Abstract
Background
There are contrary opinions regarding the surgical treatment of pulmonary hydatid cysts. We report our experience performing a modified version of uncapitonnage surgery, called “saucerization,” for treating pulmonary hydatid cysts.
Methods
A total of 78 patients with pulmonary hydatid cysts were studied regarding their surgery outcome and the complication rate. The procedure used for cyst evacuation depended on whether the cyst had ruptured. If ruptured, cystotomy was done; otherwise, enucleation was preferred. To deal with the residual cavity in an uncapitonnage manner, we removed the thin margins of the pericyst and closed the bronchial openings at the cavity floor. All patients were followed up at least for 6 months.
Results
The intensive care unit stay ranged from 1 to 9 days. Incomplete lung expansion (six patients) was the main postoperative complication followed by wound infection (four patients) and persistent air leak (≥7 days) (one patient). There was one death. Dependence on mechanical ventilation and subsequent septic shock were also observed. The other patients exhibited no complications during the follow-up period.
Conclusions
Our experience demonstrated a low complication rate associated with removing the thin margins of the residual cavity and changing the shape of it into a “saucer.” The results were satisfactory and comparable to the results of other studies on pulmonary hydatid cysts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hydatid disease is still a major health problem in endemic regions such as the Middle East [1–3]. Humans are accidental intermediate hosts for the tapeworm Echinococcus [4]. The lung is the second most common organ affected by this disease [5, 6]. Single unilateral involvement is most common (70–90 %) followed by multiple unilateral or bilateral lung involvement. The cysts are most often located in the right lower lobe of the lung [7–9]. The cysts grow rapidly in the lung because of the high negative pressure and the elasticity of pulmonary tissue.
Several treatment strategies have been suggested for treating uncomplicated or complicated pulmonary hydatid cysts. Although there are medical options, they are mainly reserved for inoperable cases (either because of dissemination of infection or there is a contraindication for surgery). Medical treatment is also used as an adjunct after surgery to avoid relapse [10]. Studies have reported that the use of puncture, aspiration of cyst contents, instillation of scolicidal agent, and reaspiration (PAIR) for pulmonary hydatid cysts is inadequate. Also, PAIR has been associated with more severe complications in patients with pulmonary hydatid disease than when it is applied in patients with hepatic cysts. Surgery thus remains the treatment of choice for many patients with thoracic hydatid cysts [11].
Generally, parenchyma-sparing conservative surgery is preferred over resection. This is especially true in endemic areas as the treated patients may become reinfected in another area of the lung [12, 13]. Despite the difference in surgical methods, they all have three major aims: first, to evacuate completely the cysts and their contents; second, to prevent any contamination or dissemination of cyst products; third, handling the residual cavity while preserving as much of the functioning lung parenchyma as possible [6, 14].
One method for evacuating the cyst is enucleation (Ugon method), which involves an incision in the lung parenchyma and completely removing the hydatid cyst. Some authors do not advocate enucleation because of the higher risk of contamination [10]. We believe that with an experienced surgeon with great patience enucleation is possible in almost every case.
Another common technique is aspirating and suctioning the cyst and its fluid and then removing the cyst’s layers (laminated and germinative layers)—“cystotomy.” After removing the cyst, the next problem is handling the residual cavity. A method that has been in use since 1952 is capitonnage, a controversial procedure [11, 14–16]. Recently, various surgical groups have challenged the usefulness of capitonnage [17–19]. They claimed that the only requirement is closure of the bronchial openings. Thus, the alternative technique entails closing the bronchial openings in the cavity floor. This maneuver may reduce the likelihood of air leak and bleeding from suture sites and result in complete lung reexpansion [14]. With this technique, however, the residual cavity may provide foci for infection. Also, its pseudocystic radiologic appearance may suggest cyst recurrence, causing unnecessary surgery. Reducing the depth of the cavity by removing the cavity’s thin margins may resolve this problem. In this article, we report the experience of performing a modified version of uncapitonnage surgery in a population of patients with pulmonary hydatid cysts.
Materials and methods
In this descriptive study, 78 patients with thoracic hydatid cyst disease who had undergone 83 thoracotomy procedures in the Department of Surgery, Imam-Khomeini Training Hospital, Urmia University of Medical Sciences between 2006 and 2011 were studied regarding complications of the procedure. The Scientific and Ethical Review Boards of Urmia University of Medical Sciences (UMSU) approved the study. All patients signed an informed consent for performing this type of surgery.
The age of the subjects ranged from 4 to 70 years. In all, 43 (53.7 %) subjects were male, and 37 (46.2 %) were female.
Almost 63 % of patients lived in rural areas (the West-Azerbaijan province of Iran) and had a history of close contact with livestock. An essential part of rural life in this region is cattle breeding, which poses the risk of exposure to Echinococcus granulosus. The diagnosis was based on the results of physical examination, chest radiography, and thoracic computed tomography (CT). Abdominal ultrasonography was performed in all cases as well. Immunologic tests were not implemented because of the high diagnostic validity of imaging techniques.
Surgical procedure
A single surgeon performed all of the surgical procedures. For bilateral lung involvement, a two-step surgical intervention (3-month interval) was performed, prioritizing the unperforated (intact) side. If both sides were intact, the surgery was done primarily on the larger cyst. We did not operate on both lungs during the same surgery because we were not sure we could reach the cysts of both lungs via sternotomy. We also wanted to avoid increasing the duration of the surgery.
The operation was conducted under general anesthesia with double-lumen intubation. We used double-lumen intubation for several reasons: First, there is the risk of intrabronchial rupture of an intact cyst during manipulation. Double-lumen intubation would keep the contralateral lung safe from any contamination. Second, there are reports that intrabronchial rupture of the cyst might result in asphyxiation during the surgery if sizable pieces of laminated membrane become impacted in the trachea. Third, it would be more convenient to deliver the cyst to the field of surgery with the intact lung collapsed.
All of the patients underwent posterolateral thoracotomy. Pneumolysis was done subsequently. After adequately exposure of the involved lobe, the surrounding area was covered with sponges moistened with 5 % saline solution to prevent implantation of scolices or daughter cysts. The operative technique depended on the size and integrity of the cyst. For intact cysts, our preference is enucleation.
For enucleation, a no. 15 scalpel was used to make an incision in the pericyst over the cyst. The pericyst was removed to the periphery with a tin-tip hemostat. This was performed at several sites until the cyst was removed completely. During the enucleation, if the laminated membrane was torn, we aborted the enucleation procedure and performed cystotomy.
For cystotomy, after covering the operative field with saline-soaked towels, a 12-gauge needle that connected to a suction apparatus was inserted into the cyst. Aliquots of 20 cc of cyst contents were aspirated and 20 cc hypertonic saline solution was injected into the cyst. This maneuver was repeated until the contents of the cyst were completely aspirated, usually after 10 min. During this process, fluid leaking from the needle insertion site was suctioned continuously with separate suction.
In the cases of perforated cysts, the pericyst was opened with electrocautery. After aspirating the residual fluid, the membrane of the cyst was removed completely.
Handling the pericyst
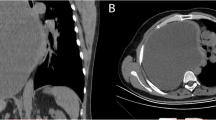
After evacuating the cyst, the thin marginal parts of the pericyst were removed using electrocautery. Thus, the depth of the cavity was reduced, and the socket was converted into the shape of a saucer (saucerization) (Fig. 1). This provided us enough space to close the bronchial openings. The bronchial openings were closed with 4-0 Vicryl and figure-of-eight stitches. To ascertain pneumostasis, the floor of the “saucer” was filled with normal saline, and the airway pressure was elevated to 30 cm H2O. Any bleeding from the periphery of the new cavity was controlled with electrocautery or another stitch with chromic suture.
The hemithorax cavity was irrigated with normal saline solution. After inserting one or two chest tubes—one in the posterior and the other in the upper pleural spaces to drain blood or air—the chest was closed using the standard approach.
All patients, apart from the intact or ruptured nature of their cyst, underwent medical therapy with albendazole (10 mg/kg per day) beginning at the time of the clinical diagnosis of hydatidosis (considering the endemicity of hydatidosis in the northwestern region of Iran) and continuing throughout the postoperative period. The albendazole therapy was discontinued after 3 months in patients with an intact cyst. For those with a perforated cyst, however, the medical therapy continued for 6 months following the operation.
Results
A total of 78 patients were enrolled in this study. Patients presented most frequently with cough (70 %), dyspnea (65 %), and chest pain (43 %). Other symptoms were expectoration, fever, and hemoptysis. None of the patients presented with an allergic reaction. Ten patients were asymptomatic, with the thoracic hydatid cyst diagnosed accidentally via chest radiography performed for other reasons.
According to the imaging, 92.5 % had unilateral involvement (right-sided in 48.7 %, left-sided in 43.7 %), and 7.6 % (six patients) had bilateral involvement. One subject had a mediastinal cyst. The right lower lobe was most frequently involved (Table 1).
The cysts were intact in 57 patients, but in 23 cases (29.4 %) it had perforated to the bronchus (9 cases) or pleural cavity (15 cases). Cystotomy was done in all patients with perforated lung hydatid cysts (Table 2). The preoperative diagnosis was different from the final, confirmed diagnosis in only one case. The patient was a woman who was referred with hemoptysis. Thoracic CT demonstrated a mass in the left upper lobe. Preoperative bronchoscopy revealed only bleeding from the left upper lobe. We performed lobectomy in this case as well as in another case in which almost 50 % of the right lower lobe was destroyed.
In six patients with bilateral involvement, we performed the second thoracotomy 3 months after the first surgery. In all, 11 patients had concurrent liver hydatid cysts. In six of these patients, the hepatic cyst was operated on at the same surgery as the pulmonary cyst.
Postoperative phase
All patients were admitted to the intensive care unit (ICU) after surgery. The length of stay in the ICU ranged from 1 to 9 days. The only death among our subjects occurred in a 60-year-old man who was operated on because of a ruptured pulmonary hydatid cyst. Empyema was detected during the operation, and decortication was performed apart from the cyst resection. Weaning from the mechanical ventilator was unsuccessful, and the patient became septic on postoperative day 5. He died from septic shock 3 days later.
Incomplete lung expansion was the main postoperative complication, occurring in six subjects. Each was treated with conservative therapy, including physiotherapy, insertion of an additional chest tube, or fiberoptic bronchoscopy. Persistent air leak (≥7 days) occurred in a 7-year-old girl. It was finally resolved by physiotherapy and suction. Wound infection was observed in four patients.
Our follow-up examinations were scheduled for 1 week after discharge, each month for 3 months (physical examination + chest radiography and CT scan if needed) in patients with an intact cyst. For those with a perforated cyst, it was the same protocol but every month for 6 months, then every 3 months until the end of the first postoperative year. They were then scheduled for annual visits that included a physical examination.
We lost 5 of the 78 subjects to follow-up. All others were followed for at least 6 months (range 6–60 months). No allergic reactions were observed, and there were no recurrences. In one subject, a hydatid cyst was later found in the contralateral lung. Another patient came to the emergency department 7 months after operation complaining of dyspnea. Chest radiography revealed pneumothorax in the operated hemithorax, which was resolved by chest tube insertion.
Another patient was referred to the emergency department because of dyspnea 13 months after surgery. Chest radiography demonstrated collapse of the operated lung. Chest tube insertion led to partial lung expansion. The patient had persistent air leak because of a bronchopleural fistula. The problem was finally resolved by performing a right upper lobectomy.
Discussion
In our study, 12.8 % of the patients with a pulmonary hydatid cyst were asymptomatic. The rate of asymptomatic cases has been variously reported at 10–20 % [12, 13, 20]. The rate of bilateral lung involvement is reportedly 4.3–6.5 % [6, 13], whereas in our study 7.6 % of the subjects had hydatid cysts in both hemithoraces. In most of the cases, the cyst was located in the right lower lobe, which is in accordance with the findings of previous studies worldwide [6, 9, 21].
Perforation of pulmonary hydatid cysts has been reported to be 6.2–48.3 % [9, 15, 22]. The rate in our study was 29.4 %. We had no recurrences in our study, whereas other studies have reported recurrence rates of 1.5–12.0 %) [23].
Several surgical procedures have been proposed for treating patients with pulmonary hydatid cysts [14]. Several articles have been published in favor or against the use of each of these procedures.
According to the literature, the use of resection should be limited to cases in which there has been additional tissue destruction due to infection [11, 12]. In our study, only two patients had to undergo lobectomy—one because of tissue destruction due to infection and the other because of a complicated pulmonary cyst with a different preoperative diagnosis.
We used cystotomy only if the cyst was perforated. Enucleation was the preferred surgical procedure. Some surgeons do not advocate enucleation because of the higher risk of infection [10]. We believe that a combination of experience and patience can lead to a high success rate when performing the enucleation procedure. Some authors blame cystectomy because of the risk of air leaks and postoperative bleeding [10].
There is also controversy about the usefulness or uselessness of capitonnage. Some studies have supported capitonnage because of its low complication rate [11]. Others have claimed that capitonnage is useless during surgery for intact lung cysts [8, 17–19] and that it carries the potential risk of pulmonary parenchymal distortion [24]. They suggested that capitonnage interferes with lung expansion [14]: suturing the healthy parenchymal margins to perform capitonnage may damage anatomic structures such as bronchial airways, leading to air leak.
We did not perform capitonnage in any of the patients in this study. We also did not recruit a control group. All of the patients underwent a modified uncapitonnage procedure, called “saucerization,” to deal with the residual cavity after evacuating the cyst. Our results showed a low complication rate for removing the thin margins of the residual cavity and changing its shape so it resembled a “saucer.” The results were completely satisfactory and comparable to the results of other studies on pulmonary hydatid cysts.
In one case (1.2 % of the population), the presurgery diagnosis was not compatible with the final diagnosis. This is in accordance with the literature. Sayir et al. noted that their imaging suggested malignancy in 14 (3.39 %) of 412 subjects. Preoperative fiberoptic bronchoscopy was unable to confirm the diagnosis in nine of them [6]. Because there is always a possibility of preoperative misdiagnosis, all avenues should be considered to ensure that the most appropriate surgical method is chosen.
Conclusions
Saucerization is a procedure by which the thin margins of the pericyst are removed after evacuating the hydatid cyst. This maneuver converts the residual cavity into a saucer-like construct. The procedure was associated with a low complication rate in our study population.
References
Rebhandl W, Turnbull J, Felberbauer FX et al (1999) Pulmonary echinococcosis (hydatidosis) in children: results of surgical treatment. Pediatr Pulmonol 27:336–340
Santivanez S, Garcia HH (2010) Pulmonary cystic echinococcosis. Curr Opin Pulm Med 16:257–261
Sokouti M, Golzari S, Aghdam BA (2011) Surgery of uncomplicated pulmonary hydatid cysts: Capitonnage or uncapitonnage? Int J Surg 9:221–224
Morar R, Feldman C (2003) Pulmonary echinococcosis. Eur Respir J 21:1069–1077
Koksal C, Baysungur V, Okur E et al (2006) A two-stage approach to a patient with hydatid cysts inside the right pulmonary artery and multiple right lung involvement. Ann Thorac Cardiovasc Surg 12:349–351
Sayir F, Cobanoğlu U, Sehitoğulları A et al (2012) Our eight-year surgical experience in patients with pulmonary cyst hydatid. Int J Clin Exp Med 5:64–71
Aytac A, Yurdakul Y, Ikizler C et al (1977) Pulmonary hydatid disease: report of 100 patients. Ann Thorac Surg 23:145–151
Ayuso LA, de Peralta GT, Lazaro RB et al (1981) Surgical treatment of pulmonary hydatidosis. J Thorac Cardiovasc Surg 82:569–575
Doğan R, Yüksel M, Cetin G et al (1989) Surgical treatment of hydatid cysts of the lung: report on 1,055 patients. Thorax 44:192–199
Yalçinkaya İ, Er M, Özbay B et al (1999) Surgical treatment of hydatid cyst of the lung: review of 30 cases. Eur Respir J 13:441–444
Bilgin M, Oguzkaya F, Akcali Y (2004) Is capitonnage unnecessary in the surgery of intact pulmonary hydatic cyst? ANZ J Surg 74:40–42
Burgos R, Varela A, Castedo E et al (1999) Pulmonary hydatidosis: surgical treatment and follow-up of 240 cases. Eur J Cardiothorac Surg 16:628–635
Hasdiraz L, Oğuzkaya F, Bilgin M (2006) Is lobectomy necessary in the treatment of pulmonary hydatid cysts? ANZ J Surg 76:488–490
Nabi MS, Waseem T (2010) Pulmonary hydatid disease: What is the optimal surgical strategy? Int J Surg 8:612–616
Kosar A, Orki A, Haciibrahimoglu G et al (2006) Effect of capitonnage and cystotomy on outcome of childhood pulmonary hydatid cysts. J Thorac Cardiovasc Surg 132:560–564
Yaldiz S, Gursoy S, Ucvet A et al (2012) Capitonnage results in low postoperative morbidity in the surgical treatment of pulmonary echinococcosis. Ann Thorac Surg 93:962–966
Erdogan A, Ayten A, Demircan A (2005) Methods of surgical therapy in pulmonary hydatid disease: Is capitonnage advantageous? ANZ J Surg 75:992–996
Eren MN, Balci AE, Eren S (2005) Non-capitonnage method for surgical treatment of lung hydatid cysts. Asian Cardiovasc Thorac Ann 13:20–23
Turna A, Yilmaz MA, Haciibrahimoğlu G et al (2002) Surgical treatment of pulmonary hydatid cysts: Is capitonnage necessary? Ann Thorac Surg 74:191–195
Safioleas M, Misiakos EP, Dosios T et al (1999) Surgical treatment for lung hydatid disease. World J Surg 23:1181–1185. doi:10.1007/s002689900643
Mesbahi S (1992) Radiological investigation of pulmonary hydatid cyst in 71 patients. Med J Tabriz Univ Med Sci Health Serv 26:106–113
Kavukcu S, Kilic D, Tokat AO et al (2006) Parenchyma-preserving surgery in the management of pulmonary hydatid cysts. J Invest Surg 19:61–68
Mottaghian H, Saidi F (1978) Postoperative recurrence of hydatid disease. Br J Surg 65:237–242
Sarsam A (1971) Surgery of pulmonary hydatid cysts: review of 155 cases. J Thorac Cardiovasc Surg 62:663–668
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mahmodlou, R., Sepehrvand, N. & Nasiri, M. Saucerization: A Modified Uncapitonnage Method of Surgery for Pulmonary Hydatidosis. World J Surg 37, 2129–2133 (2013). https://doi.org/10.1007/s00268-013-2093-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2093-7