Abstract
Background
Chyle leak complicates 1.3–10.8 % of pancreatic resections. Universal use of parenteral nutrition following pancreatic resection may reduce the incidence of chyle leak. However, this denies the majority of patients who do not develop chyle leak the benefits of enteral nutrition (EN). The present study aimed to identify risk factors for chyle leak following pancreatic resection within a single institution where EN was used universally.
Methods
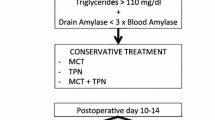
All patients who underwent pancreatic resection between January 2007 and December 2010 were identified retrospectively. The patients had been treated according to a common unit protocol of enteral feeding; those developing chyle leak were switched to a medium-chain triglyceride (MCT) regimen. Clinical progress and recovery after surgery was evaluated. Multivariate analysis was performed to identify factors associated with chyle leak.
Results
A total of 245 patients underwent major pancreatic resection (231 pancreatoduodenectomy, 14 total pancreatectomy). Chyle leak complicated 40 cases (16.3 %). After multivariate analysis, both extensive lymphadenectomy (P = 0.002) and postoperative portal/mesenteric venous thrombosis (PVT) (P = 0.009) were independently linked with a higher incidence of chyle leak. The development of chyle leak was not associated with poorer survival or prolonged duration of hospital stay. It was associated with a significantly increased duration of abdominal drainage and reduced likelihood of early hospital discharge (P = 0.026).
Conclusions
Universal use of enteral feeding is associated with a high rate of chyle leak following pancreatic resection. Patients undergoing extensive lymphadenectomy or those who develop PVT postoperatively are at increased risk. Development of chyle leak was not associated with additional morbidity or mortality following implementation of an MCT regimen. The implication is that reactive management of chyle leak with conversion to a MCT predominant diet is safe.
Similar content being viewed by others
References
Leibovitch I, Mor Y, Golomb J et al (2002) The diagnosis and management of postoperative chylous ascites. J Urol 167:449–457
Malik HZ, Crozier J, Murray L et al (2007) Chyle leakage and early enteral feeding following pancreaticoduodenectomy: management options. Dig Surg 24:418–422
Geisler JP, Foster RS, Sutton GP (1994) Chyloperitoneum following treatment for advanced gynecologic malignancies. Obstet Gynecol 83:883–885
Weston PM, Greenland JE, Wallace DM (1992) Chylous ascites following retroperitoneal lymph node dissection for testis cancer. Br J Urol 70:688–689
Bacelar TS, de Albuquerque AC, de Arruda PC et al (2003) Postoperative chylous ascites: a rare complication of laparoscopic Nissen fundoplication. JSLS 7:269–271
Guillem P, Billeret V, Houcke ML et al (1999) Successful management of post esophagectomy chylothorax by etilefrine. Dis Esophagus 12:155–156
Wu CW, Hsieh MC, Lo SS et al (1996) Results of curative gastrectomy for carcinoma of the distal third of the stomach. J Am Coll Surg 183:201–207
al-Mousawi M, Abu Nema T (1991) Chylous ascites: a rare complication of vagotomy. Eur J Surg 157:149–150
Prabhakaran K, Vidyadhar M, Jahoorahmad P et al (2004) Chylous ascites following liver resection—case report. Pediatr Surg Int 20:719–721
DeHart MM, Lauerman WC, Conely AH et al (1994) Management of retroperitoneal leakage. Spine 19:716–718
Crespo-Leiro MG, Ayucar A, Portela F et al (1998) Chylous ascites following heart transplantation. J Cardiovasc Surg (Torino) 39:217–219
Asfar S, Lowndes R, Wall WJ (1994) Chylous ascites after liver transplantation. Transplantation 58:368–369
Assumpcao L, Cameron JL, Wolfgang CL et al (2008) Incidence and management of chyle leaks following pancreatic resection: a high volume single-centre institutional experience. J Gastrointest Surg 12:1915–1923
van der Gaag NA, Verhaar AC, Haverkort EB et al (2008) Chylous ascites after pancreaticoduodenectomy: introduction of a grading system. J Am Coll Surg 207:751–757
Laterre PF, Dugernier T, Reynaert MS (2000) Chylous ascites: diagnosis, causes and treatment. Acta Gastroenterol Belg 6:260–263
Weimann A, Braga M, Harsanyi L (2006) ESPEN guidelines on enteral nutrition: surgery including organ transplantation. Clin Nutr 25:224–244
Phillips M, Lordan JT, Menezes N et al (2009) Feeding patients following pancreaticoduodenectomy: a UK national survey. Ann R Coll Surg Engl 91:385–388
Braga M, Gianotti L, Vignali A et al (1998) Artificial nutrition after major abdominal surgery: impact of route of administration and composition of the diet. Crit Care Med 26:24–30
Schroeder D, Gillanders L, Mahr K et al (1991) Effect of immediate postoperative enteral nutrition on body composition, muscle function and wound healing. J Parenter Enteral Nutr 15:376–383
Kudsk KA (2007) Beneficial effect of enteral feeding. Gastrointest Endosc Clin N Am 17:647–662
Bozzetti F, Braga M, Gianotti L et al (2001) Postoperative enteral verses parenteral nutrition in malnourished patients with gastrointestinal cancer: a randomised multicentre trial. Lancet 358:1487–1492
Gianotti L, Braga M, Gentilini O et al (2000) Artificial nutrition after pancreaticoduodenectomy. Pancreas 21:344–351
Goonetilleke KS, Siriwardena AK (2006) Systematic review of peri-operative nutritional supplementation in patients undergoing pancreaticoduodenectomy. JOP 7:5–13
Intensive Care Society Standards and Guidelines (2009) http://www.ics.ac.uk/professional/standards_safety_quality/standards_and_guidelines/levels_of_critical_care_for_adult_patients. Accessed 02 Jan 2012
Pedrazzoli S, DiCarlo V, Dionigi R et al (1998) Standard versus extended lymphadenectomy associated with pancreatoduodenectomy in the surgical treatment of adenocarcinoma of the head of the pancreas: a multicenter, prospective, randomized study. Lymphadenectomy Study Group. Ann Surg 228:508–517
Schofield WN (1985) Predicting basal metabolic rate; new standards and review of previous work. Hum Nutr Clin Nutr 39(Suppl 1):5–41
Tani M, Terasawa H, Kawai M et al (2006) Improvement of delayed gastric emptying in pylorus-preserving pancreaticoduodenectomy: results of a prospective, randomized, controlled trial. Ann Surg 243:316–320
Smoke A, Delegge MH (2008) Chyle leaks: consensus on management? Nutr Clin Pract 23:529–532
Lassen K, Kjoeve J, Fetveit T et al (2008) Allowing normal food at will after major upper gastrointestinal surgery does not increase morbidity: a randomised multicenter trial. Ann Surg 247:721–729
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hilal, M.A., Layfield, D.M., Di Fabio, F. et al. Postoperative Chyle Leak After Major Pancreatic Resections in Patients Who Receive Enteral Feed: Risk Factors and Management Options. World J Surg 37, 2918–2926 (2013). https://doi.org/10.1007/s00268-013-2171-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2171-x