Abstract
Background
To construct a modified tumor-node-metastasis (TNM) staging system for stage I-III colon cancer patients with lymph nodes examined (LNE) < 12.
Methods
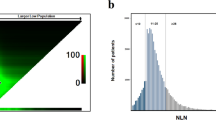
The clinicopathological and survival data of 3870 stage I-III colon cancer patients with LNE < 12 from the Surveillance, Epidemiology, and End Results (SEER) database between 2010 and 2015 (development cohort) and 126 stage I-III patients with LNE < 12 from the Second Affiliated Hospital of Harbin Medical University between 2011 and 2015 (validation cohort) were identified. The optimal stratification of LNR for cancer-specific survival (CSS) was achieved using X-tile software. The predictive accuracy of the modified stage (mStage) was determined by the concordance index (C-index).
Results
The modified N stage (mN stage) was built based on the LNR (mN0: LNR = 0, mN1: 0 < LNR < 0.4 or cancer nodule formation and mN2: 0.4 ≤ LNR ≤ 1). Preferable C-indices could be found for mStage compared with TNM stage in both development (0.750 vs 0.727) and validation cohorts (0.682 vs 0.646). Besides, patients with mStage A and B diseases could not benefit from adjuvant chemotherapy, while in patients with mStage C-F diseases, those receiving radical surgery plus adjuvant chemotherapy presented better CSS than those with radical surgery alone.
Conclusions
The mStage system could predict the prognosis of colon cancer patients with LNE < 12 accurately and showed superior predictive power compared with conventional TNM staging system. Moreover, adjuvant chemotherapy might play inequable roles in patients with different mStage diseases.






Similar content being viewed by others
Data availability
The study data of development cohort are available from the SEER database.
Abbreviations
- LNR:
-
Lymph node ratio
- LNE:
-
Lymph nodes examined
- TNM:
-
Tumor-node-metastasis
- mStage:
-
Modified stage
- SEER:
-
Surveillance, epidemiology, and end results
- CSS:
-
Cancer-specific survival
- ROC:
-
Receiver operating characteristic
- AJCC:
-
American joint committee on cancer
- AUC:
-
Area under the receiver operating characteristic curve
- CI:
-
Confidence intervals
References
Siegel R, Miller K, Goding Sauer A et al (2020) Colorectal cancer statistics, 2020. CA Cancer J Clin 70:145–64
Benson A, Venook A, Al-Hawary M et al (2018) NCCN guidelines insights: colon cancer, version 2.2018. J Natl Compr Cancer Netw JNCCN 16:359–69
Compton C, Greene F (2004) The staging of colorectal cancer: 2004 and beyond. CA Cancer J Clin 54:295–308
Polignano F, Henderson N, Alishahi S et al (2006) Laparoscopic colectomy for cancer and adequate lymphadenectomy: association between survival and number of lymph nodes. Surg Endosc 20:996–997
Wang Y, Guan X, Zhang Y et al (2020) A preoperative risk prediction model for lymph node examination of stage i-iii colon cancer patients: a population-based study. J Cancer 11:3303–3309
Guan X, Wang Y, Hu H et al (2018) Reconsideration of the optimal minimum lymph node count for young colon cancer patients: a population-based study. BMC Cancer 18:623
Dorrance H, Docherty G, O’Dwyer P (2000) Effect of surgeon specialty interest on patient outcome after potentially curative colorectal cancer surgery. Dis Colon Rectum 43:492–498
Nathan H, Shore A, Anders R et al (2011) Variation in lymph node assessment after colon cancer resection: patient, surgeon, pathologist, or hospital? J Gastrointest Surg Off J Soc Surg Aliment Tract 15:471–479
Ahmadi O, Stringer M, Black M et al (2015) Clinico-pathological factors influencing lymph node yield in colorectal cancer and impact on survival: analysis of New Zealand cancer registry data. J Surg Oncol 111:451–458
Berger A, Sigurdson E, LeVoyer T et al (2005) Colon cancer survival is associated with decreasing ratio of metastatic to examined lymph nodes. J Clin Oncol Off J Am Soc Clin Oncol 23:8706–8712
Jiang K, Zhu Y, Liu Y et al (2014) Lymph node ratio as an independent prognostic indicator in stage III colorectal cancer: especially for fewer than 12 lymph nodes examined. Tumour Biol J Int Soc Oncodevelopmental Biol Med 35:11685–11690
Costi R, Beggi F, Reggiani V et al (2014) Lymph node ratio improves TNM and Astler-Coller’s assessment of colorectal cancer prognosis: an analysis of 761 node positive cases. J Gastrointest Surg Off J Soc Surg Aliment Tract 18:1824–1836
Kwon T, Choi S, Lee Y et al (2016) Novel methods of lymph node evaluation for predicting the prognosis of colorectal cancer patients with inadequate lymph node harvest. Cancer Res Treat Off J Korean Cancer Assoc 48:216–224
Rausei S, Iovino D, Tenconi S et al (2013) Impact of lymph node ratio on survival of colorectal cancer patients. Int J Surg. https://doi.org/10.1016/S1743-9191(13)60026-6
Moug S, Saldanha J, McGregor J et al (2009) Positive lymph node retrieval ratio optimises patient staging in colorectal cancer. Br J Cancer 100:1530–1533
Hankey B, Ries L, Edwards B (1999) The surveillance, epidemiology, and end results program: a national resource. Cancer Epidemiol Biomarker Prevent Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol 8:1117–1121
Camp R, Dolled-Filhart M, Rimm D (2004) X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res An Off J Am Assoc Cancer Res 10:7252–7259
Huang B, Feng Y, Ni M et al (2018) Heterogeneous survival between stage IIA and stage IIIA colon cancer when different numbers of lymph nodes are harvested. ANZ J Surg 88:316–321
Lv Y, Feng Q, Lin S et al (2019) Exploration of exact significance of lymph node ratio and construction of a novel stage in colon cancer with no distant metastasis. Cancer Manag Res 11:6841–6854
Huang L, Yang T, Yang L et al (2020) Clinical efficacy of adjuvant chemotherapy in the treatment of pT4 stage II colorectal cancer with defective mismatch repair status: a protocol for systematic review and meta-analysis. Medicine 99:e20693
Jalaeikhoo H, Zokaasadi M, Khajeh-Mehrizi A et al (2019) Effectiveness of adjuvant chemotherapy in patients with stage II colorectal cancer: a multicenter retrospective study. J Res Med Sci 24:39
Acknowledgements
The authors acknowledge the efforts of the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER database.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
This study was approved by the Second Affiliated Hospital of Harbin Medical University and Zhejiang Cancer Hospital. The study used de-identified data and adhered to World Medical Association’s Declaration of Helsinki for Ethical Human Research. The informed consent was not required according to personal identifying information was not included.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, H., Liu, Y., Wang, C. et al. A Modified Tumor-Node-Metastasis Staging System for Colon Cancer Patients with Fewer than Twelve Lymph Nodes Examined. World J Surg 45, 2601–2609 (2021). https://doi.org/10.1007/s00268-021-06141-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06141-0