Abstract
Background
Five billion people lack access to surgery. Accurate and complete data have been identified as essential to the global scale-up of perioperative care. This study retrospectively validates the Mbarara Surgical Services Quality Assurance Database (SQUAD), an electronic outcomes database at a Ugandan secondary referral hospital.
Methods
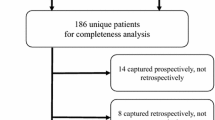
SQUAD data were compared to paper records from August 2013 to January 2017. To assess data entry accuracy, two researchers independently extracted 24 patient variables from 170 charts. To assess completeness of patient capture, SQUAD entries were compared to a sample of charts returned to the Medical Records Department, and to a sample of entries in ward and operating room logbooks. Two-tailed binomial proportions with 95% CI were calculated from the comparative results of patient observations, against a predefined accuracy of 0.85–0.95.
Results
Agreement between completed validation observations from charts and SQUAD data was 91.5% (n = 3734/4080 data points). Binomial tests indicated that 15 variables had higher than 95% accuracy. A total 19 of 24 variables had ≥ 85% accuracy. The completeness of SQUAD patient capture was 98.2% (n = 167/170) of charts returned to the Medical Records Department, 97.5% (n = 198/203) of operating logbook entries, and 100% (n = 111/111) of ward logbook entries, respectively.
Conclusion
SQUAD closely reflects the primary surgical and anaesthetic data at a Ugandan secondary hospital. Data accuracy of key variables and completeness of population capture were comparable to those of databases in high-income countries and outperformed those of other low- and middle-income countries.
Similar content being viewed by others
References
Alkire BC, Raykar NP, Shrime MG et al (2015) Global access to surgical care: a modelling study. Lancet Glob Health 3(6):e316–323
Biccard BM, Madiba TE, Kluyts HL et al (2018) Perioperative patient outcomes in the African surgical outcomes study: a 7-day prospective observational cohort study. Lancet 391(10130):1589–1598
Marmot M, Friel S, Bell R et al (2008) Closing the gap in a generation: health equity through action on the social determinants of health. The Lancet 372(9650):1661–1669
Simpson K, Gordon M (1998) The anatomy of a clinical information system. BMJ 316(7145):1655–1658
Rasanathan K, Bennett S, Atkins V et al (2017) Governing multisectoral action for health in low- and middle-income countries. PLoS Med 14(4):e1002285
Global Surgery & Anaesthesia Statistics: The Importance of Data Collection. New York: German Global Surgery Association, Program in Global Surgery and Social Change at Harvard Medical School, The G4 Alliance (2018).
Raykar NP, Yorlets RR, Liu C et al (2016) The How Project: understanding contextual challenges to global surgical care provision in low-resource settings. BMJ Global Health 1(4):e000075
Guest GD, McLeod E, Perry WRG et al (2017) Collecting data for global surgical indicators: a collaborative approach in the Pacific Region. BMJ Glob Health 2(4):e000376
Ekouevi DK, Karcher S, Coffie PA (2011) Strengthening health systems through HIV monitoring and evaluation in Sub-Saharan Africa. Curr Opin HIV AIDS 6(4):245–250
Lau F, Kuziemsky C, Price M et al (2010) A review on systematic reviews of health information system studies. J Am Med Inform Assoc 17(6):637–645
Tumusiime G, Was A, Preston MA, e al. (2017) The quality and utility of surgical and anesthetic data at a Ugandan regional referral hospital. World J Surg 2017;41(2): 370–379. Doi: 10.1007/s00268–016–3714–8
Anderson GA, Ilcisin L, Abesiga L et al (2017) (2017) Surgical volume and postoperative mortality rate at a referral hospital in Western Uganda: measuring the Lancet commission on global surgery indicators in low-resource settings. Surgery 161(6):1710–1719
Ameh EA, Shehu BB. (2002). Medical record keeping and information retrieval in developing countries: surgeons' perspective. Trop Doct 2002;32(4): 232–234.
Laing GL, Bruce JL, Skinner DL et al (2014) Development, implementation, and evaluation of a hybrid electronic medical record system specifically designed for a developing world surgical service. World J Surg 38(6):1388–1397. https://doi.org/10.1007/s00268-013-2438-2
Dale EL, Mueller MA, Wang L, et al (2013). Epidemiology of operative burns at Kijabe Hospital from 2006 to 2010: pilot study of a web-based tool for creation of the Kenya Burn Repository. Burns 2013;39(4): 788–795.
Sonshine DB, Shantz J, Kumah-Ametepey R et al (2013) The implementation of a pilot femur fracture registry at Komfo Anokye Teaching Hospital: an analysis of data quality and barriers to collaborative capacity-building. World J Surg 37(7):1506–1512. https://doi.org/10.1007/s00268-012-1726-6
Lambdin BH, Micek MA, Koepsell TD et al (2012) An assessment of the accuracy and availability of data in electronic patient tracking systems for patients receiving HIV treatment in central Mozambique. BMC Health Serv Res 12:30
Castelnuovo B, Kiragga A, Afayo V et al (2012) Implementation of provider-based electronic medical records and improvement of the quality of data in a large HIV program in Sub-Saharan Africa. PLoS ONE 7(12):e51631
Kiragga AN, Castelnuovo B, Schaefer P et al (2011) Quality of data collection in a large HIV observational clinic database in sub-Saharan Africa: implications for clinical research and audit of care. J Int AIDS Soc 14:3
Palmqvist CL, Ariyaratnam R, Watters DA et al (2015) Monitoring and evaluating surgical care: defining perioperative mortality rate and standardising data collection. Lancet 385(Suppl 2):S27
SQUAD in Uganda: Surgical Quality Assurance Database (A). 2015 (Lancet Commission on Global Surgery). https://www.globalsurgery.info/wp-content/uploads/2015/08/LCoGS-Teaching-Case-2.pdf. Accessed 21 Apr 2020.
Venermo M, Mani K, Kolh P (2017) The quality of a registry based study depends on the quality of the data - without validation, it is questionable. Eur J Vasc Endovasc Surg 53(5):611–612
Anderson GA, Ilcisin L, Ngonzi J et al (2018) Validation of an electronic surgical outcomes database at Mbarara regional referral Hospital, Uganda. World J Surg 42(1):54–60. https://doi.org/10.1007/s00268-017-4172-7
WHO. WHO Expert Committee on Specifications for Pharmaceutical Preparations—34th Report. Geneva, Switzerland: WHO Library Cataloguing in-Publication Data; 1996.
Akanbi MO, Ocheke AN, Agaba PA et al (2012) Use of electronic health records in sub-Saharan Africa: progress and challenges. J Med Trop 14(1):1–6
William M. Tierney MA, Elaine Baker, et al. (2010) The Tanzania–Uganda openMRS consortium. Experience implementing electronic health records in Three East African Countries.MEDINFO 5.
Liu C, Kayima P, Riesel J et al (2017) Brief surgical procedure code lists for outcomes measurement and quality improvement in resource-limited settings. Surgery 162(5):1163–1176
Team RC (2019) R: A language and environment for statistical computing. In: R Core Team (ed) Vienna, Austria: R Foundation for Statistical Computing
Troeng T, Malmstedt J, Bjorck M (2008) External validation of the Swedvasc registry: a first-time individual cross-matching with the unique personal identity number. Eur J Vasc Endovasc Surg 36(6):705–712
Takahashi A, Kumamaru H, Tomotaki A et al (2018) (2018) Verification of data accuracy in japan congenital cardiovascular surgery database including its postprocedural complication reports. World J Pediatr Congenit Heart Surg 9(2):150–156
Shiloach M, Frencher SK, Steeger JE et al (2010) Toward robust information: data quality and inter-rater reliability in the american college of surgeons national surgical quality improvement program. J Am Coll Surg 210(1):6–16
Hughes AJ, Hennessy O, Brennan L et al (2019) How accurate is the data provided to the Irish hip fracture database? Ir J Med Sci 188(1):13–18
Nicol E, Dudley L, Bradshaw D (2016) Assessing the quality of routine data for the prevention of mother-to-child transmission of HIV: an analytical observational study in two health districts with high HIV prevalence in South Africa. Int J Med Inform 95:60–70
Siika AM, Rotich JK, Simiyu CJ et al (2005) An electronic medical record system for ambulatory care of HIV-infected patients in Kenya. Int J Med Inform 74(5):345–355
Laing G, Bruce J, Skinner D et al (2015) Using a hybrid electronic medical record system for the surveillance of adverse surgical events and human error in a developing world surgical service. World J Surg 39(1):70–79. https://doi.org/10.1007/s00268-014-2766-x
Zargaran E, Schuurman N, Nicol AJ et al (2014) The electronic Trauma Health Record: design and usability of a novel tablet-based tool for trauma care and injury surveillance in low resource settings. J Am Coll Surg 218(1):41–50
Limburg H, Foster A, Gilbert C, et al. (2005) Routine monitoring of visual outcome of cataract surgery. Part 2: Results from eight study centres. Br J Ophthalmol 89(1): 50–52.
Kruk ME, Wladis A, Mbembati N et al (2010) Human resource and funding constraints for essential surgery in district hospitals in Africa: a retrospective cross-sectional survey. PLoS Med 7(3):e1000242
Hodges S, Wilson J, Hodges A (2009) Plastic and reconstructive surgery in Uganda-10 years experience. Paediatr Anaesth 19(1):12–18
Saswata B, Omar F, Aubery RJ et al (2005) Bridging the health gap in Uganda: the surgical role of the clinical officer. Afr Health Sci 5(1):86–89
Limburg H (2005) Routine monitoring of visual outcome of cataract surgery. Part 1: Development of an instrument. Br J Ophthalmol 89(1):45–49
Laing GL, Bruce JL, Aldous C et al (2014) The design, construction and implementation of a computerised trauma registry in a developing South African metropolitan trauma service. Injury 45(1):3–8
Elliott IS, Sonshine DB, Akhavan S et al (2015) What factors influence the production of orthopaedic research in East Africa? A qualitative analysis of interviews. Clin Orthop Relat Res 473(6):2120–2130
Lindstrom Egholm C, Helmark C, Christensen J et al (2019) Facilitators for using data from a quality registry in local quality improvement work: a cross-sectional survey of the Danish Cardiac Rehabilitation Database. BMJ Open 9(6):e028291
Were MC, Kariuki J, Chepng'Eno V et al (2010) Leapfrogging paper-based records using handheld technology- experience from Western Kenya. Stud Health Technol Inform 160:525–529
Chichom-Mefire A, Nwanna-Nzewunwa OC, Siysi VV et al (2017) Key findings from a prospective trauma registry at a regional hospital in Southwest Cameroon. PLoS ONE 12(7):e0180784
Acknowledgements
The authors acknowledge the work of the SQUAD clerks and the staff at the Medical Records Department at MRRH, whose work underlies the ultimate data quality of SQUAD. Data from this study can be made available upon reasonable request.
Funding
Funding for the database or for this publication has been provided by GE Foundation, Milton Foundation, Kletjian Foundation, MGH Department of Anesthesia, Critical Care and Pain Medicine, Göran and Erik Ennerfelt Foundation, Swedish Society for Medicine, and Fredrik Lindström Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Drevin, G., Albutt, K., Baluku, M. et al. Outcome Measurement at a Ugandan Referral Hospital: Validation of the Mbarara Surgical Services Quality Assurance Database. World J Surg 44, 2550–2556 (2020). https://doi.org/10.1007/s00268-020-05537-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05537-8