Abstract
Background
Prognosis assessment of node-positive colorectal cancer patients by Astler-Coller (AC) and TNM classifications is suboptimal. Recently, several versions of lymph node ratio (LNR; ratio metastatic/examined nodes) have been proposed but are still mostly unused.
Methods
The prognostic value of several criteria, including LNR (two classes—LNR1 and LNR2—identified by a 15 % cut-off) was studied in 761 consecutive patients, from 2000 through 2010. The relationships between total examined nodes, N, T and LNR were also analysed. LNR1 and LNR2 patients’ survival was analysed within AC and TNM subgroups, and then coupled with them.
Results
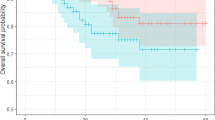
Age, tumour location and LNR are independent factors predicting survival. The relationships between LNR, N stage and T stage with examined nodes suggest confusing factors. LNR allows for identification of subgroups with different survival within AC and TNM classifications (p < 0.0001). Patients with LNR class discordant from AC stage (LNR1-C2 and LNR2-C1) have a similar 5-year survival (54 and 57 %, respectively). LNR2 and TNM stage IIIC define a poor 5-year prognosis (33 %).
Conclusions
LNR is a powerful prognosis predictor, easily integrated with TNM and AC classifications to improve prognosis assessment and facilitate clinical use. Possible confusing factors should be considered in future studies.





Similar content being viewed by others
References
Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, Forman D, Bray F. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries in 2012. Eur J Cancer 2013; 49:1374–1403
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin 2013; 63:11–30
Lykke J, Roikjaer O, Jess P; Danish Colorectal Cancer Group. The relation between lymph node status and survival in stage I–III colon cancer: results from a prospective nationwide cohort study. Colorectal Dis. 2013; 15:559–565
Lan YT, Yang SH, Chang SC, Liang WY, Li AF, Wang HS, Jiang JK, Chen WS, Lin TC, Lin JK. Analysis of the seventh edition of American Joint Committee on colon cancer staging. Int J Colorectal Dis 2012; 27:657–6663
Sjo OH, Merok MA, Svindland A, Nesbakken A. Prognostic impact of lymph node harvest and lymph node ratio in patients with colon cancer. Dis Colon Rectum 2012; 55:307–315
O'Connell JB, Maggard MA, Ko CY. Colon cancer survival rates with the New American Joint Committee on Cancer Sixth Edition Staging. J Natl Cancer Inst. 2004; 96:1420–1425
Dukes CE, Bussey HJ. The spread of rectal cancer and its effect on prognosis. Br J Cancer. 1958; 12:309–320
Fleming ID, Cooper JS, Henson DE et al. American Joint Committee on Cancer. AJCC cancer staging manual, 5th edition. Philadelphia: Lippincott-Raven, 1997
Greene FL, Page DL, Fleming ID et al. American Joint Committee on Cancer. AJCC cancer staging manual, 6th edition. New York: Springer-Verlag, 2002
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. American Joint Committee on Cancer. AJCC cancer staging manual, 7th edition. New York: Springer, 2010
Akagi Y, Adachi Y, Ohchi T, Kinugasa T, Shirouzu K. Prognostic impact of lymphatic invasion of colorectal cancer: a single-center analysis of 1,616 patients over 24 years. Anticancer Res 2013; 33:2965–2970
Sato T, Ueno H, Mochizuki H, Shinto E, Hashiguchi Y, Kajiwara Y, Shimazaki H, Hase K. Objective criteria for the grading of venous invasion in colorectal cancer Am J Surg Pathol 2010; 34:454–462
De la Chapelle A, Hampel H. Clinical relevance of microsatellite instability in colorectal cancer. J Clin Oncol 2010; 28:3380–3387
Walther A, Houlston R, Tomlinson I. Association between chromosomal instability and prognosis in colorectal cancer: a meta-analysis. Gut 2008; 57:941–950
Eklöf V, Wikberg ML, Edin S, Dahlin AM, Jonsson BA, Öberg Å, Rutegård J, Palmqvist R. The prognostic role of KRAS, BRAF, PIK3CA and PTEN in colorectal cancer. Br J Cancer 2013; 108:2153–2163
Cushman-Vokoun AM, Stover DG, Zhao Z, Koehler EA, Berlin JD, Vnencak-Jones CL. Clinical utility of KRAS and BRAF mutations in a cohort of patients with colorectal neoplasms submitted for microsatellite instability testing. Clin Colorectal Cancer 2013; 12:168–178
Hari DM, Leung AM, Lee JH, Sim MS, Vuong B, Chiu CG, Bilchik AJ. AJCC Cancer Staging Manual 7th edition criteria for colon cancer: do the complex modifications improve prognostic assessment? J Am Coll Surg 2013; 217:181–190
Prandi M, Lionetto R, Bini A, Francioni G, Accarpio G, Anfossi A, Ballario E, Becchi G, Bonilauri S, Carobbi A, Cavaliere P, Garcea D, Giuliani L, Morziani E, Mosca F, Mussa A, Pasqualini M, Poddie D, Tonetti F, Zardo L, Rosso R. Prognostic evaluation of stage B colon cancer patients is improved by an adequate lymphadenectomy: results of a secondary analysis of a large scale adjuvant trial. Ann Surg 2002; 235:458–463
Caplin S, Cerottini JP, Bosman FT, Constanda MT, Givel JC. Forpatients with Dukes’ B (TNM Stage II) colorectal carcinoma,examination of six or fewer lymph nodes is related to poor prognosis. Cancer 1998; 83:666–672
Fielding LP, Arsenault PA, Chapuis PH, Dent O, Gathright B, Hardcastle JD, Hermanek P, Jass JR, Newland RC. Clinicopathological staging for colorectal cancer: an International Documentation System (IDS) and an International Comprehensive Anatomical Terminology (ICAT). J Gastroenterol Hepatol 1991; 6:325–344
Wong JH, Severino R, Honnebier MB, Tom P, Namiki TS. Number of nodes examined and staging accuracy in colorectal carcinoma. J Clin Oncol 1999; 17:2896–2900
Goldstein NS, Sanford W, Coffey M, Layfield LJ.Lymph node recovery from colorectal resection specimens removed for adenocarcinoma: Trends over time and a recommendation for a minimum number of lymph nodes to be removed. Am J Clin Pathol 1996; 106:209–216
Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ, Haller DG. Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol 2003; 21:2912–2919
Inoue K, Nakane Y, Iiyama H, Sato M, Kanbara T, Nakai K, Okumura S, Yamamichi K, Hioki K. The superiority of ratio-based lymph node staging in gastric carcinoma. Ann Surg Oncol 2002; 9:27–34
Riediger H, Keck T, Wellner U, zur Hausen A, Adam U, Hopt UT, Makowiec F. The limph node ratio is the strongest prognostic factor after resection of pancreatic cancer. J Gastrointest Surg 2009; 13:1337–1344
Megale Costa LJ, Soares HP, Gaspar HA, Trujillo LG, Santi PX, Pereira RS, de Santana TL, Pinto FN, del Giglio A. Ratio between positive lymph nodes and total dissected axillaries lymph nodes as an independent prognostic factor for disease-free survival in patients with breast cancer. Am J Clin Oncol 2004; 27:304–306
Herr HW. Superiority of ratio based lymph node staging for bladder cancer. J Urol 2003; 169:943–945
Berger AC, Sigurdson ER, LeVoyer T, Hanlon A, Mayer RJ, Macdonald JS, Catalano PJ, Haller DG. Colon cancer survival is associated with decreasing ratio of metastatic to examined lymph nodes. J Clin Oncol 2005; 23:8706–8712
Elias E, Mukherji D, Faraj W, Khalife M, Dimassi H, Eloubeidi M, Hattoum H, Abou-Alfa GK, Saleh A, Shamseddine A. Lymph-node ratio is an independent prognostic factor in patients with stage III colorectal cancer: a retrospective study from the Middle East. World J Surg Oncol 2012; 10:63
Rosenberg R, Friederichs J, Schuster T, Gertler R, Maak M, Becker K, Grebner A, Ulm K, Höfler H, Nekarda H, Siewert JR. Prognosis of patients with colorectal cancer is associated with lymph node ratio: a single-center analysis of 3,026 patients over a 25-year time period. Ann Surg 2008; 248:968–978
Vather R, Sammour T, Kahokehr A, Connolly AB, Hill AG. Lymph node evaluation and long-term survival in stage II and stage III colon cancer: a national study. Ann Surg Oncol 2009; 16:585–593
Kritsanasakul A, Boonpipattanapong T, Wanitsuwan W, Phukaoloun M, Prechawittayakul P, Sangkhathat S. Impact of Lymph Node Retrieval on Surgical Outcomes in Colorectal Cancers. J Surg Oncol 2012; 106:238–242
Hong KD, Lee SI, Moon HY. Lymph node ratio as determined by the 7th edition of the American Joint Committee on Cancer staging system predicts survival in stage III colon cancer. J Surg Oncol 2011; 103:406–410
Ceelen W, Van Nieuwenhove Y, Pattyn P. Prognostic Value of the Lymph Node Ratio in Stage III Colorectal Cancer: A Systematic Review. Ann Surg Oncol 2010; 17:2847–2855
Faiclough DL Ed. Analysis of quality of life studies in clinical trials, 2nd edition. New York: Chapman & Hall/CRC-Taylor and Francis Group, 2010
Pietra N, Sarli L, Costi R, Ouchemi C, Grattarola M, Peracchia A. Role of follow-up in management of local recurrences of colorectal cancer: a prospective, randomized study. Dis Colon Rectum 1998; 41:1127–1133
Gao P, Song YX, Wang ZN, Xu YY, Tong LL, Zhu JL, Tang QC, Xu HM. Integrated ratio of metastatic to examined lymph nodes and number of metastatic lymph nodes into the AJCC Staging System for Colon Cancer. PLoS One 2012; 7:e35021
Wang JP, Hassett JM, Dayton MT, Kulaylat MN. Lymph node ratio: role in the staging of node-positive colon cancer. Ann Surg Oncol 2008; 15:1600–1608
Derwinger K, Carlsson G, Gustavsson B. A study of lymph node ratio as a prognostic marker in colon cancer. Eur J Surg Oncol 2008; 34:771–775
Lee HY, Choi H, Park K, Shin J, Kwon H, Roh M, Kim C. Prognostic Significance of Metastatic Lymph Node Ratio in Node-Positive Colon Carcinoma. Annals of Surgical Oncology 2007; 14:1712–1717
Schumacher P, Dineen S, Barnett C, Fleming J, Anthony T. The metastatic lymph node ratio predicts survival in colon cancer. Am J Surg 2007; 194:827–832
Peschaud F, Benoist S, Julie C, et. al. The ratio of metastatic to examined lymph nodes is a powerful independent prognostic factor in rectal cancer. Ann Surg 2008; 248:1067–1073
Thomas M, Biswas S, Mohamed F, Chandrakumaran K, Jha M, Wilson R. Dukes C colorectal cancer: is the metastatic lymph node ratio important? Int J Colorectal Dis 2012; 27:309–317
Lee SD, Kim TH, Kim DY, Baek JY, Kim SY, Chang HJ, Park SC, Park JW, Oh JH, Jung KH. Lymph node ratio is an independent prognostic factor in patients with rectal cancer treated with preoperative chemoradiotherapy and curative resection. Eur J Surg Oncol 2012; 38:478–483
Park HC. Clinical significance of the metastatic lymph-node ratio in rectal cancer. Ann Coloproctol 2013; 29:89–90
De Ridder M, Vinh-Hung V, Van Nieuwenhove Y, Hoorens A, Sermeus A, Storme G. Prognostic value of the lymph node ratio in node positive colon cancer. Gut 2006; 55:1681
Schiffmann L, Eiken AK, Gock M, Klar E. Is the lymph node ratio superior to the Union for International Cancer Control (UICC) TNM system in prognosis of colon cancer? World J Surg Oncol 2013; 11:79
Tepper JE, O'Connell MJ, Niedzwiecki D, et al. Impact of number of nodes retrieved on outcome in patients with rectal cancer. J Clin Oncol 2001; 19:157–163
Feinstein AR, Sosin DM, Wells CK. The Will Rogers phenomenon. Stage migration and new diagnostic techniques as a source of misleading statistics for survival in cancer. N Engl J Med 1985; 312:1604–1608
Shahrier M, Ahnen DJ. Colorectal cancer survival in Europe: the Will Rogers phenomenon revisited. Gut 2000; 47:463–464
George S, Primrose J, Talbot R, Smith J, Mullee M, Bailey D, du Boulay C, Jordan H; Wessex Colorectal Cancer Audit Working Group. Will Rogers revisited: prospective observational study of survival of 3592 patients with colorectal cancer according to number of nodes examined by pathologists. Br J Cancer 2006; 95:841–847
Moertel CG, Fleming TR, Macdonald JS, Haller DG, Laurie JA, Goodman PJ, Ungerleider JS, Emerson WA, Tormey DC, Glick JH, Veeder MH, Mailliard JA. Levamisole and fluorouracil for adjuvant therapy of resected colon carcinoma. N Engl J Med 1990; 322:352–358
André T, Boni C, Mounedji-Boudiaf L, Navarro M, Tabernero J, Hickish T, Topham C, Zaninelli M, Clingan P, Bridgewater J, Tabah-Fisch I, de Gramont A. Multicenter International Study of Oxaliplatin/5-Fluorouracil/Leucovorin in the Adjuvant Treatment of Colon Cancer (MOSAIC) Investigators. Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med 2004; 350:2343–2351
André T, Boni C, Navarro M, Tabernero J, Hickish T, Topham C, Bonetti A, Clingan P, Bridgewater J, Rivera F, de Gramont A. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol 2009; 27:3109–3116
Haller DG, Tabernero J, Maroun J, de Braud F, Price T, Van Cutsem E, Hill M, Gilberg F, Rittweger K, Schmoll HJ. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol 2011; 29:1465–1471
de Gramont A, Van Cutsem E, Schmoll HJ, Tabernero J, Clarke S, Moore MJ, Cunningham D, Cartwright TH, Hecht JR, Rivera F, Im SA, Bodoky G, Salazar R, Maindrault-Goebel F, Shacham-Shmueli E, Bajetta E, Makrutzki M, Shang A, André T, Hoff PM. Bevacizumab plus oxaliplatin-based chemotherapy as adjuvant treatment for colon cancer (AVANT): a phase 3 randomised controlled trial. Lancet Oncol 2012; 13:1225–1233
Peng J, Xu Y, Guan Z, Zhu J, Wang M, Cai G, Sheng W, Cai S. Prognostic significance of the metastatic lymph node ratio in node-positive rectal cancer. Ann Surg Oncol 2008; 15:3118–3123
Moug SJ, McColl G, Lloyd SM, Wilson G, Saldanha JD, Diament RH. Comparison of positive lymph node ratio with an inflammation-based prognostic score in colorectal cancer. Br J Surg 2011; 98:282–286
Acknowledgments
The authors thank Dr. Luca Ampollini (Clinica di Chirurgia Toracica, Dipartimento di Scienze Chirurgiche, Università degli Studi di Parma), Dr. Francesco Bozzani (Registro Tumori, Unità Operativa di Oncologia Medica, Azienda Ospedaliero-Universitaria di Parma), Dr. Pier Luigi Losardo (Servizio di Radioterapia, Dipartimento Onco-Ematologico Internistico, Azienda Ospedaliero-Universitaria di Parma) and Dr. Caterina Ghetti (Servizio di Fisica Sanitaria, Azienda Ospedaliera di Parma) for their precious contribution.
Conflict of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Costi, R., Beggi, F., Reggiani, V. et al. Lymph Node Ratio Improves TNM and Astler-Coller’s Assessment of Colorectal Cancer Prognosis: an Analysis of 761 Node Positive Cases. J Gastrointest Surg 18, 1824–1836 (2014). https://doi.org/10.1007/s11605-014-2591-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2591-4