Abstract
Background
Our aim was to compare the applications of totally implanted vascular access devices (TIVAD) and peripherally inserted central catheter (PICC) in breast cancer patients.
Methods
We analyzed 4080 cases of TIVAD and 1433 cases of PICC at the Breast Center of the Fourth Hospital of Hebei Medical University. The success rate, operation time, and procedures of catheterization, as well as the catheterization-related complications, catheter indwelling-related complications, and the utilization conditions were compared between these two methods.
Results
Our results showed that the success rate of catheterization was relatively higher in PICC group (99.5%) than the TIVAD group (99.0%)(χ2 = 3.521, P = 0.038), and the operation time and the rate of catheterization-related complications were lower in PICC (18.65 ± 4.7603 min, 0.91%) compared to TIVAD (29.55 ± 4.0843 min, 1.59%)(t = 38.000, P < 0.01, χ2 = 3.578, P = 0.035). However, the rate of catheter indwelling-related complications was lower in TIVAD group (2.47%) than the PICC group (3.62%)(χ2 = 5.227, P = 0.016), and the catheter care was also better in TIVAD.
Conclusions
Based on these analyses, we recommended TIVAD for the patients who need long-term and high-dose chemotherapy and PICC for the patients who need short chemotherapy cycle and live close to the hospital.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy is an important treatment for patients with malignant tumors, and intravenous injection is the main route of drug administration. Traditional infusion requires repeated puncture on the patient skin, which not only increases the pain, but also strongly stimulates the blood vessels and damages the skin or subcutaneous tissues due to the effects of chemotherapy drugs [1]. If the drug leaks into the surrounding tissue, it can cause necrosis in skin, tendon, and nerve blood vessels, leading to various dysfunctions. This problem brings pain and inconvenience to the patient and also increases the difficulty for the next chemotherapy cycle. Currently, the relatively safer intravenous administration methods include totally implanted vascular access devices (TIVAD) [2] and peripherally inserted central catheter (PICC) [3, 4]. In a non-randomized study, 106 patients reported that there were no significant differences in complication rates between ports versus PICC [5]. In comparison, a larger study, with over 1000 patients, reported a lower complication rate for ports compared to external lumen catheters [6].Therefore, to compare these two methods, we analyzed the utilization and complications in the breast cancer patients who received chemotherapy via TIVAD or PICC at our center.
Materials and methods
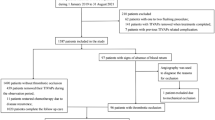
General information
We did a retrospective analysis on 4080 patients who received TIVAD from April 2014 to March 2018 and 1433 patients who received PICC from January 2014 to March 2018 at the Breast Center of the Fourth Hospital of Hebei Medical University. All of the patients are breast cancer patients. The ages of TIVAD group ranged from 17 to 84 years old, with an average of 50 years old, and the ages of PICC group ranged from 32 to 58 years old, with an average of 43.4 years old. All the patients had breast cancer.
Venous port and PICC package
The venous port used for TIVAD group was purchased from Bard company (USA), and the catheter type was 7Fr or 8Fr. The PICC group used the three-way valve puncture package produced by Bard company (USA), and the catheter type was 4Fr or 5Fr.
Catheterization method
Venous port implantation
Venous port implantation was usually performed through the internal jugular vein or subclavian vein. The catheter eventually entered the superior vena cava, and the ideal position for catheter end was the junction between superior vena cava and right atrium. After the catheter was placed, a leather bag was set up at the subclavian fossa in order to fix the infusion set; the subcutaneous tunnel was also set up, and the thickness of the subcutaneous tissue embedding the infusion set was ideally 0.5–1.0 cm. The noninvasive needle penetrated the bottom of the port vertically through the skin, and then, it was connected to the infusion device for use.
The catheterization of PICC group
The catheterization of PICC group was operated by experienced nurses. The puncture site was 2-finger under the elbow fossa or above the elbow. The preferred needle insertion vein is basilic vein, followed by the median cubital vein, and then the cephalic vein. The catheter was inserted into the superior vena cava via basilic vein, and the catheter insertion length is from the puncture point to the left and right sternoclavicular joints along the vein, plus the section down to the third intercostal space. In general, the catheter insertion length was 40–55 cm. After insertion, the catheter was covered and fixed with a sterile transparent film.
After catheterization, the position of the catheter end was confirmed by X-ray examination.
Catheter maintenance
The catheter maintenance in TIVAD group
The catheter maintenance in TIVAD group was around the injection base of the infusion port. The surrounding skin area was disinfected from inside to outside within a diameter of 10–13 cm: Alcohol was applied first to degrease, and then, iodine cotton ball was used to disinfect; when the skin was dried, alcohol cotton ball was used for deiodination, clockwise, and counter-clockwise alternating three times; then, noninvasive needle was punctured and connected to a syringe containing 0.05U/L heparin saline, which was injected to seal the catheter in pulsed-type; the noninvasive needle was removed during infusion intermission. After the daily infusion, 20 ml saline was used to flush the tube in pulsed-type, and 5 ml saline was used to seal the tube with positive pressure. After one cycle of infusion, the butterfly-winged needle was removed, followed by pulsed tube flushing with 20 ml saline, and then tube sealing with 5 ml heparin saline (0.05U/L) with positive pressure.
The catheter maintenance in PICC group
The catheter maintenance in PICC group: The arm circumference was measured first; then, the skin surrounding the degreasing puncture point was disinfected with 75% ethanol cotton ball for three times and iodine cotton ball for three times, and the diameter of disinfected area was 10 cm; finally, 0.05U/L heparin saline was used to seal the tube in pulsed-type, and the tube was fixed with a sterile film. During routine maintenance, pulsed tube flushing was conducted with 10 ml saline before and after each infusion, in order to avoid deposition of fibrin in the catheter. The back-flushed blood was avoided during tube flushing. The infusion connector with positive pressure was used.
Evaluation method
The success rate of catheterization, operation time, catheter indwelling time, catheterization-related complications, and catheter indwelling-related complications was compared between the two groups.
Statistical analysis
Statistical analysis was performed using SPSS 13.0 software. The count data were analyzed by Chi-square test, and the measurement data were analyzed by t test. P < 0.05 was considered statistically significant.
Results
Success rate of catheterization
The success rates were 99.0% (4042/4080) for TIVAD group and 99.5% (1427/1433) for PICC group. However, the one-time success rate of PICC group was significantly higher than TIVAD group (χ2 = 3.521, P = 0.038) (Table 1).
Operation time
The averaged catheterization operation time was 29.55 ± 4.0843 min for TIVAD group and 18.65 ± 4.7603 min for PICC group. PICC group had significantly shorter operation time than TIVAD group (t = 38.000, P < 0.01) (Table 1).
Catheter indwelling time
The catheter indwelling time for TIVAD group was 42–1000 days, with an average of 508.55 days. And the catheter indwelling time for PICC group was 3–238 days, with the average of 129 days. Usually, the PICC catheter was removed by the end of chemotherapy. The reasons for halfway extubation were catheter rupture/break, catheter-related infection, and venous port exposure for TIVAD group, and catheter detachment, catheter leakage, catheter-related infection, and severe phlebitis for PICC group. By comparison, there was a significant difference in catheter indwelling time between the two groups (P < 0.01) (Table 1).
Catheterization-related complications
There were 65 cases (1.59%) of catheterization-related complications in TIVAD group, including 12 cases of pneumothorax, two cases of hemothorax, 24 cases of ectopic catheter, seven cases of subcutaneous hemorrhage, one case of lymphatic fistula, 12 cases of port hematoma, and seven cases of accidental artery catheterization. There were 13 cases (0.91%) of catheterization-related complications in PICC group, including two cases of errhysis at puncture site, six cases of catheter aberrance, and five cases of mechanical phlebitis. The rates of catheterization-related complications were significantly lower in the PICC group (χ2 = 3.578, P = 0.035) (Table 1).
Catheter indwelling-related complications
There were 101 cases of catheter indwelling-related complications (2.47%) in TIVAD group, including 13 cases of infection, six cases of infusion set exposure, five cases of infusion set reversal (reel syndrome), 15 cases of catheter rupture/break, six cases of infusion site exosmosis, and 56 cases of catheter obstruction. For PICC group, there were 52 cases of catheter indwelling-related complications (3.62%), including 23 cases of infection, five cases of skin allergic changes, four cases of phlebitis, two cases of catheter coming off, four cases of thrombosis, and 14 cases of catheter obstruction. Therefore, the rates of catheter indwelling-related complications were significantly lower in TIVAD group (χ2 = 5.227, P = 0.016) (Table 1).
Discussion
Chemotherapy is the primary treatment for malignant tumors. In recent years, as the cancer incidence is increasing, the intravenous infusion methods have become the focus for medical practice, in order to both alleviate the suffering of patients and ensure better treatment. The traditional peripheral intravenous infusion not only increases the risk of phlebitis and local necrosis for patients, but also adds a significant amount of work to the nurses due to the multiple times of puncture. Therefore, choosing a venous access that is convenient, safe, and less painful is also very important for cancer treatment. In recent years, with the maturity of PICC and TIVAD technologies, more and more cancer patients use these methods for chemotherapy [7, 8]. TIVAD may be associated with some complications such as arrhythmias, pneumothorax, and arterial perforation; mechanical problems such as catheter fracture/disruption and catheter migration, extravasations, infections, occlusions, and vein thrombosis [9, 10]. The major complication rate of TIVAD ranges from 3.5 to 19% in retrospective studies [11, 12]. The complication rates of PICC ranged from 8 to 50% [13,14,15], which are higher than those associated with ports. The common complication of PICC contains infection, dislodgment, thrombosis, rupture, phlebitis, and mechanical failure [16]. However, there is no clear or consistent evidence as to which type of CVC is safer or preferable. In this study, we compared and analyzed the clinical use of PICC and TIVAD, aiming to provide useful information to cancer patients and help them choosing a more suitable infusion method.
So far, the catheterization of PICC and TIVAD has been established at our center, and both methods can achieve a high success rate of catheterization. However, the success rate in PICC group is still higher than TIVAD group, and the catheterization-related complications were significantly higher in TIVAD group. This is likely due to the special anatomy of the puncture site in TIVAD group, which makes it easier to puncture into the artery and results in pneumothorax, hemothorax, and vascular variation. Although the puncture was successful, the vascular variability might occur during the catheter delivery process, causing catheterization failure or secondary adjustment after surgery. In terms of the operation time, PICC group was significantly shorter than TIVAD group. Also, the operation in PICC is relatively simple, short, and easy to learn and can be operated in the ward. On the contrary, TIVAD needs to be carried out in the operating room and has high requirements for both operator and operating conditions. Therefore, in terms of the procedure, catheterization-related complications, and the operation time, PICC is obviously better than TIVAD.
Since some part of the catheter stays outside of body in PICC, the incidences of infection, phlebitis, catheter damage, arm swelling on the catheter placed side, catheter obstruction, and difficulty in blood withdrawal are higher [17]. In contrast, TIVAD uses subcutaneous-implanted intravenous infusion device. Although the complications such as infection and catheter occlusion can also happen [18], TIVAD is still relatively safer than PICC. In addition to the serious complications such as pneumothorax and blood pneumothorax in TIVAD, there are also some fatal complications such as catheter rupture/break that might happen during the catheter indwelling process. Since 2008, our center has performed 4080 cases of TIVAD, in which 15 cases had catheter rupture/break. Although all these cases were treated and remedied in time, the catheter end of one patient accidentally entered the pulmonary artery when we tried to take out the broken catheter. The catheter was eventually removed through the chest, and the patient was no longer in danger. Most of the studies show that the IV port can stay in body for a long time. However, based on the large number of cases we performed, we think the IV port should be removed as soon as possible after all the treatments, in order to avoid serious complications.
In addition, taking care of PICC is relatively complicated. It needs maintenance every week, and the film needs to be changed quite often. Due to the external part of the catheter in PICC, the local area needs to be kept clean and dry. If the film is curled or loose, it should be replaced as soon as possible [19]. Chen et al. [20] investigated the status of knowledge, attitude, and practice (KAP) toward the daily management of PICC in critically ill cancer patients, and they found that the KAP status toward the daily management of PICC in critically ill cancer patients discharged from intensive care units is not optimistic and needs to be further improved. Also, the arm on the catheter side should not lift heavy objects. Although the daily activities of the patients are not affected, most of the PICC patients still feel that the life quality is affected. Especially for the arm on the catheter side, its movement is not convenient. On the contrary, for TIVAD, it only needs maintenance once every month. According to most of the current chemotherapy regimens, TIVAD patients only need to take care of the catheter during chemotherapy, and it does not affect the patient daily activities.
In summary, although TIVAD has more complications than PICC during the catheterization, it is more convenient during the process of catheter indwelling and has fewer complications. Also, TIVAD does not affect the daily activities of the patient. Thereby, compared to PICC, TIVAD can greatly improve the life quality of the patient and reduce the workload of the nurses. Therefore, TIVAD is recommended for the patients who require long-term and high-dose chemotherapy such as eight cycles or more chemotherapy and those patients who lived far away from the hospital, while PICC is more suitable for the patients with shorter chemotherapy duration such as four-cycle chemotherapy or living close to hospital.
References
Singh KR, Agarwal G, Nanda G et al (2014) Morbidity of chemotherapy administration and satisfaction in breast cancer patients: a comparative study of totally implantable venous access device (TIVAD) versus peripheral venous access usage. World J Surg 38(5):1084–1092. https://doi.org/10.1007/s00268-013-2378-x
Broviac JW, Cole JJ, Scribner BH (1973) A silicone rubber atrial catheter for prolonged parenteral alimentation. Surg Gynecol Obstet 136(4):602–606
Johansson E, Hammarskjöld F, Lundberg D et al (2013) Advantages and disadvantages of peripherally inserted central venous catheters (PICC) compared to other central venous lines: a systematic review of the literature. Acta Oncol 52:886–892
Harter C, Ostendorf T, Bach A et al (2003) Peripherally inserted central catheter for autologous blood progenitor cell transplantation in patients with haema to logical malignancies. Support Care Cancer 11(12):790–794
Worth LJ, Seymour JF, Slavin MA (2009) Infective and thrombotic complications of central venous catheters in patients with hematological malignancy: prospective evaluation of nontunneled devices. Support Care Cancer 17:811–818
Groeger JS, Lucas AB, Thaler HT et al (1993) Infectious morbidity associated with long-term use of venous access devices in patients with cancer. Ann Intern Med 119:1168–1174
Patel GS, Jain K, Kumar R et al (2014) Comparison of peripherally inserted central venous catheters (PICC) versus subcutaneously implanted port-chamber catheters by complication and cost for patients receiving chemotherapy for non-haematological malignancies. Support Care Cancer 22(1):121–128
Liberale G, El Houkayem M, Viste C et al (2016) Evaluation of the perceptions and cosmetic satisfaction of breast cancer patients undergoing totally implantable vascular access device (TIVAD) placement. Support Care Cancer 24(12):5035–5040
Gallieni M, Pittiruti M, Biffi R (2008) Vascular access in oncology patients. CA Cancer J Clin 58:323–346
Sakamoto E, Hasegawa H, Komatsu S et al (2013) Complications after implantation of subcutaneous central venous port. Gan To Kagaku Ryoho 40:613–616
Ignatov A, Hoffman O, Smith B et al (2009) An 11-year retrospective study of totally implanted central venous access ports: complications and patient satisfaction. Eur J Surg Oncol 35:241–246
Sawayama H, Hayashi N, Watanabe M et al (2012) The central vein access port and catheter in outpatient chemotherapy for colorectal cancer: a retrospective study of 101 patients. Surg Today 42:29–34
Sideris LLY, Barette G, et al. (2001) Long term central venous access for chemotherapy. PICC line by the radiologist or broviac by the surgeon? Eur J Cancer 37: absract 1325
Last KMJ, Oakley C, Lofts F (1998) Long-term intravenous access devices: superiority of peripherally inserted central cannulae (PICC) over hickman catheters (HC). Ann Oncol 9:142
Yap YS, Karapetis C, Lerose S et al (2006) Reducing the risk of peripherally inserted central catheter line complications in the oncology setting. Eur J Cancer Care (Engl) 15:342–347
Walshe LJ, Malak SF, Eagan J et al (2002) Complication rates among cancer patients with peripherally inserted central catheters. J Clin Oncol 20:3276–3281
Seckold T, Walker S, Dwyer T (2015) A comparison of silicone and polyurethane PICC lines and postinsertion complication rates: a systematic review. J Vasc Access 16(3):167–177
Tang Tian-Tian, Li Yun-Tao, Zhang Li-Na et al (2016) Handling measures for the implantable vascular access device to prevent of catheter fracture/disruption. Int J Clin Exp Med 9(2):3191–3196
Bertani L, Carone M, Caricati L et al (2016) Using the theory of planned behavior to explore hospital-based nurses’ intention to use peripherally inserted central catheter (PICC): a survey study. Acta Biomed 87(4-s):23–29
Jie Chen, Hui Zhao, Zhijie Xia et al (2018) Knowledge, attitude, and practice toward the daily management of PICC in critically ill cancer patients discharged from intensive care units. Cancer Manag Res 10:1565–1574
Acknowledgements
This study was approved by the independent ethics committee of the Fourth Hospital of Hebei Medical University. All the patients provided written informed consent for genomic testing used for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Tang, Tt., Liu, L., Li, Cx. et al. Which is Better for Patients with Breast Cancer: Totally Implanted Vascular Access Devices (TIVAD) or Peripherally Inserted Central Catheter (PICC)?. World J Surg 43, 2245–2249 (2019). https://doi.org/10.1007/s00268-019-05022-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05022-x