Abstract
Background
Timely treatment for colorectal cancer (CRC) is a quality indicator in oncological care. However, patients with CRC might benefit more from preoperative optimization rather than rapid treatment initiation. The objectives of this study are (1) to determine the definition of the CRC treatment interval, (2) to study international recommendations regarding this interval and (3) to study whether length of the interval is associated with outcome.
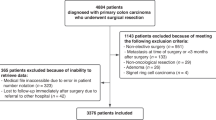
Methods
We performed a systematic search of the literature in June 2020 through MEDLINE, EMBASE and Cochrane databases, complemented with a web search and a survey among colorectal surgeons worldwide. Full-text papers including subjects with CRC and a description of the treatment interval were included.
Results
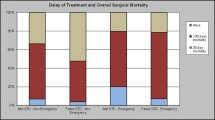
Definition of the treatment interval varies widely in published studies, especially due to different starting points of the interval. Date of diagnosis is often used as start of the interval, determined with date of pathological confirmation. The end of the interval is rather consistently determined with date of initiation of any primary treatment. Recommendations on the timeline of the treatment interval range between and within countries from two weeks between decision to treat and surgery, to treatment within seven weeks after pathological diagnosis. Finally, there is no decisive evidence that a longer treatment interval is associated with worse outcome.
Conclusions
The interval from diagnosis to treatment for CRC treatment could be used for prehabilitation to benefit patient recovery. It may be that this strategy is more beneficial than urgently proceeding with treatment.

Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Collins I, Naidoo J, Rowley S, Reynolds JV, Kennedy MJ (2009) Waiting times for access, diagnosis and treatment in a cancer centre. Ir Med J 102(9):279–282
Roland CL, Schwarz RE, Tong L et al (2013) Is timing to delivery of treatment a reliable measure of quality of care for patients with colorectal adenocarcinoma? Surgery 154(3):421–428
Leong KJ, Chapman MAS (2017) Current data about the benefit of prehabilitation for colorectal cancer patients undergoing surgery are not sufficient to alter the NHS cancer waiting targets. Colorectal Dis 19(6):522–524
Trickett JP, Donaldson DR, Bearn PE, Scott HJ, Hassall AC (2004) A study on the routes of referral for patients with colorectal cancer and its affect on the time to surgery and pathological stage. Colorectal Dis 6(6):428–431
Flemming JA, Nanji S, Wei X, Webber C, Groome P, Booth CM (2017) Association between the time to surgery and survival among patients with colon cancer: a population-based study. Eur J Surg Oncol 43(8):1447–1455
Hangaard Hansen C, Gogenur M, Tvilling Madsen M, Gogenur I (2018) The effect of time from diagnosis to surgery on oncological outcomes in patients undergoing surgery for colon cancer: a systematic review. Eur J Surg Oncol 44(10):1479–1485
Minnella EM, Bousquet-Dion G, Awasthi R, Scheede-Bergdahl C, Carli F (2017) Multimodal prehabilitation improves functional capacity before and after colorectal surgery for cancer: a five-year research experience. Acta Oncol 56(2):295–300
Heger P, Probst P, Wiskemann J, Steindorf K, Diener MK, Mihaljevic AL (2019) A systematic review and meta-analysis of physical exercise prehabilitation in major abdominal surgery (PROSPERO 2017 CRD42017080366). J Gastrointest Surg. https://doi.org/10.1007/s11605-019-04287-w
West MA, Astin R, Moyses HE et al (2019) Exercise prehabilitation may lead to augmented tumor regression following neoadjuvant chemoradiotherapy in locally advanced rectal cancer. Acta Oncol 58(5):588–595
Barberan-Garcia A, Ubre M, Roca J et al (2018) Personalised prehabilitation in high-risk patients undergoing elective major abdominal surgery: a randomized blinded controlled trial. Ann Surg 267(1):50–56
Trepanier M, Minnella EM, Paradis T et al (2019) Improved disease-free survival after prehabilitation for colorectal cancer surgery. Ann Surg. https://doi.org/10.1097/SLA.0000000000003465
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62(10):1
European network of cancer registries—call for data. https://www.encr.eu/sites/default/files/pdf/2015_ENCR_JRC_Call_for_Data_Version_1_1.pdf. Updated 2015. Accessed 19 Sep 2019
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Roder D, Karapetis CS, Olver I et al (2019) Time from diagnosis to treatment of colorectal cancer in a south australian clinical registry cohort: How it varies and relates to survival. BMJ Open 9(9):e031421-031421
National definitions for elective surgery urgency categories—Australia. https://www.aihw.gov.au/reports/hospitals/national-definitions-for-elective-surgery-urgency/contents/table-of-contents. Updated 2013. Accessed 23 July 2020
Wanis KN, Patel SVB, Brackstone M (2017) Do moderate surgical treatment delays influence survival in colon cancer? Dis Colon Rectum 60(12):1241–1249
Cancer care Ontario expert panel report. https://www.cancercareontario.ca/en/content/target-wait-times-cancer-surgery-ontario, http://waittimes.alberta.ca/AWTRInfoPage.jsp?pageID=32. Updated 2006. Accessed 18 Sep 2019
Bardell T, Belliveau P, Kong W, Mackillop WJ (2006) Waiting times for cancer surgery in ontario: 1984–2000. Clin Oncol (R Coll Radiol) 18(5):401–409
Simunovic M, Gagliardi A, McCready D, Coates A, Levine M, DePetrillo D (2001) A snapshot of waiting times for cancer surgery provided by surgeons affiliated with regional cancer centres in ontario. CMAJ 165(4):421–425
Simunovic M, Rempel E, Theriault ME et al (2009) Influence of delays to nonemergent colon cancer surgery on operative mortality, disease-specific survival and overall survival. Can J Surg 52(4):E79–E86
Helewa RM, Turner D, Park J et al (2013) Longer waiting times for patients undergoing colorectal cancer surgery are not associated with decreased survival. J Surg Oncol 108(6):378–384
Wait time alliance—Canada. http://www.waittimealliance.ca/benchmarks/general-surgery/. Accessed 19 Sept 2019
Rectal cancer surgery standards—Canada. https://s22457.pcdn.co/wp-content/uploads/2019/03/Rectal-Cancer-Surgery-Standards-EN.pdf. Updated 2019. Accessed 19 Sept 2019
Johnston GM, MacGarvie VL, Elliott D, Dewar RA, MacIntyre MM, Nolan MC (2004) Radiotherapy wait times for patients with a diagnosis of invasive cancer, 1992–2000. Clin Invest Med 27(3):142–156
Korsgaard M, Pedersen L, Sorensen HT, Laurberg S (2006) Delay of treatment is associated with advanced stage of rectal cancer but not of colon cancer. Cancer Detect Prev 30(4):341–346
Korsgaard M, Pedersen L, Laurberg S (2008) Delay of diagnosis and treatment of colorectal cancer–a population-based danish study. Cancer Detect Prev 32(1):45–51
Estonian cancer treatment quality assurance plan. https://www.sm.ee/sites/default/files/content-editors/eesmargid_ja_tegevused/Tervis/Tervislik_eluviis/eesti_vahiravi_kvaliteedi_tagamise_nouded.pdf. Updated 2011. Accessed 11 Aug 2020
Valente R, Testi A, Tanfani E et al (2009) A model to prioritize access to elective surgery on the basis of clinical urgency and waiting time. BMC Health Serv Res 9:1–1
Abu-Helalah AM, Alshraideh HA, Al-Hanaqtah M, Da’na M, Al-Omari A, Mubaidin R (2016) Delay in presentation, diagnosis, and treatment for breast cancer patients in jordan. Breast J 22(2):213–217
Yun YH, Kim YA, Min YH et al (2012) The influence of hospital volume and surgical treatment delay on long-term survival after cancer surgery. Ann Oncol 23(10):2731–2737
Lino-Silva LS, Guzmán-López JC, Zepeda-Najar C, Salcedo-Hernández RA, Meneses-García A (2019) Overall survival of patients with colon cancer and a prolonged time to surgery. J Surg Oncol 119(4):503–509
Multidisciplinary standardization oncological care in the Netherlands. https://www.soncos.org/wp-content/uploads/2017/10/43SONCOS-normeringsrapport-versie-5.pdf. Updated 2017. Accessed 13 March 2018
Gort M, Otter R, Plukker JT, Broekhuis M, Klazinga NS (2010) Actionable indicators for short and long term outcomes in rectal cancer. Eur J Cancer 46(10):1808–1814
Strous MTA, Janssen-Heijnen MLG, Vogelaar FJ (2019) Impact of therapeutic delay in colorectal cancer on overall survival and cancer recurrence: Is there a safe timeframe for prehabilitation? Eur J Surg Oncol 45(12):2295–2301
van der Geest LG, Elferink MA, Steup WH et al (2014) Guidelines-based diagnostic process does increase hospital delay in a cohort of colorectal cancer patients: A population-based study. Eur J Cancer Prev 23(5):344–352
Treeknorm—Netherlands. https://zoek.officielebekendmakingen.nl/kst-25170-31.html#IDAPMDFB. Updated 2003. Accessed 1 Oct 2019
van Steenbergen LN, Lemmens VE, Rutten HJ, Martijn H, Coebergh JW (2010) Was there shortening of the interval between diagnosis and treatment of colorectal cancer in southern netherlands between 2005 and 2008? World J Surg 34(5):1071–1079. https://doi.org/10.1007/s00268-010-0480-x
Recommendations waiting time standards for cancer care of Dutch Cancer Society. https://www.oncoline.nl/uploaded/docs/Draaiboek/Normatieve%20wachttijden.pdf. Updated 2006. Accessed 26 Sept 2019
Tiong J, Gray A, Jackson C, Thompson-Fawcett M, Schultz M (2017) Audit of the association between length of time spent on diagnostic work-up and tumour stage in patients with symptomatic colon cancer. ANZ J Surg 87(3):138–142
National cancer program—New Zealand. https://www.health.govt.nz/our-work/diseases-and-conditions/national-cancer-programme/cancer-initiatives/faster-cancer-treatment#:~:text=Faster%20cancer%20treatment%20indicators%20were,a%20high%20suspicion%20of%20cancer. Updated 2018. Accessed 13 Aug 2020
National cancer strategy 2013–2017 – Norway https://www.regjeringen.no/contentassets/07cd14ff763444a3997de1570b85fad1/i-1158_together-against_cancer_web.pdf. Accessed 8 July 2020
Nilssen Y, Brustugun OT, Tandberg Eriksen M et al (2019) Decreasing waiting time for treatment before and during implementation of cancer patient pathways in norway. Cancer Epidemiol 61:59–69
National colorectal cancer program—Norway. https://www.helsedirektoratet.no/retningslinjer/kreft-i-tykktarm-og-endetarm-handlingsprogram/IS%202849%20Nasjonalt%20handlingsprogram%20kreft%20i%20tykktarm%20og%20endetarm.pdf/_/attachment/inline/4a5fa48e-8d76-4618-98b3-43af5a85b76e:4c4a29f71e7a68ff93a19dd82848f36a49abff81/IS-2849%20Nasjonalt%20handlingsprogram%20kreft%20i%20tykktarm%20og%20endetarm.pdf. Updated 2019. Accessed 17 Aug 2020
Osowiecka K, Rucinska M, Nowakowski JJ, Nawrocki S (2018) How long are cancer patients waiting for oncological therapy in poland? Int J Environ Res Public Health 15:4. https://doi.org/10.3390/ijerph15040577
Zarcos-Pedrinaci I, Fernandez-Lopez A, Tellez T et al (2017) Factors that influence treatment delay in patients with colorectal cancer. Oncotarget 8(22):36728–36742
Guzman Laura KP, Bolibar Ribas I, Alepuz MT, Gonzalez D, Martin M (2011) Impact on patient care time and tumor stage of a program for fast diagnostic and treatment of colorectal cancer. Rev Esp Enferm Dig 103(1):13–19
Prades J, Espinas JA, Font R, Argimon JM, Borras JM (2011) Implementing a cancer fast-track programme between primary and specialised care in catalonia (spain): a mixed methods study. Br J Cancer 105(6):753–759
Standardized program for colorectal cancer—Sweden. https://kunskapsbanken.cancercentrum.se/diagnoser/tjock-och-andtarmscancer/vardforlopp/#-Fldesschema-fr-vrdfrloppet). Accessed 27 Feb 2020
Raje D, La Touche S, Mukhtar H, Oshowo A, Ingham CC (2006) Changing trends in the management of colorectal cancers and its impact on cancer waiting times. Colorectal Dis 8(2):140–144
Di Girolamo C, Walters S, Gildea C, Benitez Majano S, Rachet B, Morris M (2018) Can we assess cancer waiting time targets with cancer survival? A population-based study of individually linked data from the national cancer waiting times monitoring dataset in england, 2009–2013. PLoS ONE 13(8):e0201288
National health service cancer progamme 2000—United Kingdom. https://www.thh.nhs.uk/documents/_Departments/Cancer/NHSCancerPlan.pdf. Accessed 1 Oct 2019
Duff SE, Wood C, McCredie V, Levine E, Saunders MP, O’Dwyer ST (2004) Waiting times for treatment of rectal cancer in north west england. J R Soc Med 97(3):117–118
Robertson R, Campbell NC, Smith S et al (2004) Factors influencing time from presentation to treatment of colorectal and breast cancer in urban and rural areas. Br J Cancer 90(8):1479–1485
Chohan DP, Goodwin K, Wilkinson S, Miller R, Hall NR (2005) How has the “two-week wait” rule affected the presentation of colorectal cancer? Colorectal Dis 7(5):450–453
Maruthachalam K, Stoker E, Chaudhri S, Noblett S, Horgan AF (2005) Evolution of the two-week rule pathway–direct access colonoscopy vs outpatient appointments: one year’s experience and patient satisfaction survey. Colorectal Dis 7(5):480–485
Robinson D, Massey T, Davies E, Jack RH, Sehgal A, Moller H (2005) Waiting times for radiotherapy: variation over time and between cancer networks in southeast england. Br J Cancer 92(7):1201–1208
Currie AC, Evans J, Smith NJ, Brown G, Abulafi AM, Swift RI (2012) The impact of the two-week wait referral pathway on rectal cancer survival. Colorectal Dis 14(7):848–853
Redaniel MT, Martin RM, Blazeby JM, Wade J, Jeffreys M (2014) The association of time between diagnosis and major resection with poorer colorectal cancer survival: a retrospective cohort study. BMC Cancer 14:642–642
Aslam MI, Chaudhri S, Singh B, Jameson JS (2017) The “two-week wait” referral pathway is not associated with improved survival for patients with colorectal cancer. Int J Surg 43:181–185
Etzioni DA (2011) Timeliness of care. Semin Colon Rectal Surg 22:222–225
Eaglehouse YL, Georg MW, Shriver CD, Zhu K (2020) Racial comparisons in timeliness of colon cancer treatment in an equal-access health system. J Natl Cancer Inst 112(4):410–417
Law CW, Roslani AC, Ng LL (2009) Treatment delay in rectal cancer. Med J Malaysia 64(2):163–165
Terhaarsive Droste JS, Oort FA, van der Hulst RW et al (2010) Does delay in diagnosing colorectal cancer in symptomatic patients affect tumor stage and survival? A population-based observational study. BMC Cancer 10:332–332
Van Hout AM, de Wit NJ, Rutten FH, Peeters PH (2011) Determinants of patient’s and doctor’s delay in diagnosis and treatment of colorectal cancer. Eur J Gastroenterol Hepatol 23(11):1056–1063
Deng SX, An W, Gao J et al (2012) Factors influencing diagnosis of colorectal cancer: a hospital-based survey in china. J Dig Dis 13(10):517–524
Pruitt SL, Harzke AJ, Davidson NO, Schootman M (2013) Do diagnostic and treatment delays for colorectal cancer increase risk of death? Cancer Causes Control 24(5):961–977
Amri R, Bordeianou LG, Sylla P, Berger DL (2014) Treatment delay in surgically-treated colon cancer: Does it affect outcomes? Ann Surg Oncol 21(12):3909–3916
Curtis NJ, West MA, Salib E et al (2018) Time from colorectal cancer diagnosis to laparoscopic curative surgery-is there a safe window for prehabilitation? Int J Colorectal Dis 33(7):979–983
Weller D, Menon U, Zalounina Falborg A et al (2018) Diagnostic routes and time intervals for patients with colorectal cancer in 10 international jurisdictions; findings from a cross-sectional study from the international cancer benchmarking partnership (ICBP). BMJ Open 8(11):e023870-023870
Shin DW, Cho J, Kim SY et al (2013) Delay to curative surgery greater than 12 weeks is associated with increased mortality in patients with colorectal and breast cancer but not lung or thyroid cancer. Ann Surg Oncol 20(8):2468–2476
Bagaria SP, Heckman MG, Diehl NN, Parker A, Wasif N (2019) Delay to colectomy and survival for patients diagnosed with colon cancer. J Invest Surg 32(4):350–357
Khorana AA, Tullio K, Elson P et al (2019) Time to initial cancer treatment in the united states and association with survival over time: an observational study. PLoS ONE 14(3):e0213209
Lee YH, Kung PT, Wang YH, Kuo WY, Kao SL, Tsai WC (2019) Effect of length of time from diagnosis to treatment on colorectal cancer survival: a population-based study. PLoS ONE 14(1):e0210465
McConnell YJ, Inglis K, Porter GA (2010) Timely access and quality of care in colorectal cancer: Are they related? Int J Qual Health Care 22(3):219–228
Kaltenmeier C, Shen C, Medich DS et al (2019) Time to surgery and colon cancer survival in the united states. Ann Surg. https://doi.org/10.1097/SLA.0000000000003745
Kucejko RJ, Holleran TJ, Stein DE, Poggio JL (2020) How soon should patients with colon cancer undergo definitive resection? Dis Colon Rectum 63(2):172–182
Grunfeld E, Watters JM, Urquhart R et al (2009) A prospective study of peri-diagnostic and surgical wait times for patients with presumptive colorectal, lung, or prostate cancer. Br J Cancer 100(1):56–62
Weller D, Vedsted P, Rubin G et al (2012) The aarhus statement: Improving design and reporting of studies on early cancer diagnosis. Br J Cancer 106(7):1262–1267
Macia F, Pumarega J, Gallen M, Porta M (2013) Time from (clinical or certainty) diagnosis to treatment onset in cancer patients: The choice of diagnostic date strongly influences differences in therapeutic delay by tumor site and stage. J Clin Epidemiol 66(8):928–939
Neal RD, Tharmanathan P, France B et al (2015) Is increased time to diagnosis and treatment in symptomatic cancer associated with poorer outcomes? systematic review. Br J Cancer 112(Suppl 1):92
Malmstrom M, Rasmussen BH, Bernhardson BM et al (2018) It is important that the process goes quickly, isn’t it?" A qualitative multi-country study of colorectal or lung cancer patients’ narratives of the timeliness of diagnosis and quality of care. Eur J Oncol Nurs 34:82–88
Mathews M, Ryan D, Bulman D (2015) What does satisfaction with wait times mean to cancer patients? BMC Cancer 15:1017-z
Moore JS, Aulet TH (2017) Colorectal cancer screening. Surg Clin North Am 97(3):487–502
Dekker E, Tanis PJ, Vleugels JLA, Kasi PM, Wallace MB (2019) Colorectal cancer. Lancet 394(10207):1467–1480
Langenbach MR, Schmidt J, Neumann J, Zirngibl H (2003) Delay in treatment of colorectal cancer: multifactorial problem. World J Surg 27(3):304–308. https://doi.org/10.1007/s00268-002-6678-9
Flashman K, O’Leary DP, Senapati A, Thompson MR (2004) The department of health’s “two week standard” for bowel cancer: Is it working? Gut 53(3):387–391
Langenbach MR, Sauerland S, Krobel KW, Zirngibl H (2010) Why so late?!–delay in treatment of colorectal cancer is socially determined. Langenbecks Arch Surg 395(8):1017–1024
Thompson MR, Heath I, Swarbrick ET, Wood LF, Ellis BG (2011) Earlier diagnosis and treatment of symptomatic bowel cancer: Can it be achieved and how much will it improve survival? Colorectal Dis 13(1):6–16
Dua RS, Brown VS, Loukogeorgakis SP, Kallis G, Meleagros L (2009) The two-week rule in colorectal cancer: Can it deliver its promise? Int J Surg 7(6):521–525
Sothisrihari SR, Wright C, Hammond T (2017) Should preoperative optimization of colorectal cancer patients supersede the demands of the 62-day pathway? Colorectal Dis 19(7):617–620
Nishihara R, Wu K, Lochhead P et al (2013) Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med 369(12):1095–1105
Acknowledgements
The authors thank E. Delvaux (Máxima MC) for her contribution in the literature search and S.J.P. Jansen for his contribution in the development of the survey. We thank the following colorectal surgeons for their contribution to the current study by completing the survey: A. Ponson, Dr. Horacio Oduber Hospital (Aruba); Assoc. Prof. T. Sammour, Royal Adelaide Hospital (Australia); Prof. A.M. Wolthuis, University Hospitals Leuven (Belgium); M. Valadão, Instituto Nacional de Câncer (Brazil); Z. Wu, Peking University Cancer Hospital (China); P. Vlček, St. Ann's University Hospital (Czech Republic); Prof. I. Gögenur, Zealand University Hospital (Denmark); O. Tammik, Tartu University Clinic (Estonia); Prof. E. Cotte, Lyon-Sud Hospital (France); Prof. E. Xynos, Creta Interclinic Hospital (Greece); D. Toth, Academic County Hospital (Hungary); Prof. D.C. Winter, St. Vincent's University Hospital (Ireland); Prof. L. Boni, Surgery Policlinico of Milan (Italy); H. Ota, Ikeda City Hospital (Japan); Assoc. Prof. G. O’Grady, Auckland City Hospital (New Zealand); R. Gaupset, Akershus University Hospital (Norway); I. Negoi, Carol Davila University of Medicine and Pharmacy Bucharest (Romania); Assoc. Prof. L. Marko, Roosevelt Hospital (Slovak Republic); M. Frasson, University Hospital La Fe (Spain); Assoc. Prof. P.J. Nilsson, Karolinska University Hospital (Sweden); Prof. D. Hahnloser, University Hospital Lausanne (Switzerland); and Prof. T.A. Rockall, Royal Surrey County Hospital NHS Trust (UK). Finally, we would like to thank the peer reviewers for their feedback and recommendations on this manuscript.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
CM, LJ and GS made substantial contributions to conception and design of the study. CM performed the literature and web search. CM, LJ and GS screened and selected papers and extracted data from the included studies. CM, LJ and GS designed the survey. CM and GS sent the survey and extracted data. CM and GS conducted the web search. All authors contributed to data interpretation. CM, LJ, RR and GS primarily drafted the manuscript, and all authors revised the manuscript critically for important intellectual content and approved the final version to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
We declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Molenaar, C.J.L., Janssen, L., van der Peet, D.L. et al. Conflicting Guidelines: A Systematic Review on the Proper Interval for Colorectal Cancer Treatment. World J Surg 45, 2235–2250 (2021). https://doi.org/10.1007/s00268-021-06075-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06075-7