Abstract
Background
Femoral shaft fractures are one of the most common injuries seen by surgeons in low- and middle-income countries (LMICs). Surgical repair in LMICs is often dismissed as not being cost-effective or unsafe, though little evidence exists to support this notion. Therefore, the goal of this study is to determine the cost of intramedullary nailing of femoral shaft fractures in Tanzania.
Methods
We used micro-costing methods to estimate the fixed and variable costs of intramedullary nailing of femoral shaft fractures. Variable costs assessed included medical personnel costs, ward personnel costs, implants, medications, and single-use supplies. Fixed costs included costs for surgical instruments and administrative and ancillary staff.
Results
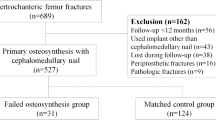
46 adult femoral shaft fracture patients admitted to Muhimbili Orthopaedic Institute between June and September 2014 were enrolled and treated with intramedullary fixation. The total cost per patient was $530.87 (SD $129.99). The mean variable cost per patient was $419.87 (SD $129.99), the largest portion coming from ward personnel $144.47 (SD $123.30), followed by implant $134.10 (SD $15.00) medical personnel $106.86 (SD $28.18), and medications/supplies $30.05 (SD $12.28). The mean fixed cost per patient was $111.00, consisting of support staff, $103.50, and surgical instruments, $7.50.
Conclusions
Our study provides empirical information on the variable and fixed costs of intramedullary nailing of femoral shaft fractures in LMICs. Importantly, the lack of surgical capacity was the primary driver of the largest cost for this procedure, preoperative ward personnel time. Our results provide the cost data for a formal cost-effectiveness analysis on this intervention.



Similar content being viewed by others
References
Lim SS, Vos T, Flaxman AD et al (2012) A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2224–2260. doi:10.1016/S0140-6736(12)61766-8
Grimes CE, Bowman KG, Dodgion CM et al (2011) Systematic review of barriers to surgical care in low-income and middle-income countries. World J Surg 35(5):941–950. doi:10.1007/s00268-011-1010-1
Farmer PE, Kim JY (2008) Surgery and global health: a view from beyond the OR. World J Surg 32(4):533–536. doi:10.1007/s00268-008-9525-9
Chao TE, Sharma K, Mandigo M et al (2014) Cost-effectiveness of surgery and its policy implications for global health: a systematic review and analysis. Lancet Glob Health 2(6):e334–e345. doi:10.1016/S2214-109X(14)70213-X
Chen AT, Pedtke A, Kobs JK et al (2012) Volunteer orthopedic surgical trips in Nicaragua: a cost-effectiveness evaluation. World J Surg 36(12):2802–2808. doi:10.1007/s00268-012-1702-1
Gosselin RA, Gialamas G, Atkin DM (2011) Comparing the cost-effectiveness of short orthopedic missions in elective and relief situations in developing countries. World J Surg 35(5):951–955. doi:10.1007/s00268-010-0947-9
Grimes CE, Henry JA, Maraka J et al (2014) Cost-effectiveness of surgery in low- and middle-income countries: a systematic review. World J Surg 38(1):252–263. doi:10.1007/s00268-013-2243-y
Phillips J, Jergesen HE, Caldwell A et al (2009) IGOT-The Institute for Global Orthopaedics and Traumatology: a model for collaboration and change. Tech Orthop 24(4):308–311. doi:10.1097/BTO.0b013e3181c3ebb1
World Health Organization (2009) Global status report on road safety: time for action. World Health Organization, Geneva
Bach O (2004) Musculoskeletal trauma in an East African public hospital. Injury 4:401–406. doi:10.1016/S0020-1383(03)00290-0
Agarwal-Harding KJ, Meara JG, Greenberg SL et al (2015) Estimating the global incidence of femoral fracture from road traffic collisions: a literature review. J Bone Joint Surg Am 6:e31. doi:10.2106/JBJS.N.00314
Mathers C, Fat DM, Boerma JT (2008) The global burden of disease: 2004 update. World Health Organization, Geneva
Bong MR, Koval KJ, Egol KA (2006) The history of intramedullary nailing. Bull NYU Hosp Jt Dis 3–4:94–97
Vecsei V, Hajdu S, Negrin LL (2011) Intramedullary nailing in fracture treatment: history, science and Kuntscher’s revolutionary influence in Vienna, Austria. Injury 42:S1–S5. doi:10.1016/S0020-1383(11)00419-0
International SFC (2012) Technique manual of SIGN IM nail & interlocking screw system insertion & extraction guide, Richland
CPI Inflation Calculator, United States Department of Labor Bureau of Labor Statistics
Zirkle LG Jr (2008) Injuries in developing countries–how can we help? The role of orthopaedic surgeons. Clin Orthop Relat Res 10:2443–2450. doi:10.1007/s11999-008-0387-0
Frye J (ed) (2014) International drug price indicator guide. Management Sciences for Health I, Medford
Barnum H, Kutzin J (1993) World Bank. Public hospitals in developing countries: resource use, cost, financing. Johns Hopkins University Press, Baltimore
Gosselin RA, Heitto M, Zirkle L (2009) Cost-effectiveness of replacing skeletal traction by interlocked intramedullary nailing for femoral shaft fractures in a provincial trauma hospital in Cambodia. Int Orthop 33(5):1445–1448. doi:10.1007/s00264-009-0798-x
GDP per capita (current US$) | Data | Table, World Bank (2014)
Iotov A, Takov E, Ivanov V et al (1996) Infraisthmal femoral fractures: cast bracing or interlocking intramedullary nailing? Ortopediya i Travmatologiya 2:58
Ikem IC, Oginni LM, Bamgboye EA (2001) Open fractures of the lower limb in Nigeria. Int Orthop 6:386–388
Mandrella B (2002) The conservative treatment of femur fractures by Perkins traction. Management in adverse situations. Unfallchirurg 105(10):923–931. doi:10.1007/s00113-002-0467-7
Gosselin R, Lavaly D (2007) Perkins traction for adult femoral shaft fractures: a report on 53 patients in Sierra Leone. Int Orthop 31(5):697–702. doi:10.1007/s00264-006-0233-5
Clasper JC, Rowley DI (2009) Outcome, following significant delays in initial surgery, of ballistic femoral fractures managed without internal or external fixation. J Bone Joint Surg Br 91(1):97–101. doi:10.1302/0301-620x.91b1.21106
Bezabeh B, Wamisho BL, Coles MJ (2012) Treatment of adult femoral shaft fractures using the Perkins traction at Addis Ababa Tikur Anbessa University Hospital: the Ethiopian experience. Int Surg 97(1):78–85. doi:10.9738/cc48.1
Doorgakant A, Mkandawire NC (2012) The management of isolated closed femoral shaft fractures in a district hospital in Malawi. Trop Dr 42(1):8–12. doi:10.1258/td.2011.110211
Opondo E, Wanzala P, Makokha A (2013) Cost effectiveness of using surgery versus skeletal traction in management of femoral shaft fractures at Thika level 5 hospital, Kenya. Pan Afr Med J 15:42. doi:10.11604/pamj.2013.15.42.2451
Eliezer E, Haonga B, Morshed S et al (2015) Predictors of reoperation for adult femoral shaft fractures treated operatively in Tanzania. Orthopaedic Trauma Association Annual Meeting, San Diego
Kramer EJ, Shearer D, Morshed S (2016) The use of traction for treating femoral shaft fractures in low- and middle-income countries: a systematic review. Int Orthop. doi:10.1007/s00264-015-3081-3
Samandari T, Bishai D, Luteijn M et al (2011) Costs and consequences of additional chest X-ray in a tuberculosis prevention program in Botswana. Am J Respir Crit Care Med 183(8):1103–1111. doi:10.1164/rccm.201004-0620OC
Jacobs B, Mercer A (1999) Feasibility of hospital-based blood banking: a Tanzanian case study. Health Policy Plan 14(4):354–362
Duke T, Peel D, Wandi F et al (2010) Oxygen supplies for hospitals in Papua New Guinea: a comparison of the feasibility and cost-effectiveness of methods for different settings. P N G Med J 53(3–4):126–138
Janson J, Marais F, Mehtar S et al (2012) Costs and process of in-patient tuberculosis management at a central academic hospital, Cape Town, South Africa. Public Health Action 2(3):61–65
Cleary S, Boulle A, McIntyre D et al (2004) Cost-effectiveness of antiretroviral treatment for HIV-positive adults in a South African township. Cost Eff Resour Alloc 4:20. doi:10.1186/1478-7547-4-20
Collins D, Gupta P, Sovannarith E (2009) Cost projections for the complementary package of activities for referral hospitals: Ministry of Health, Royal Government of CambodiaBasic Support for Institutionalizing Child Survival (USAID/BASICS). United States Agency for International Development (USAID), Arlington
Acknowledgments
Dr. Rondall Lane (UCSF), Associate Professor of Anesthesia, UCSF School of Medicine, for assistance in developing anaesthetic medicine cost equations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No potential or real conflicts of interest to report.
Appendix: equations and assumptions
Appendix: equations and assumptions
See Table 5.
Disposable supply cost details
The median supplier cost given in the database was used in this analysis with the exception of midazolam for which only a buyer median price was reported. For medications packaged in large multiuse vials, the total volume per unit was divided by the volume used and multiplied by the unit cost to assess the cost used in each procedure. The unit cost of gauze, scalpels, and needles were obtained from MOI. The cost of single-use X-ray materials were estimated from a 2008 study in Botswana [32]. The unit cost of a 500 mL transfusion was taken from a 1999 study in Tanzania [33]. The cost per litre (CPL) of oxygen gas produced from a central oxygen generator using grid electricity was estimated using the parameters of a 2010 cost study in Papua New Guinea and Eqs. 3 and 4 [34]. The cost of halothane or isoflurane used in each procedure was calculated with Eq. 5. For each patient, the costs of each supply used was summed to give a total supply and medication cost per patient.
Equation 1: Surgical personnel costs per patient (CPP)
Salaries were separated into nine occupational categories (attending orthopaedic surgeon, anaesthesiologist, medical resident, nurse anaesthetist, nurse, radiology technician, or hospital assistant):
where a is the mean wage of ward staff, calculated by dividing the mean annual salary by 1840, the product of 8 h days and 230 working days per year (365–104 weekend days–15 sick days and 16 holidays).
Equation 2: Ward personnel CPP calculated for general and private wards separately
where \(\# {\text{workers}}_{1}\) is the number of staff during normal hours (6AM–6PM), \(\# {\text{workers}}_{2}\) is the number of staff during off-hours (6PM–6AM), a is the mean wage of ward staff, b is the patient length of stay, and c is the number of patients in ward.
Equation 3: Oxygen capital cost per litre (CPL)
Equation 4: Oxygen electrical cost per litre (CPL)
where a is the (([{#Beds × 0.75} + {all ORs × 10}] × peak hours/week × 60 min × 52 weeks) + ([{#beds × 0.75} + {emergency OR × 10}] × non-peak hours/week × 60 min × 52 weeks)) × 10, b is the capacity factor based on litres needed during peak/non-peak hours, c is the TANESCO price/kWh for high power users (December 2014 prices), and d is the assuming system is designed for operation at calculated peak need +10 %, (6000 L/h).
Equation 5: Liquid volume of halothane and isoflurane used in anaesthesia
where \(Q_{{{\text{O}}_{2} }}\) is the oxygen flow rate (L/min), P is the percent by gaseous volume of the compound, M is the molecular weight of the compound (g/mol), and t is the time (min) and \(\rho\) is the density of the compound (g/mL) at 20 °C.
Equation 6: Femur fixation-specific instrument set costs per patient (CPP)
where a is the Femoral shaft fixation procedures per year.
Equation 7: Administrative and ancillary staff costs per patient, patient-day equivalent (PDE) method
where a is the inpatient equivalence ratio (IER) built by averaging the IERs of three previously published cost studies (3, 3.77, 4) [35–37].
Rights and permissions
About this article
Cite this article
Kramer, E.J., Shearer, D.W., Marseille, E. et al. The Cost of Intramedullary Nailing for Femoral Shaft Fractures in Dar es Salaam, Tanzania. World J Surg 40, 2098–2108 (2016). https://doi.org/10.1007/s00268-016-3496-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3496-z