Abstract
Introduction
The clinical entity of large parathyroid adenomas (LPTAs) has not been well defined. It is speculated that LPTAs would have biochemical, histological, and molecular characteristics different from small adenomas. Our study aimed to find out occurrence of atypia and carcinomas in large parathyroid lesions and the presence of distinct molecular abnormalities in LPTAs.
Materials and methods
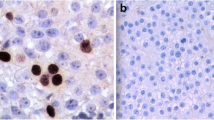
We divided the parathyroid lesions into large (>7 g, i.e., LPTAs) and small (<7 g) adenomas. We performed parafibromin, APC (adenomatous polyposis coli), galectin 3, and PGP9.5 (protein gene product 9.5) analysis by immunohistochemistry in adenomas without atypia, atypical adenomas, and carcinomas.
Results
Mean serum calcium, alkaline phosphatase, and intact PTH were significantly higher in large parathyroid tumor group. The presence of both atypical adenoma and carcinoma was higher in large parathyroid tumor group. There was higher percentage of atypia in patients with LPTAs >10 g (33 %), and 68 % of tumors showed at least one marker suggestive of malignancy in this group. Detailed analysis of immunohistochemical features of LPTA >10 g revealed that six patients showed complete loss of parafibromin immunoreactivity (out of these four showed atypia), while seven showed partial loss. In histopathologically proven malignancy (n = 9), six patients showed complete loss of parafibromin staining, 5 (55 %) APC negativity, and 45 % showed both galectin 3 and PGP9.5 positivity. Three out of these showed all IHC markers s/o malignancy, and all of them had evidence of metastases or recurrence. 32 % of atypical adenoma and 13 % of atypical adenoma showed complete loss of parafibromin staining, however none developed metastases or recurrence in follow-up (median follow-up 40 months). Loss of parafibromin staining (complete or partial) was higher in LPTA group (56 %) than that in small adenoma (39 %); however, it was not statistically significant. APC, galectin 3, and PGP9.5 markers suggestive were higher in LPTA group but were not significant.
Conclusion
LPTAs may show some morphological and immunohistochemical features suggestive of malignancy and can be considered a separate entity. However, the immunohistochemical markers are unable to clearly segregate those LPTAs that may show premalignant potential. Further, we would like to recommend that LPTAs showing complete parafibromin loss together with atypia should be kept under close follow-up.

Similar content being viewed by others
References
Mishra SK, Agarwal G, Kar DK, Gupta SK, Mithal A, Rastad J (2001) Unique clinical characteristics of primary hyperparathyroidism in India. Br J Surg 88(5):708–714
Agarwal A, Mishra SK, Gujral RB (1998) Advanced skeletal manifestations in primary hyperparathyroidism. Can J Surg 41(5):342–343
Shah VN, Bhadada S, Bhansali A, Behera A, Mittal BR (2014) Changes in clinical & biochemical presentations of primary hyperparathyroidism in India over a period of 20 years. Indian J Med Res 139(5):694–699
Agarwal A, Gupta SK, Sukumar R (2009) Hyperparathyroidism and malnutrition with severe vitamin D deficiency. World J Surg 33(11):2303–2313. doi:10.1007/s00268-009-0044-0
Singh DN, Gupta SK, Kumari N, Krishnani N, Chand G, Mishra A, Agarwal G, Verma AK, Mishra SK, Agarwal A (2015) Primary hyperparathyroidism presenting as hypercalcemic crisis: twenty-year experience. Indian J Endocrinol Metab 19(1):100–105
Agarwal G, Prasad KK, Kar DK, Krishnani N, Pandey R, Mishra SK (2006) Indian primary hyperparathyroidism patients with parathyroid carcinoma do not differ in clinic investigative characteristics from those with benign parathyroid pathology. World J Surg 30(5):732–742. doi:10.4103/2230-8210.117222
Sulaiman L, Nilsson IL, Juhlin CC, Haglund F, Höög A, Larsson C, Hashemi J (2012) Genetic characterization of large parathyroid adenomas. Endocr Relat Cancer 19(3):389–407
Bondeson L, Sandelin K, Grimelius L (1993) Histopathological variables and DNA cytometry in parathyroid carcinoma. Am J Surg Pathol 17(8):820–829
Shane E (2001) Clinical review 122: parathyroid carcinoma. J Clin Endocrinol Metab 86:485–493
Howell VM, Gill A, Clarkson A, Nelson AE, Dunne R, Delbridge LW, Robinson BG, Teh BT, Gimm O, Marsh DJ (2009) Accuracy of combined protein gene product 9.5 and parafibromin markers for immunohistochemical diagnosis of parathyroid carcinoma. J Clin Endocrinol Metab 94(2):434–441
Hubbard J, Inabnet WB, Lo CY (2009) Endocrine surgery: principles and practice. Springer Science & Business Media, London, p 325
O’Neal P, Mowschenson P, Connolly J, Hasselgren PO (2011) Large parathyroid tumors have an increased risk of atypia and carcinoma. Am J Surg 202:146–150
Bindlish V, Freeman JL, Witterick IJ, Asa SL (2002) Correlation of biochemical parameters with single parathyroid adenoma weight and volume. Head Neck 24:1000–1003
Moretz WH, Watts TL, Virgin FW, Chin E, Gourin CG, Terris DJ (2007) Correlation of intraoperative parathyroid hormone levels with parathyroid gland size. Laryngoscope 117:1957–1960
Randhawa PS, Mace AD, Nouraei SAR, Stearns MP (2007) Primary hyperparathyroidism: do perioperative biochemical variables correlate with parathyroid adenoma weight or volume? Clin Otolaryngol 32:179–184
De Lellis RA (2011) Parathyroid tumors and related disorders. Mod Pathol 24:S78–S93
Fernandez-Ranvier GG, Khanafshar E, Jensen K, Jensen K, Zarnegar R, Lee J, Kebebew E, Duh QY, Clark OH (2007) Parathyroid carcinoma, atypical parathyroid adenoma, or parathyromatosis? Cancer 110:255–264
Juhlin CC, Nilsson IL, Johansson K, Haglund F, Villablanca A, Höög A, Larsson C (2010) Parafibromin and APC as screening markers for malignant potential in atypical parathyroid adenomas. Endocr Pathol 21(3):166–177
Sandelin K, Tullgren O, Farnebo LO (1994) Clinical course of metastatic parathyroid cancer. World J Surg 18(4):594–598. doi:10.1016/j.clon.2010.04.007
Cryns VL, Rubio MP, Thor AD, Louis DN, Arnold A (1994) p53 abnormalities in human parathyroid carcinoma. J Clin Endocrinol Metab 78:1320–1324
Cetani F, Pardi E, ViacavaP Pollina GD, Fanelli G, Picone A, Borsari S, Gazzerro E, Miccoli P, Berti P, Pinchera A, Marcocci C (2004) A reappraisal of the Rb1 gene abnormalities in the diagnosis of parathyroid cancer. Clin Endocrinol (Oxf) 60:99–106
Lloyd RV, Carney JA, Ferreiro JA, Jin L, Thompson GB, Van Heerden JA, Grant CS, Wollan PC (1995) Immunohistochemical analysis of the cell cycle-associated antigens Ki-67 and retinoblastoma protein in parathyroid carcinomas and adenomas. Endocr Pathol 6(4):279–287
Juhlin CC, Nilsson IL, Johansson K, Haglund F, Villablanca A, Höög A, Larsson C (2010) Parafibromin and APC as screening markers for malignant potential in atypical parathyroid adenomas. Endocr Pathol 21(3):166–177
Bergero N, De Pompa R, Sacerdote C, Gasparri G, Volante M, Bussolati G, Papotti M (2005) Galectin-3 expression in parathyroid carcinoma: immunohistochemical study of 26 cases. Hum Pathol 36(8):908–914
Tezel E, Hibi K, Nagasaka T, Nakao A (2000) PGP9.5 as a prognostic factor in pancreatic cancer. Clin Cancer Res 6(12):4764–4767
Takano T, Miyauchi A, Matsuzuka F, Yoshida H, Nakata Y, Kuma K, Amino N (2004) PGP9.5 mRNA could contribute to the molecular-based diagnosis of medullary thyroid carcinoma. Eur J Cancer 40(4):614–618
Yamazaki T, Hibi K, Takase T, Tezel E, Nakayama H, Kasai Y, Ito K, Akiyama S, Nagasaka T, Nakao A (2002) PGP9.5 as a marker for invasive colorectal cancer. Clin Cancer Res 8(1):192–195
Carpten JD, Robbins CM, Villablanca A, Forsberg L, Presciuttini S, Bailey-Wilson J, Simonds WF, Gillanders EM, Kennedy AM, Chen JD, Agarwal SK, SoodR Jones MP, Moses TY, Haven C, Petillo D, Leotlela PD, Harding B, Cameron D, Pannett AA, Höög A, Heath H 3rd, James-Newton LA, Robinson B, ZarboRJ Cavaco BM, Wassif W, Perrier ND, Rosen IB, Kristoffersson U, Turnpenny PD, Farnebo LO, Besser GM, Jackson CE, Morreau H, Trent JM, Thakker RV, Marx SJ, Teh BT, Larsson C, Hobbs MR (2002) HRPT2, encoding parafibromin, is mutated in hyperparathyroidism-jaw tumor syndrome. Nat Genet 32:676–680
Shattuck TM, Valimaki S, Obara T, Gaz RD, Clark OH, Shoback D, Wierman ME, Tojo K, Robbins CM, Carpten JD, Farnebo LO, Larsson C, Arnold A (2003) Somatic and germ-line mutations of the HRPT2 gene in sporadic parathyroid carcinoma. N Engl J Med 349:1722–1729
Howell VM, Haven CJ, Kahnoski K, Khoo SK, Petillo D, Chen J, Fleuren GJ, Robinson BG, Delbridge LW, Philips J, Nelson AE, Krause U, Hammje K, Dralle H, Hoang-Vu C, Gimm O, Marsh DJ, Morreau H, Teh BT (2003) HRPT2 mutations are associated with malignancy in sporadic parathyroid tumours. J Med Genet 40:657–663
Tan MH, Morrison C, Wang P, Yang X, Haven CJ, Zhang C, Zhao P, Tretiakova MS, Korpi-Hyovalti E, Burgess JR, Soo KC, Cheah WK, Cao B, Resau J, Morreau H, Teh BT (2004) Loss of parafibromin immunoreactivity is a distinguishing feature of parathyroid carcinoma. Clin Cancer Res 10:6629–6637
Gill AJ, Clarkson A, Gimm O, Keil J, Dralle H, Howell VM, Marsh DJ (2006) Loss of nuclear expression of parafibromin distinguishes parathyroid carcinomas and hyperparathyroidism-jaw tumor (HPT-JT) syndrome related adenomas from sporadic parathyroid adenomas and hyperplasias. Am J Surg Pathol 30(9):1140–1149
Acknowledgments
This work was possible due to grant-in-aid from the Intramural research fund of SGPGIMS, Lucknow, India.
Author information
Authors and Affiliations
Corresponding author
Additional information
Amit Agarwal and Roma Pradhan have contributed equally to the manuscript.
Rights and permissions
About this article
Cite this article
Agarwal, A., Pradhan, R., Kumari, N. et al. Molecular Characteristics of Large Parathyroid Adenomas. World J Surg 40, 607–614 (2016). https://doi.org/10.1007/s00268-015-3380-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3380-2