Abstract
Background
Uniportal video-assisted thoracoscopic surgery (VATS) lobectomy has emerged as a promising and exciting approach for minimally invasive thoracic surgeries. However, nearly all reported uniportal VATS lobectomies are performed via an intercostal route, and chest wall trauma remains an issue. Here, we report the use of a novel uniportal VATS technique involving a subxiphoid route for pulmonary lobectomies.
Methods
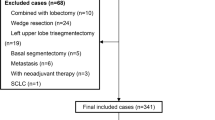
We retrospectively analyzed perioperative data for patients who underwent subxiphoid uniportal and traditional three-port VATS lobectomies from January 2016 to January 2017 at our hospital.
Results
During the study period, 37 patients successively underwent subxiphoid uniportal VATS lobectomies, including three synchronous bilateral pulmonectomies; 68 patients underwent traditional three-port VATS. There were no surgical or 30-day postoperative mortalities, and no significant between-group differences were found in the number of retrieved lymph nodes, number of explored nodal stations, blood loss, drainage time, postoperative complications, or length of hospital stay. Operative time was longer in the subxiphoid uniportal VATS group than in the traditional three-port VATS group (P < 0.001). Visual analog scale (VAS) pain scores after surgery were significantly lower in the subxiphoid uniportal VATS group (P < 0.05).
Conclusions
Subxiphoid uniportal VATS lobectomy is a safe and feasible surgical procedure associated with reduced surgical trauma and postoperative pain as well as improved cosmetic results compared with traditional VATS. Moreover, this procedure is better suited for patients receiving synchronous bilateral pulmonectomy. Further long-term follow-up analyses involving more patients are ongoing.
Trial registry number
ClinicalTrials.gov NCT03051438.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Rapid technological progress has decreased the invasiveness of thoracic surgeries, as well as the duration of postoperative rehabilitation [1]. Since 2010, uniportal video-assisted thoracoscopic surgery (VATS) lobectomy has become a new area of exploration and evolution for minimally invasive thoracic surgery [2]. Because of excellent results, uniportal VATS lobectomy is becoming increasingly accepted [3, 4]. We started using this surgical procedure in 2015 [5]. However, nearly all reported uniportal VATS lobectomies were performed via an intercostal route, and intercostal incisions can result in postoperative intercostal neuralgia and chronic thoracotomy pain [6]. Here, we report the use of a novel uniportal VATS technique involving a subxiphoid route for pulmonary lobectomy prevents these outcomes and better preserves pulmonary function. This study aims to assess the feasibility and applicability of the subxiphoid uniportal VATS approach for pulmonary lobectomy and to compare perioperative outcomes of subxiphoid uniportal and traditional three-port VATS lobectomies.
Materials and methods
Data acquisition and follow-up
We retrospectively analyzed the results of patients who underwent subxiphoid uniportal or traditional three-port VATS lobectomy between January 2016 and January 2017 at our hospital. None of these patients had received neoadjuvant therapies prior to surgery. Institutional Review Board (IRB) approval and patient consent were obtained. The retrospective study was registered at ClinicalTrials.gov (NCT03051438). Pre-, peri-, and postoperative outcome variables and patient details were collected via patient inquiry and clinical assessment.
Surgical technique
General aspects
Both subxiphoid uniportal and traditional three-port VATS lobectomies were performed under general anesthesia. A double-lumen endotracheal tube and single-lung ventilation were utilized. Required surgical equipment included Echelon Flex endoscopic articulating linear cutters (Ethicon Endo-Surgery, Somerville, NJ, USA), long curved endoscopic surgical instruments with double articulations and curved suction (Yundi, Wuxi, China), and a 10-mm 30° thoracoscope (Storz Medical AG, Tägerwilen, Switzerland).
Traditional three-port VATS technique
Traditional VATS lobectomies were completed using the three-port technique, which involves three incisions and an operative field that is visualized onscreen via a video thoracoscope [7].
Subxiphoid uniportal VATS technique
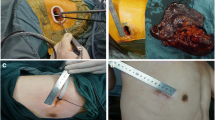
Patients were placed in a supine position, and the operating table was adjusted as needed to elevate the appropriate side of the body for surgery (Fig. 1). Both the surgeon and the assistant stood contralaterally to the surgical lung so that the same visual field was obtained, enhancing surgical coordination. A single incision approximately 4.0 cm in length was made below the xiphoid process. The incision was transverse and for bilateral lung surgeries and tilted in the direction of the operative costal arch for unilateral lung surgeries (Fig. 1a–d). The skin, subcutaneous tissue, and rectus abdominis insertion at the costal arch were cut. During single-lung ventilation, the tunnel close to the deep surface of the costal arch was bluntly dissected with a finger, and the pleural cavity was entered above the diaphragm (Fig. 1e). A plastic wound protector (Demai, Guangzhou, China) was placed in the incision to provide optimal exposure. The procedures required bimanual instrumentation with paired surgical instruments that crossed at incision sites (Fig. 1f).
The incision for subxiphoid uniportal VATS lobectomy. a The transverse incision just below the xiphoid process. b The chest tube for bilateral lung surgery. c The incision is tilted in the direction of the operative costal arch. d The chest tube for unilateral lung surgery. e The tunnel close to the deep surface of the costal arch was bluntly dissected with a finger. f The surgeon performed the operation with bimanual instrumentation; in particular, a pair of surgical instruments that were crossed at the incision site was utilized
Our surgical procedures followed classic principles of pulmonary resections, and similar to mediastinal lymphadenectomies for lung cancer, we were often required to dissect individual veins, arteries, and lobar bronchi. Of key concern was adequate exposure of the lung, which was mandatory for every step. For a subxiphoid uniportal VATS approach, an endostapler was the most convenient tool for ligating bronchi, incomplete fissures, and blood vessels due to the operative angle. Small vascular branches were difficult to divide using an endostapler. Thus, vascular clips were used in these cases. Resected tissue specimens were collected in a protective bag, and mediastinal lymphadenectomy was performed for all lung cancer patients. At the end of the operations, a U-shaped suture surrounding the chest tube was placed to close the drainage spout after extubation (Fig. 1d), and the wound was infiltrated with ropivacaine (Naropin, AstraZeneca AB, Sweden).
Upper lobectomy
Right and left upper lobectomies were performed by first dividing the artery and then the vein. The corresponding pulmonary fissure was ultimately stapled when the bronchus was transected (Fig. 2). Procedures for subxiphoid uniportal VATS of the left lung sometimes caused compression of the heart that leads to premature ventricular contraction; to overcome this problem, long curved endoscopic surgical instruments with double articulations and curved suction were used, and we attempted to minimize pressure on the heart. All patients tolerated the entire procedure well, with no instances of severe intraoperative arrhythmia.
Upper lobectomy via subxiphoid uniportal VATS. a Treatment of the right upper lobar artery. b Treatment of the right upper lobar vein. c Treatment of the right upper lobar bronchus. d Treatment of the left upper lobar artery. e Treatment of the left upper lobar vein. f Treatment of the left upper lobar bronchus
Middle lobectomy
Right middle lobectomies were performed in the following sequence: division of the anterior portion of the major fissure, the vein, the bronchus, the artery, and the remaining fissure. Only when the fissure was complete was the artery divided before the bronchus (Fig. 3a–c).
Middle and lower lobectomy via subxiphoid uniportal VATS. a Treatment of the right middle lobar vein. b Treatment of the right middle lobar bronchus. c Treatment of the right middle lobar artery. d Treatment of the right lower lobar vein. e Treatment of the right lower lobar artery. f Treatment of the right lower lobar bronchus
Lower lobectomy
For right and left lower lobectomies, the procedure was easier when the division of the fissure was complete. When the fissure was incomplete and no arteries were visible in the fissure, lobectomy was performed from bottom-to-top, with the fissure stapled last (Fig. 3d–f).
Pulmonary ground-glass opacities and small nodules
Ground-glass opacities (GGOs) and small nodules can be difficult to palpate through a subxiphoid incision. Therefore, preoperative CT-guided puncture positioning was used to pinpoint the positions of pulmonary lesions (Fig. 1f).
Statistical analysis
Categorical variables were expressed as percentages, and continuous variables were expressed as mean ± standard deviation. Variables were compared using Student’s t test, Chi-squared test, or Fisher’s exact test. Data were analyzed using SPSS 17.0. P values < 0.05 were regarded as statistically significant.
Results
Patient characteristics
Between January 2016 and January 2017, 37 patients were successfully treated via subxiphoid uniportal VATS lobectomy, including three synchronous bilateral pulmonectomies for the following purpose: (1) radical right upper lobectomy for carcinoma with left upper lobe wedge resection; (2) radical right lower lobectomy for carcinoma with left upper lobe wedge resection; (3) radical left upper lobectomy for carcinoma with right lower lobe wedge resection. A total of 68 patients underwent traditional three-port VATS. There were no surgical or 30-day postoperative mortalities. All patient characteristics and lobectomy combinations are presented in Table 1. Postoperative pathologic diagnoses included both primary lung cancers and benign conditions (Table 2). Primary lung cancers were classified by pathologic stages (stage I, II, III, or higher; Table 3).
Surgical outcomes
In both the subxiphoid uniportal and three-port VATS groups, one procedure required conversion to conventional open thoracotomy because of dense adhesions and bleeding. The conversion rates were 2.70% and 1.47%, respectively. Both converted procedures were completed safely, and no inpatient deaths occurred. There were no significant between-group differences in blood loss, number of retrieved lymph nodes, number of explored nodal stations, drainage time, or length of hospital stay. Operative time was longer in the subxiphoid uniportal VATS group compared with the traditional three-port VATS group (P < 0.01; Table 4). Three patients (8.11%) in the subxiphoid uniportal VATS group and six patients (8.82%) in the traditional three-port VATS group experienced postoperative complications (P > 0.05; Table 5).
Visual analog scale pain scores
The intensity of postoperative pain was scored using a 10-cm vertical visual analog scale (VAS) [8]. The mean VAS scores at 24 h, 48 h, 72 h, 1 week, and 1 month after surgery were 3.27 ± 1.46, 3.14 ± 1.52, 2.35 ± 1.29, 1.97 ± 0.54, and 0.79 ± 0.35, respectively, for the subxiphoid uniportal VATS group; the scores were 7.69 ± 1.32, 6.26 ± 1.28, 4.65 ± 1.63, 2.31 ± 0.75, and 1.11 ± 0.54, respectively, for the three-port VATS group. Postoperative pain scores were significantly lower (P < 0.05) in the subxiphoid uniportal VATS group than in the three-port VATS group, confirming an expected advantage of subxiphoid uniportal VATS.
Discussion
The field of thoracic surgery is continually evolving [9]. Since the first uniportal VATS lobectomy was performed by Gonzalez Rivas in 2011, there have been considerable improvements in techniques and reliability [4, 10]. The advantages of uniportal VATS over traditional three-port VATS include less postoperative pain, speedier recovery, and superior cosmetic results [11, 12]. Although postoperative pain and chest wall paresthesias can be reduced with uniportal VATS due to its minimally invasive nature, they often still occur when an incision through the intercostal space is utilized. Technological advances and innovative devices have led to the development of a novel uniportal VATS involving a subxiphoid approach [10]. Initially, this procedure was applied to pneumothorax operations, metastasectomies, and mediastinal tumor resections [11,12,13]. However, as demonstrated here, the use of novel uniportal VATS approaches for lobectomies has proved quite successful.
In this study, we compared the outcomes of pulmonary lobectomy via subxiphoid uniportal VATS with traditional three-port VATS. We found no significant between-group differences in the number of retrieved lymph nodes, number of explored nodal stations, blood loss, drainage time, postoperative complications, or length of hospital stay. Compared with other reports [14], the average number of resected lymph nodes was lower in our study. This can be explained by our routine performance of en-bloc resection of lymph nodes during mediastinal lymphadenectomy. During our procedures, we dissected and investigated over six stations of lymph nodes during mediastinal lymphadenectomy, including at least three mediastinal lymph node stations. Specifically, in our center, we conventionally dissect stations #2, 4, 7, 9, 10, 11, and 12 during right pneumonectomies, and stations #5, 6, 7, 9, 10, 11, and 12 lymph nodes during left pneumonectomies. Dissection of #7 lymph nodes is often relatively difficult. During our procedures, we pulled the lobes forward along the mediastinum below the bronchus and resected lymph nodes en-bloc. We feel this is an effective approach; as previously noted, the two groups did not differ in the number of retrieved lymph nodes or the number of explored nodal stations.
Besides the number of resected lymph nodes, other surgical outcomes in our center, including blood loss, drainage time, postoperative complications, and length of hospital stay, were mostly in accordance with other published results [15,16,17]. The positioning of patients and general surgical techniques followed Dr. Chia-Chuan Liu’s subxiphoid incision approach [16]. His techniques helped us to adapt to the new approach, and complete the operation proficiently. However, we used some extended laparoscopic instruments to better access to certain surgical regions. Our retrospective study had a limited sample size, and the next step is to expand surgical cases via subxiphoid VATS. These experiences will be summarized in future publications.
In early surgeries at our hospital, we utilized three ports by conventional thoracoscopic access. With increased technical proficiency, we were eventually able to complete the operation using one port through the thoracic cage. Now the majority of thoracic surgeries are performed with single-port VATS at our center. More importantly, we have found that the intensity of postoperative pain following the single-port approach is indeed lower than after the three-port approach. We have compared the results of procedures performed through the thoracic cage using either three ports or one port in a previous study [5]; despite the number of ports, patients continued to experience intercostal neuralgia. Thus, we began to explore uniportal subxiphoid VATS and to investigate advantages of the uniportal approach over the three-port conventional VATS. Because this technique and approach were new to us and synchronous bilateral pulmonectomies were performed in the subxiphoid uniportal VATS group, operative times for this group were somewhat prolonged. Substantially less time will likely be required for subxiphoid uniportal VATS lobectomies with increased experience and enhanced instrumentation. Finally, we found that VAS pain scores were significantly lower after surgery in the subxiphoid uniportal VATS lobectomy group than in the other group. We attributed this difference to decreased incidence of intercostal nerve injury and access trauma.
We have noted several advantages of the uniportal subxiphoid approach in this study. First, there was no limitation of shoulder movement after subxiphoid uniportal VATS, because thoracic integrity was maintained. Second, this approach involves a low risk of pulmonary complications. All the advantages above have overt benefits for enhanced recovery after surgery (ERAS) [18]. Third, for patients with bilateral pulmonary lesions, subxiphoid uniportal VATS allows synchronous bilateral pulmonectomies. Furthermore, compared with other approaches, subxiphoid uniportal VATS has superior aesthetic outcomes, with no visible chest scars.
Subxiphoid uniportal VATS lobectomy may have certain limitations under certain technical conditions. First, it is difficult to use this approach to perform complex thoracic procedures, such as surgeries in patients who have received prior thoracic irradiation and induction therapy, sleeve lobectomies, and vascular reconstructions. Second, bleeding control for vascular injuries may be significantly harder to achieve when using this approach. Third, the heart may be compressed, or arrhythmias may be encountered when passing instruments into the left chest. However, we are convinced that these weaknesses will be overcome with the continuous development of videoendoscopic instruments and endosurgical techniques.
In our study, we retrospectively analyzed the advantages and disadvantages of uniportal subxiphoid VATS in pulmonectomies compared to traditional VATS. Our recent experience demonstrates that subxiphoid uniportal VATS lobectomy is a safe and feasible surgical procedure with excellent postoperative results, particularly for patients with bilateral pulmonary lesions. However, subxiphoid uniportal VATS lobectomy is a relatively complex procedure, and appropriate expertise and instruments are critical to its success. Moreover, further analyses of subxiphoid uniportal VATS lobectomy should be conducted with more patients to better evaluate the potential and promise of this approach.
References
Hanna WC, de Valence M, Atenafu EG et al (2013) Is video-assisted lobectomy for non-small-cell lung cancer oncologically equivalent to open lobectomy? Eur J Cardiothorac Surg 43:1121–1125
Gonzalez-Rivas D, de la Torre M, Fernandez R et al (2011) Single-port video-assisted thoracoscopic left upper lobectomy. Interact Cardiovasc Thorac Surg 13:539–541
Reinersman JM, Passera E, Rocco G (2016) Overview of uniportal video-assisted thoracic surgery (VATS): past and present. Ann Cardiothorac Surg 5:112–117
Gonzalez-Rivas D, Paradela M, Fernandez R et al (2013) Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 95:426–432
Wang L, Liu D, Lu J et al (2017) The feasibility and advantage of uniportal video-assisted thoracoscopic surgery (VATS) in pulmonary lobectomy. BMC Cancer 17:75
Yim AP (1995) Minimizing chest wall trauma in video-assisted thoracic surgery. J Thorac Cardiovasc Surg 109:1255–1256
Yang X, Wang S, Qu J (2009) Video-assisted thoracic surgery (VATS) compares favorably with thoracotomy for the treatment of lung cancer: a five-year outcome comparison. World J Surg 33:1857–1861
DeLoach LJ, Higgins MS, Caplan AB et al (1998) The visual analog scale in the immediate postoperative period: intrasubject variability and correlation with a numeric scale. Anesth Analg 86:102–106
Reck M, Heigener DF, Mok T et al (2013) Management of non-small-cell lung cancer: recent developments. Lancet 382:709–719
Suda T, Ashikari S, Tochii S et al (2014) Single-incision subxiphoid approach for bilateral metastasectomy. Ann Thorac Surg 97:718–719
Liu CC, Wang BY, Shih CS et al (2015) Subxyphoid single-incision thoracoscopic pulmonary metastasectomy. Thorac Cancer 6:230–232
Liu CY, Lin CS, Liu CC (2015) Subxiphoid single-incision thoracoscopic surgery for bilateral primary spontaneous pneumothorax. Wideochir Inne Tech Maloinwazyjne 10:125–128
Wu L, Lin L, Liu M et al (2015) Subxiphoid uniportal thoracoscopic extended thymectomy. J Thorac Dis 7:1658–1660
Hsu PK, Lin WC, Chang YC et al (2015) Multiinstitutional analysis of single-port video-assisted thoracoscopic anatomical resection for primary lung cancer. Ann Thorac Surg 99:1739–1744
Aresu G, Weaver H, Wu L et al (2016) The Shanghai Pulmonary Hospital uniportal subxiphoid approach for lung segmentectomies. J Vis Surg 2:172
Aresu G, Weaver H, Wu L et al (2016) Uniportal subxiphoid video-assisted thoracoscopic bilateral segmentectomy for synchronous bilateral lung adenocarcinomas. J Vis Surg 2:170
Liu CC, Shih CS, Liu YH et al (2016) Subxiphoid single-port video-assisted thoracoscopic surgery. J Vis Surg 2:112
Wilmore DW, Kehlet H (2001) Management of patients in fast track surgery. BMJ 322:473–476
Acknowledgments
We thank Katrina Krogh, MD, from essayreview.co.kr for editing a draft of this manuscript.
Funding
This study was supported by the Specialized Research Fund for the Doctoral Program of Higher Education of China (20122104120015).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Yang, X., Wang, L., Zhang, C. et al. The Feasibility and Advantages of Subxiphoid Uniportal Video-Assisted Thoracoscopic Surgery in Pulmonary Lobectomy. World J Surg 43, 1841–1849 (2019). https://doi.org/10.1007/s00268-019-04948-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-04948-6