Abstract
Introduction
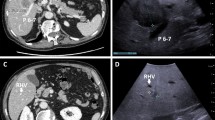
The sensitivity of preoperative assessment of colorectal liver metastases (CRLM) ranges from 74 to 80 %. Intraoperative ultrasound (IOUS) associated with contrast-enhanced intraoperative ultrasound (CE-IOUS) may be able to improve this. Thus, the aims of this study were to assess the value of IOUS and CE-IOUS for the surgical approach and to determine risk factors both for the detection of new nodules and for the modification of the surgical strategy.
Materials and methods
Forty-three patients who underwent CRLM surgery were included. These patients had an MRI in the 8 weeks preceding surgery and benefited from intraoperative IOUS and CE-IOUS.
Results and discussion
The use of IOUS/CE-IOUS permitted the identification of 43 additional lesions and an improved characterization of nodules in 23 patients with a resulting modification of surgical strategy. Lesions were down-staged in six patients and up-staged in six patients. Chemotherapy (p = 0.02) and the presence of nodules in the left lobe (p = 0.04) were predictive factors for finding new nodules at IOUS/CE-IOUS. The discovery of a new nodule systematically modified surgical management. IOUS/CE-IOUS improved intraoperative management of liver metastases. The techniques enable pertinent modification of surgical resections and a reduction of residual lesions.



Similar content being viewed by others
References
Benson MD, Gandhi MR (2000) Ultrasound of the hepatobiliary-pancreatic system. World J Surg 24:166–170. doi:10.1007/s002689910029
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 230:309
Scheele J, Stang R, Altendorf-Hofmann A, Paul M (1995) Resection of colorectal liver metastases. World J Surg 19:59–71. doi:10.1007/BF00316981
Jaeck D, Bachellier P, Guiguet M, Boudjema K, Vaillant JC, Balladur P et al (1997) Long-term survival following resection of colorectal hepatic metastases. Association Française de Chirurgie. Br J Surg 84:977–980
Adam R, Pascal G, Azoulay D, Tanaka K, Castaing D, Bismuth H (2003) Liver resection for colorectal metastases: the third hepatectomy. Ann Surg 238:871–883
Stangl R, Altendorf-Hofmann A, Charnley RM, Scheele J (1994) Factors influencing the natural history of colorectal liver metastases. Lancet 343:1405–1410
Tomlinson JS, Jarnagin WR, DeMatteo RP, Fong Y, Kornprat P, Gonen M et al (2007) Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol 25:4575–4580
Charnsangavej C, Clary B, Fong Y, Grothey A, Pawlik TM, Choti MA (2006) Selection of patients for resection of hepatic colorectal metastases: expert consensus statement. Ann Surg Oncol 13:1261–1268
Niekel MC, Bipat S, Stoker J (2010) Diagnostic imaging of colorectal liver metastases with CT, MR imaging, FDG PET, and/or FDG PET/CT: a meta-analysis of prospective studies including patients who have not previously undergone treatment. Radiology 257:674–684
Yu MH, Lee JM, Hur BY, Kim TY, Jeong SY, Yi NJ, Suh KS, Han JK, Choi BI (2015) Gadoxetic acid-enhanced MRI and diffusion-weighted imaging for the detection of colorectal liver metastases after neoadjuvant chemotherapy. Eur Radiol 25:2428–2436
Kim HJ, Lee SS, Byun JH, Kim JC, Yu CS, Park SH, Kim AY, Ha HK (2015) Incremental value of liver MR imaging in patients with potentially curable colorectal hepatic metastasis detected at CT: a prospective comparison of diffusion-weighted imaging, gadoxetic acid-enhanced MR imaging, and a combination of both MR techniques. Radiology 274:712–722
Arita J, Ono Y, Takahashi M, Inoue Y, Takahashi Y, Matsueda K, Saiura A (2015) Routine preoperative liver-specific magnetic resonance imaging does not exclude the necessity of contrast-enhanced intraoperative ultrasound in hepatic resection for colorectal liver metastasis. Ann Surg. doi:10.1097/SLA.0000000000001085
Kreft B, Pauleit D, Bachmann R, Conrad R, Krämer A, Schild HH (2001) Incidence and significance of small focal liver lesions in MRI. RöFo Fortschritte Auf Dem Geb Röntgenstrahlen Nukl 173:4–429
Schwartz LH, Gandras EJ, Colangelo SM, Ercolani MC, Panicek DM (1999) Prevalence and importance of small hepatic lesions found at CT in patients with cancer. Radiology 210:71–74
Albrecht T, Blomley MJK, Burns PN, Wilson S, Harvey CJ, Leen E et al (2003) Improved detection of hepatic metastases with pulse-inversion US during the liver-specific phase of SHU 508A: multicenter study. Radiology 227:361–370
Strobel D, Seitz K, Blank W, Schuler A, Dietrich C, von Herbay A et al (2008) Contrast-enhanced ultrasound for the characterization of focal liver lesions–diagnostic accuracy in clinical practice (DEGUM multicenter trial). Ultraschall Med 29:499–505
Tranquart F, Correas JM, Ladam Marcus V, Manzoni P, Vilgrain V, Aube C et al (2009) Real-time contrast-enhanced ultrasound in the evaluation of focal liver lesions: diagnostic efficacy and economical issues from a French multicentric study. J Radiol 90:109–122
Torzilli G, Del Fabbro D, Palmisano A, Donadon M, Bianchi P, Roncalli M et al (2005) Contrast-enhanced intraoperative ultrasonography during hepatectomies for colorectal cancer liver metastases. J Gastrointest Surg 9:1148–1153
Leen E, Ceccotti P, Moug SJ, Glen P, MacQuarrie J, Angerson WJ et al (2006) Potential value of contrast-enhanced intraoperative ultrasonography during partial hepatectomy for metastases: an essential investigation before resection? Ann Surg 243:236–240
Fioole B, de Haas RJ, Wicherts DA, Elias SG, Scheffers JM, van Hillegersberg R et al (2008) Additional value of contrast enhanced intraoperative ultrasound for colorectal liver metastases. Eur J Radiol 67:169–176
Torzilli G, Botea F, Donadon M, Cimino M, Procopio F, Pedicini V et al (2014) Criteria for the selective use of contrast-enhanced intra-operative ultrasound during surgery for colorectal liver metastases. HPB 16(11):994–1001
Arita J, Ono Y, Takahashi M, Inoue Y, Takahashi Y, Saiura A (2014) Usefulness of contrast-enhanced intraoperative ultrasound in indentifying disappearing liver metastases from colorectal carcinoma after chemotherapy. Ann Surg Oncol 21:390–397
Ferrero A, Langella S, Russolillo N, Vigano L, Lo R, Capussotti L (2012) Intraoperative detection of disappearing colorectal liver metastases as a predictor of residual disease. J Gastrointest Surg 16:806–814
Ruzzenente A, Conci S, Iacono C, Valdegamberi A et al (2013) Usefulness of contrast-enhanced intraoperative ultrasonography (CE-IOUS) in patients with colorectal liver metastases after preoperative chemotherapy. J Gastrointest Surg 17:281–287
Valls C, Andía E, Sánchez A, Gumà A, Figueras J, Torras J et al (2001) Hepatic metastases from colorectal cancer: preoperative detection and assessment of resectability with helical CT. Radiology 218:55–60
Zacherl J, Scheuba C, Imhof M, Zacherl M, Längle F, Pokieser P et al (2002) Current value of intraoperative sonography during surgery for hepatic neoplasms. World J Surg 26:550–554. doi:10.1007/s00268-001-0266-2
Spatz J, Holl G, Sciuk J, Anthuber M, Arnholdt HM, Märkl B (2010) Neoadjuvant chemotherapy affects staging of colorectal liver metastasis–a comparison of PET, CT and intraoperative ultrasound. Int J Colorectal Dis 26:165–171
Schulz A, Dormagen JB, Drolsum A, Bjørnbeth BA, Labori KJ, Kløw N-E (2012) Impact of contrast-enhanced intraoperative ultrasound on operation strategy in case of colorectal liver metastasis. Acta Radiol 53:1081–1087
Tamandl D, Herberger B, Gruenberger B, Schoppmann SF, Puhalla H, Schindl M et al (2008) Adequate preoperative staging rarely leads to a change of intraoperative strategy in patients undergoing surgery for colorectal cancer liver metastases. Surgery 143:648–657
Ferrero A, Langella S, Giuliante F, Viganò L, Vellone M, Zimmitti G et al (2013) Intraoperative liver ultrasound still affects surgical strategy for patients with colorectal metastases in the modern era. World J Surg 37:2655–2663. doi:10.1007/s00268-013-2183-6
Acknowledgments
The authors wish to thank Mr Kevin Erwin for his kind help in the English revision of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
None.
Additional information
Julien Hoareau and Aurélien Venara have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Hoareau, J., Venara, A., Lebigot, J. et al. Intraoperative Contrast-Enhanced Ultrasound in Colorectal Liver Metastasis Surgery Improves the Identification and Characterization of Nodules. World J Surg 40, 190–197 (2016). https://doi.org/10.1007/s00268-015-3269-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3269-0