova K, Reiter JG, Brachtel E et al (2017) Origins of lymphatic and distant metastases in human colorectal cancer. Science 357(6346):55–60
Nagtegaal ID, Schmoll HJ (2017) Colorectal cancer: What is the role of lymph node metastases in the progression of colorectal cancer? Nat Rev Gastroenterol Hepatol 14(11):633–634
Cady B (1984) Lymph node metastases: indicators, but not governors of survival. Arch Surg 119(9):1067–1072
Morton DL, Hoon DS, Cochran AJ et al (2003) Lymphatic mapping and sentinel lymphadenectomy for early-stage melanoma: therapeutic utility and implications of nodal microanatomy and molecular staging for improving the accuracy of detection of nodal micrometastases. Ann Surg 238(4):538–549
Sleeman JP, Nazarenko I, Thiele W (2011) Do all roads lead to Rome? Routes to metastasis development. Int J Cancer 128(11):2511–2526
Sleeman JP, Cady B, Pantel K (2012) The connectivity of lymphogenous and hematogenous tumor cell dissemination: biological insights and clinical implications. Clin Exp Metastasis 29(7):737–746
Gervasoni JE Jr, Sbayi S, Cady B (2007) Role of lymphadenectomy in surgical treatment of solid tumors: an update on the clinical data. Ann Surg Oncol 14(9):2443–2462
Cristofanilli M, Budd GT, Ellis MJ et al (2004) Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N Engl J Med 351(8):781–791
Braun S, Vogl FD, Naume B et al (2005) A pooled analysis of bone marrow micrometastasis in breast cancer. N Engl J Med 353(8):793–802
Viehl CT, Weixler B, Guller U et al (2017) Presence of bone marrow micro-metastases in stage I-III colon cancer patients is associated with worse disease-free and overall survival. Cancer Med 6(5):918–927
Rahbari NN, Aigner M, Thorlund K et al (2010) Meta-analysis shows that detection of circulating tumor cells indicates poor prognosis in patients with colorectal cancer. Gastroenterology 138(5):1714–1726
Weixler B, Viehl CT, Warschkow R et al (2017) Comparative analysis of tumor cell dissemination to the sentinel lymph nodes and to the bone marrow in patients with nonmetastasized colon cancer: a prospective multicenter study. JAMA Surg 152(10):912–920
Viehl CT, Hamel CT, Marti WR et al (2003) Identification of sentinel lymph nodes in colon cancer depends on the amount of dye injected relative to tumor size. World J Surg 27(12):1285–1290. https://doi.org/10.1007/s00268-003-7086-5
Langer I, Guller U, Worni M et al (2014) Bone marrow micrometastases do not impact disease-free and overall survival in early stage sentinel lymph node-negative breast cancer patients. Ann Surg Oncol 21(2):401–407
SGGSSG, Konsensus-Empfehlung zur Nachsorge nach kurativ operiertem kolorektalem Karzinom 2014 (updated 02.10.2014). https://sggssg.ch/empfehlungen/
Rueff J, Weixler B, Viehl CT et al (2020) Improved quality of colon cancer surveillance after implementation of a personalized surveillance schedule. J Surg Oncol 122:529–537
Watson PF, Petrie A (2010) Method agreement analysis: a review of correct methodology. Theriogenology 73(9):1167–1179
Firth D (1993) Bias reduction of maximum likelihood estimates. Biometrika 80(1):27–38
Heinze G, Schemper M (2002) A solution to the problem of separation in logistic regression. Stat Med 21(16):2409–2419
Sobin LH (2003) TNM, sixth edition: new developments in general concepts and rules. Semin Surg Oncol 21(1):19–22
Faerden AE, Sjo OH, Bukholm IR et al (2011) Lymph node micrometastases and isolated tumor cells influence survival in stage I and II colon cancer. Dis Colon Rectum 54(2):200–206
Feinstein AR, Sosin DM, Wells CK (1985) The Will Rogers phenomenon: stage migration and new diagnostic techniques as a source of misleading statistics for survival in cancer. N Engl J Med 312(25):1604–1608
Lindemann F, Schlimok G, Dirschedl P et al (1992) Prognostic significance of micrometastatic tumour cells in bone marrow of colorectal cancer patients. Lancet 340(8821):685–689
Yahagi M, Okabayashi K, Hasegawa H et al (2016) The worse prognosis of right-sided compared with left-sided colon cancers: a systematic review and meta-analysis. J Gastrointest Surg 20(3):648–655
Hellman S (1994) Karnofsky memorial lecture. Natural history of small breast cancers. J Clin Oncol 12(10):2229–2234
Ubellacker JM, Tasdogan A, Ramesh V et al (2020) Lymph protects metastasizing melanoma cells from ferroptosis. Nature 585(7823):113–118
Klein CA (2009) Parallel progression of primary tumours and metastases. Nat Rev Cancer 9(4):302–312
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ramser, M., Warschkow, R., Viehl, C.T. et al. The Simultaneous Presence of Isolated Tumour Cells and Bone Marrow Micrometastases in Stage I and II Colon Cancer—Challenging the Theory of a Chronological Pathway of Tumour Cell Dissemination. World J Surg 46, 680–689 (2022). https://doi.org/10.1007/s00268-021-06399-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06399-4