Abstract
Background
Some patients develop troublesome dysphagia after laparoscopic antireflux surgery, and a proportion require further intervention. The management of this problem was evaluated.
Methods
Patients who underwent intervention for dysphagia after laparoscopic fundoplication were identified from a database. Outcomes were prospectively determined from a standardized questionnaire that evaluated symptoms scores for dysphagia for solids and liquids, as well as patient satisfaction with the overall outcome. Outcomes 1 year after reintervention, and at the most recent follow-up were evaluated.
Results
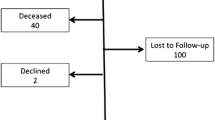
From 1994 to 2009, 121 (6.6%) of 1,821 patients who underwent laparoscopic fundoplication for gastroesophageal reflux also underwent endoscopic or surgical reintervention for dysphagia. Of these 121 patients, 56 underwent endoscopic dilatation, and 24 were satisfied with the outcome of dilatation; 18 progressed to surgery, and dysphagia persisted in 14 of them. Overall, 83 patients underwent revisional surgery, and 47 (62.7%) were satisfied with the outcome. Compared to patients who did not undergo any intervention for dysphagia, patients who underwent reintervention had lower satisfaction scores and higher dysphagia scores.
Conclusions
Approximately two thirds of patients with troublesome post-fundoplication dysphagia have a satisfactory outcome following either endoscopic dilatation or revisional surgery. However, approximately one third continue to be troubled by symptoms, despite further intervention.

Similar content being viewed by others
References
Kelly JJ, Watson DI, Chin KF et al (2007) Laparoscopic Nissen fundoplication: clinical outcomes at 10 years. J Am Coll Surg 205:570–575
Watson DI, Pike GK, Baigrie RJ et al (1997) Prospective double-blind randomized trial of laparoscopic Nissen fundoplication with division and without division of short gastric vessels. Ann Surg 226:642–652
O’Boyle CJ, Watson DI, Jamieson GG et al (2002) Division of short gastric vessels at laparoscopic Nissen fundoplication: a prospective double-blind randomized trial with 5-year follow-up. Ann Surg 235:165–170
Yang H, Watson DI, Lally CJ et al (2008) Randomized trial of division versus nondivision of the short gastric vessels during laparoscopic Nissen fundoplication: 10-year outcomes. Ann Surg 247:38–42
Sgromo B, Irvine LA, Cuschieri A, Shimi SM (2007) Long-term comparative outcome between laparoscopic total Nissen and Toupet fundoplication: symptomatic relief, patient satisfaction and quality of life. Surg Endosc 22:1048–1053
Watson DI, Jamieson GG, Pike GK et al (1999) Prospective randomized double-blind trial between laparoscopic Nissen fundoplication and anterior partial fundoplication. Br J Surg 86:123–130
Engstrom C, Lonroth H, Mardani J et al (2007) An anterior or posterior approach to partial fundoplication? Long-term results of a randomized trial. World J Surg 31:1221–1225. doi:10.1007/s00268-0007-9004-8
Stewart GD, Watson AJ, Lamb PJ et al (2004) Comparison of three different procedures for antireflux surgery. Br J Surg 91:724–729
Guerin E, Betroune K, Closset J et al (2007) Nissen versus Toupet fundoplication: results of a randomized and multicenter trial. Surg Endosc 21:1985–1990
Ackroyd R, Watson DI, Majeed AW et al (2004) Randomized clinical trial of laparoscopic versus open fundoplication for gastro-oesophageal reflux disease. Br J Surg 91:975–982
Triponez F, Dumonceau J-M, Azagury D et al (2005) Reflux, dysphagia, and gas bloat after laparoscopic fundoplication in patients with incidentally discovered hiatal hernia and in a control group. Surgery 137:235–242
Pessaux P, Arnaud J-P, Delattre JF et al, for the Association Française de Chirurgie (2005) Laparoscopic antireflux surgery: five years results and beyond in 1340 patients. Arch Surg 140:946–951
Malhi-Chowla N, Gorecki P, Bammer T et al (2002) Dilation after fundoplication: timing, frequency, indications and outcome. Gastrointest Endosc 55:219–223
Ravi N, Al-Sarraf N, Moran T et al (2005) Acid normalization and improved esophageal motility after Nissen fundoplication: equivalent outcomes in patients with normal and ineffective esophageal motility. Am J Surg 190:445–450
Gaudric M, Sabate JM, Artru P et al (1999) Results of pneumatic dilatation in patients with dysphagia after anti-reflux surgery. Br J Surg 86:1088–1091
Mardani J, Lundell L, Engström C (2011) Total or posterior partial fundoplication in the treatment of GERD: results of a randomized trial after 2 decades of follow-up. Ann Surg 253:875–878
Lamb PJ, Myers JC, Jamieson GG et al (2009) Long-term outcomes of revisional surgery following laparoscopic fundoplication. Br J Surg 96:391–397
Beck PE, Watson DI, Devitt PG et al (2009) Impact of gender age on the long-term outcome of laparoscopic fundoplication. World J Surg 33:2620–2626. doi:10.1007/s00268-009-0216-y
Yau P, Watson DI, Devitt PG et al (2000) Early reoperation following laparoscopic antireflux surgery. Am J Surg 179:172–176
Acknowledgments
The authors are grateful to their colleagues from the Royal Adelaide Hospital and Flinders Medical Centre who contributed clinical cases to the database. Tanya Irvine and Lorelle Smith supported this study data entry and data extraction.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, H., Meun, C., Sun, X. et al. Outcome Following Management of Dysphagia after Laparoscopic Anti-reflux Surgery. World J Surg 36, 838–843 (2012). https://doi.org/10.1007/s00268-011-1416-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-011-1416-9