Abstract
Background
Only a few papers have focused on the surgical outcomes of patients with hepatocellular carcinoma (HCC) associated with the metabolic syndrome. We compared the outcomes of patients with metabolic HCC with those of patients with non-B, non-C HCC associated with other etiologies.
Methods
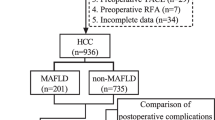
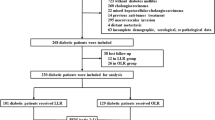
Metabolic HCC was defined as HCC arising in patients with at least three of the following metabolic disorders: central obesity, dyslipidemia, hypertension, and diabetes mellitus. A total of 246 patients with non-B, non-C HCC were divided into three groups: metabolic HCC (n = 35), alcoholic HCC (n = 114), and cryptogenic HCC (n = 97). Clinical characteristics, surgical data, and survival were compared among the three groups.
Results
Metabolic HCC was diagnosed at a significantly higher age than alcoholic (75 vs. 68 years, P = 0.004) and cryptogenic HCCs (75 vs. 71 years, P = 0.027). Postoperative complications occurred significantly higher in patients with metabolic HCC compared with those with cryptogenic HCC (40.0 vs. 22.7 %, P = 0.049). Especially, pulmonary complications were significant in metabolic HCC compared with cryptogenic HCC (22.9 vs. 8.2 %, P = 0.023). The overall survival rates in the metabolic, alcoholic, and cryptogenic HCC groups were 96.7 % (95 % CI, 90.5–100), 96.3 % (95 % CI, 92.8–99.9), and 95.6 % (95 % CI, 91.5–99.9) at 1 year, respectively, and 87.2 % (95 % CI, 74.5–100), 82.9 % (95 % CI, 74.6–92.2), and 84.5 % (95 % CI, 75.7–94.3) at 3 years, respectively (P = 0.84). The disease-free survival rates in each group were 74.4 % (95 % CI, 60.5–91.5), 76.9 % (95 % CI, 69.2–85.5), and 74.3 % (95 % CI, 65.0–84.8) at 1 year, respectively, and 29.3 % (95 % CI, 16.6–51.8), 39.0 % (95 % CI, 29.7–51.2), and 41.1 % (95 % CI, 29.7–56.8) at 3 years, respectively, (P = 0.90).
Conclusions
Metabolic HCC patients have specific risks of postoperative complication related to the metabolic syndrome.

Similar content being viewed by others
References
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Llovet JM, Burroughs A, Bruix J (2003) Hepatocellular carcinoma. Lancet 362:1907–1917
Welzel TM, Graubard BI, Zeuzem S et al (2011) Metabolic syndrome increases the risk of primary liver cancer in the United States: a study in the SEER-Medicare database. Hepatology 54:463–471
Cauchy F, Zalinski S, Dokmak S et al (2013) Surgical treatment of hepatocellular carcinoma associated with the metabolic syndrome. Br J Surg 100:113–121
McCormack L, Petrowsky H, Jochum W et al (2007) Hepatic steatosis is a risk factor for postoperative complications after major hepatectomy: a matched case-control study. Ann Surg 245:923–930
Zarzavadjian Le Bian A, Costi R, Constantinides V et al (2012) Metabolic disorders, non-alcoholic fatty liver disease and major liver resection: an underestimated perioperative risk. J Gastrointest Surg 16:2247–2255
Kleiner DE, Brunt EM, Van Natta M et al (2005) Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 41:1313–1321
Paradis V, Zalinski S, Chelbi E et al (2009) Hepatocellular carcinomas in patients with metabolic syndrome often develop without significant liver fibrosis: a pathological analysis. Hepatology 49:851–859
Wakai T, Shirai Y, Sakata J et al (2011) Surgical outcomes for hepatocellular carcinoma in nonalcoholic fatty liver disease. J Gastrointest Surg 15:1450–1458
Agopian VG, Kaldas FM, Hong JC et al (2012) Liver transplantation for nonalcoholic steatohepatitis: the new epidemic. Ann Surg 256:624–633
Heuer M, Kaiser GM, Kahraman A et al (2012) Liver transplantation in nonalcoholic steatohepatitis is associated with high mortality and post-transplant complications: a single-center experience. Digestion 86:107–113
Siegel AB, Lim EA, Wang S et al (2012) Diabetes, body mass index, and outcomes in hepatocellular carcinoma patients undergoing liver transplantation. Transplantation 94:539–543
Takayama T, Makuuchi M, Kubota K et al (2001) Randomized comparison of ultrasonic vs clamp transection of the liver. Arch Surg 136:922–928
Eckel RH, Alberti KG, Grundy SM et al (2010) The metabolic syndrome. Lancet 375:181–183
Starley BQ, Calcagno CJ, Harrison SA (2010) Nonalcoholic fatty liver disease and hepatocellular carcinoma: a weighty connection. Hepatology 51:1820–1832
Fletcher LM, Dixon JL, Purdie DM et al (2002) Excess alcohol greatly increases the prevalence of cirrhosis in hereditary hemochromatosis. Gastroenterology 122:281–289
Ludwig J, Viggiano TR, McGill DB et al (1980) Nonalcoholic steatohepatitis: Mayo clinic experiences with a hitherto unnamed disease. Mayo Clin Proc 55:434–438
Desmet VJ, Gerber M, Hoofnagle JH et al (1994) Classification of chronic hepatitis: diagnosis, grading and staging. Hepatology 19:1513–1520
Turati F, Talamini R, Pelucchi C et al (2013) Metabolic syndrome and hepatocellular carcinoma risk. Br J Cancer 108:222–228
Midorikawa Y, Kubota K, Takayama T et al (1999) A comparative study of postoperative complications after hepatectomy in patients with and without chronic liver disease. Surgery 126:484–491
Yamato I, Takayama T, Midorikawa Y et al (2012) Postoperative outcomes of patients with hepatocellular carcinoma negative for all virus-related markers. Surg Today 43:865–870
Arcidiacono B, Iiritano S, Nocera A et al (2012) Insulin resistance and cancer risk: an overview of the pathogenetic mechanisms. Exp Diabetes Res 2012:789174
Reddy SK, Steel JL, Chen HW et al (2012) Outcomes of curative treatment for hepatocellular cancer in nonalcoholic steatohepatitis versus hepatitis C and alcoholic liver disease. Hepatology 55:1809–1819
Kaneda K, Kubo S, Tanaka H et al (2012) Features and outcome after liver resection for non-B non-C hepatocellular carcinoma. Hepatogastroenterology 59:1889–1892
Utsunomiya T, Shimada M, Kudo M et al (2014) Nationwide study of 4741 patients with non-B non-C hepatocellular carcinoma with special reference to the therapeutic impact. Ann Surg 259:336–345
Acknowledgments
We thank Mr. Peter Star of Medical Network K.K. for assistance in writing the manuscript. This work was mainly supported by a Grant-in-Aid for Scientific Research (A) 24249068 (T.T.) from the Ministry of Education, Culture, Sports, Science and Technology (MEXT), Japan.
Conflict of interest
We declare that we have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yoshida, N., Takayama, T., Midorikawa, Y. et al. Surgical Outcomes in Patients with Hepatocellular Carcinoma Associated with Metabolic Syndrome. World J Surg 39, 471–477 (2015). https://doi.org/10.1007/s00268-014-2828-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2828-0