Abstract
Background
Prolonged hypotension is a common complication after surgery for pheochromocytomas and paragangliomas (PPGLs). It places patients at an increased risk of major morbidities and even death. The objective of the study was to investigate the risk predictors of prolonged hypotension in patients undergoing open surgery for PPGLs.
Methods
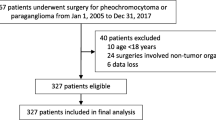
The present study adopted a retrospective, single-center design. Patients who underwent open surgery for PPGLs were enrolled from January 1, 2002, to December 31, 2018, at Peking University First Hospital. Perioperative variables were screened from patients’ electronic medical records. Prolonged hypotension was defined as hypotension that required continuous catecholamine support for at least 30 min to maintain a systolic blood pressure of > 90 mmHg after surgery.
Results
A total of 162 patients were included in the study. Fifty-two patients (31.1%) had prolonged hypotension with a median vasopressor support duration of 14 h (IQR = 4–30 h). Body mass index <24 kg/m2 (OR = 3.015, 95% CI 1.217–7.467; P = 0.017), larger tumor size (OR = 1.146, 95% CI 1.014–1.295; P = 0.029), and higher plasma norepinephrine concentration (OR = 1.053, 95% CI 1.019–1.087; P = 0.002) were associated with prolonged hypotension. Patients with prolonged hypotension had a higher incidence of complication, were more frequently admitted to the intensive care unit, underwent mechanical ventilation for a longer duration, and had a longer postoperative hospital stay when compared to those without.
Conclusion
Body mass index < 24 kg/m2, larger tumor size, and higher plasma norepinephrine concentration are independent risk predictors of prolonged hypotension in patients undergoing open surgery for PPGLs.
Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- HR:
-
Heart rate
- ICU:
-
Intensive care unit
- MV:
-
Mechanical ventilation
- PPGLs:
-
Pheochromocytomas and paragangliomas
- SBP:
-
Systolic blood pressure
References
Brauckhoff M, Gimm O, Dralle H (2004) Preoperative and surgical therapy in sporadic and familial pheochromocytoma. Front Horm Res 31:121–144
Kiernan CM, Du L, Chen X et al (2014) Predictors of hemodynamic instability during surgery for pheochromocytoma. Ann Surg Oncol 21:3865–3871
An R, Pang QY, Liu HL (2019) Association of intra-operative hypotension with acute kidney injury, myocardial injury and mortality in non-cardiac surgery: A meta-analysis. Int J Clin Pract 73(10):e13394
Malindretos PM, Sarafidis PA, Geropoulou EZ et al (2008) Sustained hypotension complicating an extra-adrenal pheochromocytoma. Am J Hypertens 21:840–842
Kurita S, Tanaka H, Sanuki M et al (2002) Severe hypotension after removal of pheochromocytoma in a pediatric patient. Masui 51:255–260
Whitelaw BC, Prague JK, Mustafa OG (2019) Mechanical circulatory support such as extracorporeal membrane oxygenation is indicated in phaeochromocytoma crisis with sustained hypotension. Clin Med (Lond) 19:91–92
Namekawa T, Utsumi T, Kawamura K et al (2016) Clinical predictors of prolonged postresection hypotension after laparoscopic adrenalectomy for pheochromocytoma. Surgery 159:763–770
Wu S, Chen W, Shen L et al (2017) Risk factors for prolonged hypotension in patients with pheochromocytoma undergoing laparoscopic adrenalectomy: a single-center retrospective study. Sci Rep 7:5897
Bai S, Yao Z, Zhu X et al (2019) Comparison of transperitoneal laparoscopic versus open adrenalectomy for large pheochromocytoma: A retrospective propensity score-matched cohort study. Int J Surg 61:26–32
Chang RY, Lang BH, Wong KP et al (2014) High pre-operative urinary norepinephrine is an independent determinant of peri-operative hemodynamic instability in unilateral pheochromocytoma/paraganglioma removal. World J Surg 38:2317–2323. https://doi.org/10.1007/s00268-014-2597-9
Randle RW, Balentine CJ, Pitt SC et al (2017) Selective versus non-selective α-blockade prior to laparoscopic adrenalectomy for pheochromocytoma. Ann Surg Oncol 24:244–250
WHO Expert Consultation (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363:157–163
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Taffurelli G, Ricci C, Casadei R et al (2017) Open adrenalectomy in the era of laparoscopic surgery: a review. Updates Surg 69:135–143
Elfenbein DM, Scarborough JE, Speicher PJ et al (2013) Comparison of laparoscopic versus open adrenalectomy: results from American College of Surgeons-National Surgery Quality Improvement Project. J Surg Res 184:216–220
Prakash P, Ramachandran R, Tandon N et al (2020) Open surgery for pheochromocytoma: current indications and outcomes from a retrospective cohort. Indian J Urol 36:21–25
Streeten DH, Anderson GH Jr (1996) Mechanisms of orthostatic hypotension and tachycardia in patients with pheochromocytoma. Am J Hypertens 9:760–769
Naranjo J, Dodd S, Martin YN (2017) Perioperative management of pheochromocytoma. J Cardiothorac Vasc Anesth 31:1427–1439
Heavner MG, Krane LS, Winters SM et al (2015) Pheochromocytoma diagnosed pathologically with previous negative serum markers. J Surg Oncol 112:492–495
An Y, Reimann M, Masjkur J et al (2019) Adrenomedullary function, obesity and permissive influences of catecholamines on body mass in patients with chromaffin cell tumours. Int J Obes (Lond) 43:263–275
Kim HJ, Lee JI, Cho YY et al (2015) Diagnostic accuracy of plasma free metanephrines in a seated position compared with 24-hour urinary metanephrines in the investigation of pheochromocytoma. Endocr J 62:243–250
Jiang M, Ding H, Liang Y et al (2018) Preoperative risk factors for hemodynamic instability during pheochromocytoma surgery in Chinese patients. Clin Endocrinol (Oxf) 88:498–505
Kwon SY, Lee KS, Lee JN et al (2016) Risk factors for hypertensive attack during pheochromocytoma resection. Investig Clin Urol 57:184–190
Liu H, Li B, Yu X et al (2017) Preoperative risk factors for massive blood loss in adrenalectomy for pheochromocytoma. Oncotarget 8:79964–79970
Scholten A, Vriens MR, Cromheecke GJ et al (2011) Hemodynamic instability during resection of pheochromocytoma in MEN versus non-MEN patients. Eur J Endocrinol 165:91–96
Eisenhofer G, Lenders JW, Goldstein DS et al (2005) Pheochromocytoma catecholamine phenotypes and prediction of tumor size and location by use of plasma free metanephrines. Clin Chem 51:735–744
Gaujoux S, Bonnet S, Lentschener C et al (2016) Preoperative risk factors of hemodynamic instability during laparoscopic adrenalectomy for pheochromocytoma. Surg Endosc 30:2984–2993
Yang RL, Liu DW, Long Y et al (2008) Perioperative hemodynamics in pheochromocytoma secreting different types of catecholamine. Zhonghua Yi Xue Za Zhi 88:816–819
Buitenwerf E, Osinga TE, Timmers HJLM et al (2019) Efficacy of α-blockers on hemodynamic control during pheochromocytoma resection-a randomized controlled trial. J Clin Endocrinol Metab 105(7):dgz188
Salmasi V, Maheshwari K, Yang D et al (2017) Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology 126:47–65
Maheshwari K, Turan A, Mao G et al (2018) The association of hypotension during non-cardiac surgery, before and after skin incision, with postoperative acute kidney injury: a retrospective cohort analysis. Anaesthesia 73:1223–1228
Araki S, Kijima T, Waseda Y et al (2019) Incidence and predictive factors of hypoglycemia after pheochromocytoma resection. Int J Urol 26:273–277
Chen Y, Hodin RA, Pandolfi C et al (2014) Hypoglycemia after resection of pheochromocytoma. Surgery 156:1404–1409
Acknowledgements
The authors gratefully acknowledge Ms. Xiao-Lu Nie (Centre for Clinical Epidemiology & Evidence-Based Medicine, Beijing Children's Hospital, Capital Medical University, Beijing 100045, China) for her assistance with statistical analysis.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Consent to participate
Because of the retrospective and observational nature of the study, the local Ethics Committee agreed to exempt written informed consent.
Ethics approval
The original study protocol was approved by the Clinical Research Ethics Committee of Peking University First Hospital, Beijing, China (2019 [47]) on July 24, 2019.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kong, H., Li, N., Tian, J. et al. Risk Predictors of Prolonged Hypotension After Open Surgery for Pheochromocytomas and Paragangliomas. World J Surg 44, 3786–3794 (2020). https://doi.org/10.1007/s00268-020-05706-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05706-9