Abstract
Background
Although there have been many studies dealing with tracheostomy timing in trauma patients, the optimal timing is still being debated. This study aimed to compare outcomes between early tracheostomy (ET) and late tracheostomy (LT) in trauma populations to estimate the optimal timing of tracheostomy after intubation.
Methods
We retrospectively reviewed the 5 years’ data of trauma patients who underwent tracheostomy during their acute intensive care unit (ICU) stay. The cases were divided into two groups: ET was defined as tracheostomy performed within 7 days after intubation, and LT, after the seventh day. Propensity score matching was utilized using a 1-to-1 matching technique, and outcomes between two groups were compared.
Results
Among 236 enrolled patients, 76 met the criteria for ET and 160 were included for LT. Using propensity matching, 70 patients who met the criteria for ET were matched to 70 patients in the LT. Based on the comparison of outcomes after matching, ET showed significantly shorter values than LT in overall ventilator duration, length of stay at the ICU, and post-tracheostomy ventilation duration. Furthermore, the incidence of pneumonia was significantly lower with ET than with LT, although the rate of postoperative complications showed no significant differences.
Conclusions
We suggest that ET should be considered in trauma patients needing prolonged mechanical ventilation. Also, we recommend that surgeons perform tracheostomy as early as within 7 days after intubation to not only reduce the ventilation and ICU days but also prevent pneumonia without worrying about an increase in postoperative complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tracheostomy is usually performed when the patient is expected to experience prolonged endotracheal intubation and mechanical ventilation. Two to eleven percent of intensive care unit (ICU) patients requiring mechanical ventilation undergo tracheostomy during hospitalization [1]. Tracheostomy reduces oropharyngeal irrigation, minimizes the work of breathing, secures airway patency, decreases the risk of ventilator-associated pneumonia or lung injury, and improves weaning from ventilator or sedative drug use [2,3,4,5,6]. Particularly, trauma patients with severe head or chest injury who need intubation and mechanical ventilation for a long time often undergo tracheostomy for these advantages. Physicians, however, should balance such benefits with risks of complications such as bleeding, infection, nerve injury, and tracheal damage. Furthermore, evidence on the benefits of tracheotomy despite risks is necessary to influence both the patient’s family and medical providers who are hesitant to invasive procedures.
Although there have been several studies on tracheostomy timing in critically ill patients, the optimal timing is still controversial [7]. In some large multicenter randomized controlled trials conducted recently [6, 8, 9], tracheostomy timing was not associated with better outcomes. Tracheostomy timing is also an issue with trauma patients, who are a unique subpopulation of critically ill patients. Some studies [10,11,12] showed positive results of early tracheostomy (ET), whereas others [13, 14] did not.
Because the onset of illness is clear in injured patients, unlike in medically ill patients, the timing of most surgical procedures has been relatively well established for trauma populations. Thus, we selected trauma patients who underwent tracheostomy in our trauma center to estimate the optimal timing of tracheostomy. We hypothesized that ET within 7 days after intubation in trauma patients would be more beneficial for outcomes without an increase in postoperative complications than late tracheostomy (LT).
Materials and methods
Study design and setting
We reviewed data on trauma patients admitted to the ICU of Ajou University Hospital who underwent tracheostomy during their acute ICU stay. This tertiary hospital in Korea has been running a trauma center equivalent to a level I trauma center in the USA. Approximately 17,000 trauma patients visit the emergency room and 500 major trauma patients with an Injury Severity Score (ISS) of >15 are admitted to the ICU annually. In this study, we included patients ≥19 years who were admitted between January 1, 2011, and December 31, 2015; patients who received tracheostomy during the initial treatment period for the injury; and trauma patients who needed intubation within 2 days after admission and underwent tracheostomy after the first intubation. We excluded patients who were extubated and re-intubated, who were <19 years old, who were re-admitted, who were intubated due to complications, with underlying pulmonary disease such as asthma or chronic obstructive pulmonary disease (COPD), with an uncertain injury mechanism, and who were pulseless on arrival. Based on medical records and history taking from the patients and their family, we identified patients with underlying pulmonary disease as those taking medications for COPD or asthma and needing continuous follow-up at a certain medical facility. Cases who were weaned from a ventilator within a day after tracheostomy, who had severe oro-maxillofacial injury and received tracheostomy solely for securing the airway against their injuries were also excluded.
Since our protocol recommends performing tracheostomy within 7 days after placement of a mechanical ventilator, the cases were divided into the ET group (tracheostomy performed within 7 days after intubation) and LT group (tracheostomy after the seventh day). All tracheostomies were performed in the operating room by open surgical technique. All surgeries were performed and critical care given by the trauma surgeons of our department. This study was approved by the institutional review board of Ajou University Hospital. Informed consent was waived by the board because the study was observational.
Data collection and outcomes measurement
Data collected included demographic variables, vital signs at admission, ISS, amounts of transfusion within 24 h after admission, tracheostomy duration, ventilator days, ICU length of stay (LOS), morbidity, and mortality. The following outcomes were compared between the two groups and analyzed: (1) duration of mechanical ventilation (overall time and time post-tracheostomy), (2) ICU LOS, (3) rate of weaning success from a ventilator, (4) in-hospital mortality, (5) pneumonia incidence, and (6) postoperative complications.
Tracheostomy timing was calculated (date of admission coded as day 0), and ventilator days after tracheostomy were counted (date of tracheostomy coded as day 0). Particularly, pneumonia was diagnosed based on fever, leukocytosis or leukopenia, purulent sputum, abnormal radiologic findings, and culture results that satisfied general diagnostic criteria. We did not, however, necessarily apply bronchoalveolar lavage for sputum culture to patients suspected of having pneumonia according to the latest guidelines [15]. Moreover, all cases of pneumonia were confirmed by consulting a respiratory medicine and/or infectious disease specialist, and the treatment was performed with their close cooperation. Weaning success was defined as discontinuation of the ventilator for >2 weeks, and postoperative bleeding as a case that required additional surgical procedures for bleeding control. Stoma infection was diagnosed when there was purulent discharge with quantitative culture results of >105 colony-forming units/mL. Meanwhile, vocal cord palsy or tracheal granuloma was diagnosed under a laryngo-fiberscope exam and confirmed by ear, nose, and throat (ENT) doctors.
Statistical analysis
To reduce selection bias, propensity score matching was utilized using a one-to-one matching technique without replacement. The propensity score was estimated using logistic regression based on variables including age, sex, systolic blood pressure at admission, Glasgow Coma Scale (GCS) at admission, ISS, packed red blood cell (PRBC) transfusion amounts within 24 h after admission, head Abbreviated Injury Scale (AIS), and chest AIS. Continuous data were expressed as median values and interquartile ranges (IQR), and categorical data were presented as frequencies and percentages. We selected variables that allow for obtaining and confirming sufficient, reliable information from our database after selecting the candidates based on factors mentioned in previous studies [11, 12]. After propensity matching, comparisons of variables and outcomes between the ET and LT groups were performed using the Mann–Whitney U test for continuous variables and the Chi-square analysis or Fisher’s exact test (two-sided) for categorical variables. All analyses were performed using SPSS version 21.0 (IBM, Chicago, IL, USA).
Results
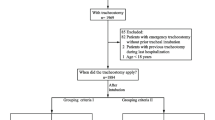
A total of 291 patients were enrolled, among which 55 were excluded: 34 with age <19 years, 12 with tracheostomy for establishing airway against oro-maxillofacial injury and weaning from a ventilator within 1 day after the procedure, 5 pulseless cases who arrived at the emergency department with an uncertain injury mechanism, and 4 with severe underlying lung disease (COPD). Thus, 236 patients were reviewed. The median age was 53 years (IQR 38–56), and 185 (78.4%) were male. The most common mechanism of injury was motor vehicle traffic injury (144 patients, 61.0%), followed by falls (65, 27.5%). Only 6 (2.5%) were injured by a penetrating mechanism. Seventy-six patients (32.2%) who underwent tracheostomy within 7 days after intubation met the criteria for ET, and the remaining 160 (67.8%) were included in the LT group. Using propensity scoring, 70 patients who met the criteria for ET were matched to 70 patients in the LT group, providing a total sample of 140 patients for outcomes analysis (Fig. 1). Prior to propensity score matching, the median age, ISS, PRBC transfusion amounts within 24 h, and rate of patients with head and chest AIS ≥ 3 points were significantly different between ET and LT (Table 1); the LT group had more-severe injuries than the ET group. Hence, the LT group had patients with older age, higher ISS, and a higher rate for head and chest AIS. However, no significant difference existed between the groups regarding age and severity after propensity matching (Table 2).
Based on the comparison of outcomes between ET and LT after propensity score matching (Table 3), ET patients showed significantly shorter overall ventilator duration (median, 14 days; IQR 9–25) and ICU LOS (median, 21 days; IQR 12–36) than LT patients [median, 35 days (IQR 25–50), and median, 42 days (IQR 31–70), respectively] (p < 0.001). Ventilator duration after tracheostomy was also significantly shorter with ET than with LT [median values, 13 days (IQR 5–23) vs. 17 days (IQR 9–30); p = 0.046]. Moreover, the ET group tended to have a better weaning success rate (91.4 vs. 81.4%), but there was no significant difference (p = 0.084). There was also no significant difference in in-hospital mortality between the groups (14.3 vs. 18.6%; p = 0.494). Furthermore, pneumonia incidence was significantly lower with ET than with LT (28 patients, 40%, vs. 46 patients, 65.7%; p = 0.002), although the rate of postoperative complications showed no significant differences between the groups. Stoma infection (15.7 vs. 8.6%) and tube displacement (5.7 vs. 1.4%) were more frequent with ET, but the differences were not statistically significant.
Discussion
Tracheostomy is usually performed in ICU patients with prolonged intubation and mechanical ventilation. Although tracheostomy is performed 10–21 days after intubation, the optimal timing is still controversial. Several randomized trials investigated the effect of ET, but the results were not conclusive due to the heterogenous characteristics of populations and ICU patients enrolled [6, 9, 14]. However, several studies reported that ET might have benefits for trauma patients [16]. A recent meta-analysis presented strong evidence regarding the beneficial effect of ET on ICU LOS, hospital LOS, mechanical ventilator days, and pneumonia incidence [17]. Romeo et al. [18] demonstrated that tracheostomy within 7 days of mechanical ventilation shortened the duration of ventilation and ICU stay in patients with spinal cord injury. Alali et al. [12] also described that tracheostomy within 8 days from intubation reduced the duration of ventilation, ICU LOS, and overall hospital LOS in patients with traumatic brain injury. Although there was no significant difference in mortality in these studies, Hyde et al. [11] demonstrated that ET could benefit trauma patients from shorter ICU LOS, fewer ventilator days, and a lower incidence of ventilator-associated pneumonia. In our study, ET was associated with reduced mechanical ventilation duration and ICU LOS. Another outcomes analysis also suggests that ET is associated with lower pneumonia incidence. However, we did not find a significant difference in mortality according to tracheostomy timing. Our results are consistent with those of several recent studies listed above [10,11,12], despite some gaps in the subpopulations enrolled, the criteria for analysis, and the medical environment among these studies.
In this study, our definition of ET as tracheostomy performed within 7 days after intubation was based on the guidelines for tracheostomy timing made by the EAST Practice Management Guidelines Work Group in 2009 [19]. We have been following the guidelines since 2011; however, the recommended ET timing is conflicting. For extreme examples, Rumbak et al. [20] defined ET as a procedure performed within 2 days after intubation, while Metha et al. [21] defined ET as within 21 days. Current systematic reviews using meta-analysis showed that ET timing was defined as generally within 5–10 days after endotracheal intubation [22,23,24]. Another meta-analysis in 2017 showed that a number of included studies utilized the 7-day cutoff in classifying tracheostomy as “early” or “late” [17]. Although the optimal timing of tracheostomy is not clearly established, a study showed that tracheostomy timing was related to ventilator duration, success rate of weaning from the mechanical ventilator, and ICU LOS [25]. Hsu et al. [26] also demonstrated that tracheostomy after 21 days from intubation was associated with weaning failure and ICU mortality. Meanwhile, Keenan et al. [13] reported that tracheostomy within 10 days after intubation was related to mortality in trauma patients without head injury. These findings make it difficult to confine the specific time limit for tracheostomy in trauma patients, especially due to numerous confounding variables associated with the outcomes.
Although we have been following the EAST guidelines since 2011, we could not always require it due to concerns from both the patient’s family and medical providers. Most family members worry about the invasiveness of the procedure, occurrence of complications, and uncertainty of the patient’s survival despite their responsibility to pay more for medical care. Medical providers become too concerned about potential postoperative complications, uncertainty of weaning from a ventilator, extubation, and keeping patients alive. Such concerns make trauma surgeons hesitate to perform ET. We also aimed to investigate the reasons for delaying tracheostomy compared with the protocol, but could not obtain sufficient data. To improve limitations in data collection and freedom to do prospective research on applying invasive procedures in the clinical traumatology field, we had to apply statistical methods.
Propensity scoring is useful in matching cases and reducing selection bias in observational studies. Despite the limitation of retrospectively collected data, we have compared the outcomes between ET and LT after adjusting for age and injury severity through such method. After matching, nearly all postoperative complications showed more frequency in the ET group, although the differences were not statistically significant. This could be because in the ET group, the procedure was performed on frailer and more edematous tissues caused by severe inflammation, before they even recovered from the catabolic stage of injury. These results, nevertheless, could influence physicians to perform tracheostomy within 7 days after intubation without worrying about postoperative complications in patients requiring prolonged mechanical ventilation. However, monitoring the incidence of stoma infection and tube displacement and maintaining the integrity of the stoma are highly necessary so as not to cancel out the effectiveness of ET.
This study has several limitations. Firstly, this is a retrospective review conducted on a small number of patients at a single institution. Therefore, the generalizability of the results is limited. However, the fact that all procedures and critical care were administered by one team in accordance with the same protocol could be an advantage in comparing outcomes between groups within a cohort. Secondly, we applied propensity score matching to create groups for comparison, which could lead to missing out some confounding factors as we only used key variables for propensity scoring. Thirdly, we did not investigate on why tracheostomy was performed early or late. Thus, even if other variables, such as the family members’ characteristics and medical providers’ personal views, might be involved in the decision of tracheostomy timing, we were not able to check on them clearly. Lastly, the spectrum of patients in the study was wide compared with those of several other studies dealing with trauma populations. The number of cases and the duration of data collection were not sufficient for us to perform in-depth analysis of more-specific subgroups such as patients with severe head injury or spinal cord injury. We only confined the sample by adjusting the number of patients with head AIS and chest AIS.
Nevertheless, the study had some notable findings and suggestions. ET within 7 days after intubation resulted in shorter ventilator duration and ICU LOS and lower pneumonia incidence without significant differences in postoperative complications. We therefore suggest that ET be considered in trauma patients requiring prolonged mechanical ventilation. Furthermore, we recommend that trauma surgeons perform tracheostomy as early as within 7 days after intubation to not only reduce the ventilation and ICU days but also prevent pneumonia without worrying about an increase in postoperative complications.
References
Scales DC, Thiruchelvam D, Kiss A, Redelmeler DA (2001) The effect of tracheostomy timing during critical illness on long-term survival. Crit Care Med 36:2547–2557
Bouderka MA, Fakhir B, Bouaggad A et al (2004) Early tracheostomy versus prolonged endotracheal intubation in severe head injury. J Trauma 57:251–254
Jeon YT, Hwang JW, Lim YJ et al (2014) Effect of tracheostomy timing on clinical outcome in neurosurgical patients: early versus late tracheostomy. J Neurosurg Anesthesiol 26:22–26
Moller MG, Slaikeu JD, Bonelli P et al (2005) Early tracheostomy versus late tracheostomy in the surgical intensive care unit. Am J Surg 189:293–296
Nieszkowska A, Combes A, Luyt CE et al (2005) Impact of tracheotomy on sedative administration, sedation level, and comfort of mechanically ventilated intensive care unit patients. Crit Care Med 33:2527–2533
Terragni PP, Antonelli M, Fumagalli R et al (2010) Early vs late tracheotomy for prevention of pneumonia in mechanically ventilated adult ICU patients: a randomized controlled trial. JAMA 303:1483–1489
Freeman BD (2017) Tracheostomy update: when and how. Crit Care Clin 33:311–322
Young D, Harrison DA, Cuthbertson BH et al (2013) Effect of early vs late tracheostomy placement on survival in patients receiving mechanical ventilation: the TracMan randomized trial. JAMA 309:2121–2129
Trouillet JL, Luyt CE, Guiguet M et al (2011) Early percutaneous tracheotomy versus prolonged intubation of mechanically ventilated patients after cardiac surgery: a randomized trial. Ann Intern Med 154:373–383
Wang HK, Lu K, Liliang PC et al (2012) The impact of tracheostomy timing in patients with severe head injury: an observational cohort study. Injury 43:1432–1436
Hyde GA, Savage SA, Zarzaur BL et al (2015) Early tracheostomy in trauma patients saves time and money. Injury 46:110–114
Alali AS, Scales DC, Fowler RA et al (2014) Tracheostomy timing in traumatic brain injury: a propensity-matched cohort study. J Trauma Acute Care 76:70–78
Keenan JE, Gulack BC, Nussbaum DP et al (2015) Optimal timing of tracheostomy after trauma without associated head injury. The J Surg Res 198:475–481
Barquist ES, Amortegui J, Hallal A et al (2006) Tracheostomy in ventilator dependent trauma patients: a prospective, randomized intention-to-treat study. J Trauma 60:91–97
Kalil AC, Metersky ML, Klompas M et al (2016) Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis 63:e61–e111
Dunham CM, Ransom KJ (2006) Assessment of early tracheostomy in trauma patients: a systematic review and meta-analysis. Am Surg 72:276–281
Cai SQ, Hu JW, Liu D et al (2017) The influence of tracheostomy timing on outcomes in trauma patients: a meta-analysis. Injury 48:866–873
Romero J, Vari A, Gambarrutta C et al (2009) Tracheostomy timing in traumatic spinal cord injury. Eur Spine J 18:1452–1457
Holevar M, Dunham JC, Brautigan R et al (2009) Practice Management Guidelines for Timing of Tracheostomy: the EAST Practice Management Guidelines Work Group. J Trauma 67:870–874
Rumbak MJ, Newton M, Truncale T et al (2004) A prospective, randomized, study comparing early percutaneous dilational tracheotomy to prolonged translaryngeal intubation (delayed tracheotomy) in critically ill medical patients. Crit Care Med 32:1689–1694
Mehta AB, Cooke CR, Wiener RS et al (2016) Hospital Variation in Early Tracheostomy in the United States: a Population-Based Study. Crit Care Med 44:1506–1514
Keeping A (2016) Early versus late tracheostomy for critically ill patients: a clinical evidence synopsis of a recent Cochrane Review. Can J Respir Ther 52:27–28
Huang H, Li Y, Ariani F, Chen X et al (2014) Timing of tracheostomy in critically ill patients: a meta-analysis. PLoS ONE 9:e92981
Gomes Silva BN, Andriolo RB, Saconato H et al (2012) Early versus late tracheostomy for critically ill patients. Cochrane Database Syst Rev 14:CD007271
Freeman BD, Borecki IB, Coopersmith CM et al (2005) Relationship between tracheostomy timing and duration of mechanical ventilation in critically ill patients. Crit Care Med 33:2513–2520
Hsu CL, Chen KY, Chang CH et al (2005) Timing of tracheostomy as a determinant of weaning success in critically ill patients: a retrospective study. Crit Care 9:R46–R52
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kang, B.H., Cho, J., Lee, J.CJ. et al. Early Versus Late Tracheostomy in Trauma Patients: A Propensity-Matched Cohort Study of 5 Years’ Data at a Single Institution in Korea. World J Surg 42, 1742–1747 (2018). https://doi.org/10.1007/s00268-018-4474-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4474-4