Abstract
Background
In a retrospective cohort study, we looked at the incidence and risk factors of developing in-hospital venous thromboembolism (VTE) after major emergency abdominal surgery and the risk factors for developing a venous thrombosis.
Methods
Data were extracted through medical records from all patients undergoing major emergency abdominal surgery at a Danish University Hospital from 2010 until 2016. The primary outcome was the incidence of venous thrombosis developed in the time from surgery until discharge from hospital. The secondary outcomes were 30-day mortality and postoperative complications. Multivariate logistic analyses were used for confounder control.
Results
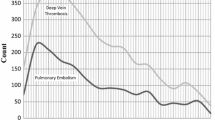
In total, 1179 patients who underwent major emergency abdominal surgery during 2010–2016 were included. Thirteen patients developed a postoperative venous thromboembolism (1.1%) while hospitalized. Eight patients developed a pulmonary embolism all verified by CT scan and five patients developed a deep venous thrombosis verified by ultrasound scan. Patients diagnosed with a VTE were significantly longer in hospital with a length of stay of 34 versus 14 days, P < 0.001, and they suffered significantly more surgical complications (69.2% vs. 30.4%, P = 0.007). Thirty-day mortality was equal in patients with and without a venous thrombosis. In a multivariate analysis adjusting for gender, ASA group, BMI, type of surgery, dalteparin dose and treatment with anticoagulants, we found that a dalteparin dose ≥5000 IU was associated with the risk of postoperative surgical complications (odds ratio 1.55, 95% CI 1.11–2.16, P = 0.009).
Conclusion
In this study, we found a low incidence of venous thrombosis among patients undergoing major emergency abdominal surgery, comparable to the incidence after elective surgery.
Similar content being viewed by others
References
Michota F (2005) Venous thromboembolism: epidemiology, characteristics, and consequences. Clin Cornerstone 7(4):8–15
Bulger CM, Jacobs C, Patel NH (2004) Epidemiology of acute deep vein thrombosis. Tech Vasc Interv Radiol 7(2):50–54
Clagett GP, Reisch JS (1988) Prevention of venous thromboembolism in general surgical patients. Results of meta-analysis. Ann Surg 208(2):227–240. https://doi.org/10.1097/00000658-198808000-00016
Institut for Rationel Farmakoterapi Dyb venøs trombose, epidemiologi, diagnose og behandling. http://www.irf.dk/dk/publikationer/rationel_farmakoterapi/maanedsblad/2009/dyb_venoes_trombose_epidemiologi_diagnose_og_behandling.htm. Accessed 2 Jan 2017
Næss IA, Christiansen SC, Romundstad P, Cannegieter SC, Rosendaal FR, Hammerstrøm J (2007) Incidence and mortality of venous thrombosis: a population-based study. J Thromb Haemost 5(4):692–699. https://doi.org/10.1111/j.1538-7836.2007.02450.x
Alsubaie H, Leggett C, Lambert P et al (2015) Diagnosis of VTE postdischarge for major abdominal and pelvic oncologic surgery: implications for a change in practice. Can J Surg 58(5):305–311
Bilgi K, Muthusamy A, Subair M et al (2016) Assessing the risk for development of VENOUS THROMBOEMBOLISM (VTE) in surgical patients using adapted Caprini scoring system. Int J Surg 30:68–73. https://doi.org/10.1016/j.ijsu.2016.04.030
Mukherjee D, Lidor AO, Chu KM, Gearhart SL, Haut ER, Chang DC (2008) Postoperative venous thromboembolism rates vary significantly after different types of major abdominal operations. J Gastrointest Surg 12(11):2015–2022. https://doi.org/10.1007/s11605-008-0600-1
Pannucci CJ, Laird S, Dimick JB, Campbell DA, Henke PK (2014) A validated risk model to predict 90-day VTE events in postsurgical patients. Chest 145(3):567–573. https://doi.org/10.1378/chest.13-1553
Screen Shot 2014-08-03 at 12
Kucher N, Spirk D, Kalka C et al (2008) Clinical predictors of prophylaxis use prior to the onset of acute venous thromboembolism in hospitalized patients SWIss Venous ThromboEmbolism Registry (SWIVTER). J Thromb Haemost 6(12):2082–2087. https://doi.org/10.1111/j.1538-7836.2008.03172.x
Bahl V, Hu HM, Henke PK, Wakefield TW, Campbell DA, Caprini JA (2010) A validation study of a retrospective venous thromboembolism risk scoring method. Ann Surg 251(2):344–350. https://doi.org/10.1097/SLA.0b013e3181b7fca6
Cohen AT, Tapson VF, Bergmann J-F et al (2008) Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. www.thelancet.com;371. https://www-clinicalkey-com.ez-sus.statsbiblioteket.dk:12048/service/content/pdf/watermarked/1-s2.0-S0140673608602020.pdf?locale=en_US. Accessed 26 March 2017
Rogers SO, Kilaru RK, Hosokawa P, Henderson WG, Zinner MJ, Khuri SF (2007) Multivariable predictors of postoperative venous thromboembolic events after general and vascular surgery: results from the patient safety in surgery study. J Am Coll Surg 204:1211–1221. https://doi.org/10.1016/j.jamcollsurg.2007.02.072
Ulrych J, Kvasnicka T, Fryba V et al (2016) 28 day post-operative persisted hypercoagulability after surgery for benign diseases: a prospective cohort study. BMC Surg 16(1):16. https://doi.org/10.1186/s12893-016-0128-3
McGoldrick DM, Redmond HP (2016) Venous thromboembolism prophylaxis risk assessment in a general surgery cohort: a closed-loop audit. Irish J Med Sci (1971). https://doi.org/10.1007/s11845-016-1529-0
Negus JJ, Gardner JJ, Tann O, Lewis S, Cohen AT (2006) Thromboprophylaxis in major abdominal surgery for cancer. Eur J Surg Oncol 32(9):911–916. https://doi.org/10.1016/j.ejso.2006.03.023
Galster H, Kolb G, Kohsytorz A, Seidlmayer C, Paal V (2000) The pre-, peri-, and postsurgical activation of coagulation and the thromboembolic risk for different risk groups. Thromb Res 100(5):381–388
Humes DJ, Walker AJ, Hunt BJ, Sultan AA, Ludvigsson JF, West J (2016) Risk of symptomatic venous thromboembolism following emergency appendicectomy in adults. Br J Surg 103(4):443–450. https://doi.org/10.1002/bjs.10091
Humes DJ, Walker AJ, Blackwell J, Hunt BJ, West J (2015) Variation in the risk of venous thromboembolism following colectomy. Br J Surg 102(13):1629–1638. https://doi.org/10.1002/bjs.9923
El-Dhuwaib Y, Selvasekar C, Corless DJ, Deakin M, Slavin JP (2017) Venous thromboembolism following colorectal resection. Color Dis 19(4):385–394. https://doi.org/10.1111/codi.13529
Pannucci CJ, Shanks A, Moote MJ et al (2012) Identifying patients at high risk for venous thromboembolism requiring treatment after outpatient surgery. Ann Surg 255(6):1093–1099. https://doi.org/10.1097/SLA.0b013e3182519ccf
Murphy PB, Vogt KN, Lau BD et al (2018) Venous thromboembolism prevention in emergency general surgery a review. JAMA Surg 153(5):479–486. https://doi.org/10.1001/jamasurg.2018.0015
Kessler D, Hunt EA, Duval-arnould J, Lin Y, Cook DA, Pusic M (2016) Reporting guidelines for health care simulation research. Adv Simul. https://doi.org/10.1097/SIH.0000000000000150
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Geerts WH, Pineo GF, Heit JA et al (2004) Prevention of venous thromboembolism. Chest 126(3):338S–400S. https://doi.org/10.1378/chest.126.3_suppl.338S
Stevens H, Tran H (2018) Update on diagnosis and anticoagulant therapy for venous thromboembolism. Intern Med J 48(10):1175–1184. https://doi.org/10.1111/imj.14063
Riva N, Vella K, Hickey K et al (2018) Biomarkers for the diagnosis of venous thromboembolism: D-dimer, thrombin generation, procoagulant phospholipid and soluble P-selectin. J Clin Pathol 71:1015–1022. https://doi.org/10.1136/jclinpath-2018-205293
Letsos S et al (2013) Influence of patient positioning and pneumoperitoneum on lower limbs venous haemodynamics during laparoscopic cholecystectomy. Hell J Surg 85:78–84
Joris JL, Noirot DP, Legrand MJ, Jacquet NJ, Lamy ML (1993) Hemodynamic changes during laparoscopic cholecystectomy. Anesth Analg 76(5):1067–1071. https://doi.org/10.1213/00000539-199305000-00027
Scholten DJ, Hoedema RM, Scholten SE (2002) A comparison of two different prophylactic dose regimens of low molecular weight heparin in bariatric surgery. Obes Surg 12(1):19–24. https://doi.org/10.1381/096089202321144522
Adolf J, Fritsche HM, Haas S et al (1999) Comparison of 3,000 IU aXa of the low molecular weight heparin certoparin with 5,000 IU aXa in prevention of deep vein thrombosis after total hip replacement. German Thrombosis Study Group. Int Angiol 18(2):122
Fleming FJ, Kim MJ, Salloum RM, Young KC, Monson JR (2010) How much do we need to worry about venous thromboembolism after hospital discharge? A study of colorectal surgery patients using the national surgical quality improvement program database. Dis Colon Rectum 53(10):1355–1360. https://doi.org/10.1007/DCR.0b013e3181eb9b0e
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Balachandran, R., Jensen, K.K., Burcharth, J. et al. Incidence of Venous Thromboembolism Following Major Emergency Abdominal Surgery. World J Surg 44, 704–710 (2020). https://doi.org/10.1007/s00268-019-05246-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05246-x