Abstract
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of serious fungal infections continues to increase in both the immunocompetent and immunocompromised patient populations [1–7]. Among the broad spectrum of invasive candidal diseases, Candida peritonitis is one of the most common manifestations of infection [8–10]. Peritonitis, an inflammation of the peritoneal lining of the abdomen usually secondary to infection, is a particular problem among surgical patients with hollow viscus perforation or those with intra-abdominal surgical drains [1, 11, 12]. The recovery of bacteria along with Candida in peritoneal fluid samples in these patients is an increasingly common occurrence that raises questions about the role of Candida as a pathogen, co-pathogen, or an innocent bystander in the disease process [12–15].
Overall, fungal peritonitis accounts for approximately 12% of all cases of peritonitis, but the rate can be much higher [16, 17]. The most common cause of fungal peritonitis is Candida, whereas intra-abdominal infections with other fungi, such as Aspergillus, Paecilomyces, Penicillium, and Zygomycetes, are relatively rare [17, 18]. The most common species of Candida that causes intra-abdominal infections is C. albicans, but a shift toward non-albicans Candida, such as C. parapsilosis, C. glabrata, C. tropicalis, C. krusei, and C. lusitaniae, with reduced susceptibility to commonly used antifungal agents was recently observed [7, 11, 17, 19–23].
Left untreated, Candida peritonitis can lead to systemic infection, multiorgan failure, and death. The mortality of Candida peritonitis is very high and has been estimated between 20 and 70% [1, 14, 19]. Despite this, there is still debate about the significance of positive peritoneal fungal cultures and whether antifungal therapy should be started [24]. Adding to the debate is the fact that patients with Candida peritonitis often die of complications of infection even with antifungal therapy [25–27]. Furthermore, there is very little published research on this topic. It is, therefore, important to address the role of Candida in patients with peritonitis secondary to polymicrobial infections. The purpose of this review was to present the latest research on secondary Candida peritonitis in the context of polymicrobial infections and the latest in diagnosis and treatment to guide clinicians in the management of such infections. Candida peritonitis associated with peritoneal dialysis is not within the scope of this article.
Epidemiology
Peritonitis is classified as primary, secondary, or tertiary [8]. Primary peritonitis is spontaneous peritonitis with no apparent breach in the gastrointestinal (GI) tract [28]. Secondary peritonitis, the most common form of Candida peritonitis, is a local infectious process within the abdominal cavity with a distinct cause. It generally occurs as a result of GI tract pathology, allowing translocation of micro-organisms across the bowel wall, perforation of a hollow viscus, an abscess within the abdominal cavity, instrumentation of the GI tract, or GI tract surgery [8]. Tertiary peritonitis usually refers to refractory peritonitis following generally adequate pharmacological and surgical treatment for secondary peritonitis [8, 10].
Candida is one of the leading pathogens isolated in secondary and tertiary peritonitis [8, 17, 29–31]. Candida spp. are involved in an estimated 40–45% of secondary nonappendicitis peritonitis [32]. The distinction between community-acquired versus nosocomial Candida peritonitis also is important and is discussed more below. Nosocomial infections are defined as Candida peritonitis that becomes evident ≥48 h after admission and are an independent risk factor of mortality [25].
Risk factors
The natural flora of the gastrointestinal tract is polymicrobial, and the main organisms are Gram-negative and anaerobic bacteria. Primary invasive organisms of the gastrointestinal tract include Escherichia coli and Bacteroides fragilis [33]. Candida spp. are well-established gut commensals [34]. Under certain conditions, Candida can heavily colonize the digestive tract, invade the mucosa, and spread locally or disseminate distantly [35]. Factors that influence this colonization and infection are outlined in Table 1. Clinical and surgical risk factors for Candida peritonitis are outlined in Tables 2 and 3, respectively.
Overall the two main risk factors that predispose patients to infections with Candida spp. include: (1) colonization of skin and mucous membranes; and (2) breaches in natural host defenses, such as through surgery, loss of integrity of skin, mucosal barriers and gut epithelium, and insertion of intravascular and urinary catheters and surgical drains [11, 36]. Surgery is a major risk factor for Candida peritonitis for several reasons: (1) there are direct breaches in natural barriers of defense; (2) in the case of GI surgery there is direct soiling of the intra-abdominal compartment; (3) patients often require intravascular and urinary catheters and surgical drains; (4) patients often require resting of the GI tract and total parenteral nutrition (TPN), which causes villous atrophy and translocation of bacteria and fungi; and (5) patients may develop hemorrhagic shock, which leads to gut ischemia and bacterial and fungal translocation across the gut wall [17, 24, 25, 27, 37, 38]. The latter is why thoracic surgery is a risk factor for Candida peritonitis; a decrease in blood pressure during surgery causes GI tract hypoperfusion resulting in gut ischemia, compromise, and translocation of fungi and bacteria. Studies have shown that secretory IgA, a principle immunologic defense at the gut mucosal surface, may be depleted by TPN, bowel rest, steroids, hemorrhagic shock, and microbial degradation facilitating microbial translocation across the gut wall [39–41].
In a study of 49 patients who had spontaneous hollow viscus perforation or surgical opening of the GI tract and positive Candida cultures of intra-abdominal specimens, Candida caused infections in 19 patients (39%) [27]. Of these patients, 7 had intra-abdominal abscesses and 12 peritonitis. Candida was more likely to cause infection in those patients who had surgery for acute pancreatitis than other surgical conditions. Importantly, the overall mortality was much higher in those with intra-abdominal candidal infections (7/19 patients, 37%) than in surgical patients without such infection. One notable result from this study was that Candida was more likely to be isolated in peritoneal fluids samples when the source of infection was the upper GI tract than when it was the lower GI tract. The outcome also was worse for the former. These results were similar in several other studies [17, 24, 37, 38]. An upper GI tract site of infection was found to be independent risk factor of mortality in nosocomial Candida peritonitis [25]. Interestingly, Spanakis et al. found that statin use correlated with decreased positive cultures (blood, sputum, urine, peritoneal fluid) among patients with type 2 diabetes mellitus who underwent lower GI surgery [42].
Surgical patients often are transferred to intensive care units (ICU) where despite constant improvements in standards of care, there is still a high mortality attributed to intra-abdominal sepsis [14]. Yeasts are isolated in 5–22% of peritoneal samples in this setting with an overall increase in mortality as high as 70% [11, 14, 15, 26, 30]. Studies have shown high rates of Candida colonization, up to 64%, and infection in surgical ICU patients with higher mortality in colonized patients [35, 43]. Independent risk factors of yeast isolation in peritoneal fluid samples in this patient group include: female gender; mechanical ventilation; ventilator-associated pneumonia; bacteremia; surgical complications; an upper GI tract source of infection; intraoperative cardiovascular failure; previous antimicrobial therapy ≥48 h before the onset of peritonitis; laparotomy; TPN; diabetes mellitus; immunosuppression; and body temperature >38.2°C [14, 21, 25, 44]. The key outcome of these studies is that they identify groups of critically ill patients in which antifungal prophylaxis may be beneficial [45].
Pathogenicity
Bacteria can influence fungal growth, physiology, and pathogenicity directly or indirectly, and fungi can do the same to bacteria [46–55]. Several studies have shown increased mortality with dual infections with C. albicans and E. coli [46, 54, 56]. Sawyer et al. examined the role of C. albicans in the pathogenesis of mixed fungal and bacterial peritonitis in murine models and whether these infectious elements were synergistic, competitive, or neutral [12]. The authors developed murine models of peritonitis with abscess formation and a high mortality with C. albicans, E. coli, and B. fragilis alone or in combination as part of a polymicrobial infection. Components of each system were eliminated with directed antimicrobial therapy. The results showed that both C. albicans and bacteria contributed to mortality in mixed infections and treatment with both bacterial and fungal antimicrobial agents increased survival from 50 to 90%. With regards to abscess formation, C. albicans, E. coli, and B. fragilis caused parallel infections that were not synergistic and had no effect on the growth of the other species. Similar studies in mice, however, have shown that there is some bacterial–fungal synergistic effect on mortality [55, 57]. This synergy is species-specific and did not occur in similar murine models using C. albicans and Staphylococcus aureus, Serratia marcescens, or Enterococcus faecalis [57–63].
Unfortunately, we still do not know the factors that transform Candida into a pathogen in this setting. There is an exciting area of research into the role of Candida spp. in polymicrobial infections and, in particular, the ability of Candida spp. to modulate the virulence of bacteria during coinfection [46, 47, 64, 65]. Work done so far indicates that during Candida coinfection with bacteria, especially Gram-negative pathogens, such as Pseudomonas aeruginosa, Acinetobacter baumannii, and Salmonella enterica serovar Typhimurium, there is a pathogen–pathogen interaction that centers on quorum-sensing molecules of Candida and bacteria [66, 67]. This interaction may augment bacterial virulence during peritonitis, in a similar way that it has been theorized during Pseudomonas pneumonia [68].
Diagnosis
The clinical picture is usually indistinguishable from that of bacterial sepsis, especially when early blood cultures are negative for fungi or return positive late in the course of disease. For that reason, it is important to have a high index of suspicion of fungal superinfection in the presence of sepsis, especially when symptoms of sepsis persist despite antibiotic therapy [69]. Nonspecific elements of clinical picture suggestive of Candida peritonitis include high fever, rigors, diaphoresis, hypotension, and adynamic ileus (Table 4) [8].
Laboratory findings include leukocytosis with neutrophilia, high C-reactive protein (CRP), high procalcitonin, purulent exudates, and positive peritoneal fluid cultures with budding fungi on microscopy [8, 70–73]. Interestingly, procalcitonin seems to have a higher specificity and sensitivity as a marker of infection compared with CRP [70–72].
Histopathological diagnosis in tissue samples or growth of Candida in culture media is still considered the “gold standard” for diagnosis [74]. Blood, peritoneal fluid, and fluid from indwelling drains should be sent for microscopy and fungal culture [1]. Fungal cultures, however, take more than a week to yield results. Perioperative isolation of Candida in body fluid or tissue samples has higher clinical significance than isolation from postoperative drains [3]. Importantly, cases of disseminated candidiasis with negative blood cultures have been reported in patients on systemic antifungal agents or steroids, as well as cases of abdominal candidiasis with negative peritoneal fluid cultures [75].
Serological assays can be useful to screen for invasive candidal infections, but their sensitivity and specificity are variable [76]. They involved detection of antibodies against highly immunogenic fungal cell wall components, such as 1 → 3 β-d-Glucan (BDG), galactomannan, and mannan [74, 77–81]. BDG and galactomannan are nonspecific markers of fungal infection that are positive in other fungal infections [74, 77]. The Candida anti-mannan antibody assay may be more specific for the diagnosis of Candida infection [77].
Serological assays may be combined with deoxyribonucleic acid (DNA) detection methods to improve their sensitivity and specificity [77]. Highly sensitive and specific assays using DNA genomic amplification by polymerase chain reaction (PCR) have been developed to detect Candida infections with good results [33, 77, 82, 83]. The average time for detection and speciation is just more than 2 days. A specialized semi-nested PCR (snPCR) improves sensitivity by ten times with the detection limit <10 yeast cells compared with a genus-specific PCR [33]. DNA microarray chip technology, consisting of oligonucleotide probes fixed on a solid support using photolithographic methods, also can be used for C. albicans detection [84, 85].
A new diagnostic tool for Candida detection is mass spectrometry. Raman spectroscopy can identify Candida strains with 90% accuracy within 12–24 h [86]. Matrix-assisted laser desorption ionization-time of flight (MALDI-TOF) is a very promising experimental mass spectrometry assay that can identify fungi in approximately 1 h, but currently has limitations (discussed in [87–89]).
Treatment
The treatment of Candida peritonitis includes conservative, medical, and surgical measures (Table 4). Conservative measures include removal of all foreign bodies, such as intravascular and urinary catheters, drains, and prosthetic materials, because fungi can colonize these materials and form biofilms [2, 9, 18, 19]. Removal of peritoneal catheters can be delayed for peritoneal lavage with antimycotics via these catheters [19, 90]. Surgical measures, such as identifying and draining visceral abscesses, are essential for the treatment of secondary peritonitis [1, 91].
In general, there are four classes of antifungal agents used in the medical management of Candida peritonitis: polyenes (deoxycholate and liposomal formulations of amphotericin B); azoles (fluconazole, itraconazole and the newer extended spectrum voriconazole and posaconazole); echinocandins (caspofungin, micafungin, and anidulafungin); and flucytosine [8, 92–101]. While selecting antifungal agents, clinicians should consider severity of the illness, the length of stay in the hospital, the type of peritonitis, recent exposure to antifungal agents, the resistance profile of the Candida species involved, relevant comorbid conditions (such as renal, liver, and bone marrow failure), and evidence of CNS, cardiac valve, and visceral organ involvement [94, 95, 102, 103].
The azoles are fungistatic against most Candida spp., whereas the polyenes and echinocandins are fungicidal [98]. Fluconazole is recommended for patients with community-acquired Candida peritonitis, no prior azole exposure, and those not at high risk of infection with fluconazole-resistant strains (such as C. krusei and C. glabrata) [104–106]. These high-risk patients include the elderly, diabetic, and cancer patients [8, 19, 94]. With good oral bioavailability and peritoneal penetration, fluconazole can be used orally or intravenously [19]. Fluconazole is popular because of its good side-effect profile and consequently resistance Candida strains are common [21, 94]. Empiric therapy with fluconazole is not recommended for most mild-to-moderate community-acquired cases of peritonitis, except in neonates where Candida infection is suspected [107]. A cumulative stay in hospital ≥29 days is a strong predictor for the isolation of nonfluconazole-susceptible Candida isolates among critically ill emergency surgery patients [103]. For high-risk patients with clinical suspicion of Candida peritonitis, culture confirmation is not necessary and treatment should commence promptly [1, 107]. If there is no detectable Candida in peritoneal fluid samples, the decision to treat should be based on clinical findings and risk factors combined with other variables. Overall, it is important to treat early to prevent dissemination of infection and to continue surveillance of blood cultures (and if they are positive, evaluate the patient for Candida endophthalmitis) [101, 108].
In a joint meeting between the American Surgical Infection Society (SIS) and the Infection Diseases Society of America (IDSA), echinocandins were recommended for patients infected with fluconazole-resistant species of Candida and those who were critically ill [107, 109]. Some centers recommend the use of echinocandins from the outset in patients with moderate-to-severe disease and those with prior azole exposure [94]. The echinocandins have a high clinical efficacy and good side-effect profile, making them another attractive option for treating Candida peritonitis [89, 94]. These antifungals have been used with success, especially for the treatment of non-albicans Candida, which can have a high resistance to triazoles [89].
With regards to the polyene antifungals, amphotericin B can be given intravenously, but it is highly protein bound resulting in poor penetration of the peritoneum [19, 110]. Peritoneal lavage with amphotericin B can be used, but it can cause peritoneal irritation leading to abdominal pain [19]. Amphotericin B also is associated with renal toxicity (liposomal formulations of amphotericin B have less renal toxicity) and electrolyte abnormalities [1, 2].
Flucytosine has good peritoneal penetration with oral administration [19]. It must be used in combination with other antifungal agents because the risk of resistance is high [19, 110]. Some centers use amphotericin B and flucytosine as first-line agents [19, 111]. Fluconazole and flucytosine can be used in combination for peritoneal lavage when intra-abdominal catheters cannot be removed [19]. Flucytosine is hepatotoxic and causes bone marrow toxicity; therefore, its use is contraindicated in patients with bone marrow depression or hematological disease and patients taking other drugs that suppress bone marrow [19]. Its use necessitates therapeutic drug monitoring and regular monitoring of full blood count and liver function tests.
Of the newer extended-spectrum triazoles, voriconazole and posaconazole are the only two currently available for use [92, 94–96]. The newer triazoles have improved safety profiles and a broad spectrum of activity, making them attractive choices for treatment [92–97, 99, 100]. Voriconazole has intravenous and oral preparations, whereas posaconazole is only effective when given orally [19]. Although well tolerated, voriconazole can cause hepatotoxicity, adverse visual events, and rashes [19]. Posaconazole can be used as salvage therapy for refractive infections and in rare cases can cause hepatotoxicity [19, 92, 96, 97]. For Candida strains with increased resistant to azoles, such as C. glabrata and C. krusei, echinocandins or preparations of amphotericin B can be used as alternatives [2]. C. parapsilosis and C. guilliermondii are less susceptible to echinocandins, and C. lusitaniae can be resistant to amphotericin B [95, 96]. The efficacy of the new extended spectrum triazoles has not been studied in detail against these Candida strains [95, 96].
Most experts agree that the duration of antifungal treatment should be continued for a minimum of 2 weeks after documented clearance in peritoneal fluid or blood samples [94]. Patients are likely to improve within a day or two of starting antifungal therapy. If there is a lack of improvement within 3–4 days of starting antifungal agents, therapeutic failure must be considered. Therapeutic failures can be defined as the lack of clinical resolution of symptoms and signs, persistent positive fungal cultures from peritoneal fluid samples or blood cultures, and persistently raised makers of inflammation, such as neutrophilia and raised C-reactive protein. Treatment must then be escalated by moving to second-line agents, combination therapy, or imaging and surgical exploration. Antifungal susceptibility should always guide the choice of antifungal agents.
Outcome
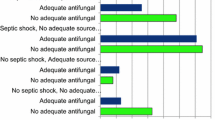
The outcome of Candida peritonitis is variable. The risk factors associated with increased mortality in Candida peritonitis include: extremes of age; Candida cultured in peritoneal fluid samples; candidemia; upper GI tract source of infection; patient comorbidities, such as cardiac insufficiency, cirrhosis, and diabetes mellitus; respiratory failure; renal failure before initiation of treatment; uncontrolled undrained infections; high APACHE II score; and multiorgan failure [8, 18, 25, 26, 31, 37, 86, 91]. The most important risk factor of mortality is isolation of Candida from peritoneal fluid samples and an upper GI source of infection [37]. In general, if Candida is detected on direct examination of peritoneal fluid, the outcome is worse. In one study, the attributable mortality of candidemia and Candida peritonitis was 37% with an overall mortality of 57% [1]. The attributable mortality of Candida peritonitis in surgical patients was 37% in this study. The mortality rate in patients with Candida peritonitis is high despite treatment with antifungal agents, but this is likely because treatment is started late [25]. There is evidence to suggest that patients with nosocomial Candida peritonitis have a higher mortality rate compared with patients with community-acquired Candida peritonitis [25].
Prophylaxis
Prevention against fungal infection starts with conservative measures, such as good hygiene, hand washing, and hospital infection control measures [2]. Pharmacological prophylaxis also is important in some patients. Fluconazole is currently the drug of choice for prophylaxis against Candida infection, especially for high-risk patients [2]. Caspofungin also has been used with some success [112, 113]. However, when to start prophylaxis and the duration of therapy needs to be determined and the results thus far are mixed [22, 45].
Published systematic reviews on the effects of fluconazole prophylaxis in non-neutropenic critically ill adult patients showed significantly reduced invasive fungal infections [113–115]. In some cases, a shift to triazole-resistant Candida strains was observed, such as C. krusei [116].
A policy of antifungal prophylaxis based on risk-factors alone can lead to an extensive use of prophylaxis and the selection of resistant strains of Candida [45]. Risk factors must be combined with other variables to determine in which patients to start antifungal prophylaxis. Special consideration is given to ICU patients who are heavily colonized with Candida spp. Using Candida colonization scores may help to determine patients who should receive antifungal prophylaxis [22, 45]. One such scoring system, the “Candida score,” was developed to determine when to initiate antifungal treatment in non-neutropenic critically ill patients with Candida colonization by using surveillance of urine, tracheal, and gastric samples [117]. A Candida score of >2.5 accurately predicted patients who would benefit from early antifungal treatment, including patients on TPN, those who had undergone recent abdominal surgery, and those with severe sepsis. Of note, central venous catheters were not a risk factor for invasive Candida infection.
Conclusions
Candida peritonitis is important because of its increasing incidence and high mortality rate. Although C. albicans is the most common yeast causing Candida peritonitis, a shift to non-albicans strains, which are increasingly drug-resistant has been observed. The most common species causing Candida peritonitis include C. albicans, C. parapsilosis, C. glabrata, C. tropicalis, and C. krusei. The interpretation of microbiological cultures is difficult, because cultured Candida spp. can represent a contaminant as part of mixed gut flora or a pathogen causing peritonitis. However, isolated Candida spp. must be treated as a pathogen contributing to peritonitis. We still need to study the Candida pathogenesis and the interaction of this pathogen with enteric bacteria. Prompt diagnosis, effective antifungal therapy, and skilled surgical management are an essential component of treatment.
References
British Society for Antimicrobial Chemotherapy Working Party (1994) Management of deep Candida infection in surgical and intensive care unit patients. Intensive Care Med 20:522–528
Edwards JE Jr., Bodey GP, Bowden RA et al (1997) International conference for the development of a consensus on the management and prevention of severe candidal infections. Clin Infect Dis 25:43–59
Eggimann P, Calandra T, Fluckiger U et al (2005) Invasive candidiasis: comparison of management choices by infectious disease and critical care specialists. Intensive Care Med 31:1514–1521
Falagas ME, Apostolou KE, Pappas VD (2006) Attributable mortality of candidemia: a systematic review of matched cohort and case-control studies. Eur J Clin Microbiol Infect Dis 25:419–425
Wenzel RP, Gennings C (2005) Bloodstream infections due to Candida species in the intensive care unit: identifying especially high-risk patients to determine prevention strategies. Clin Infect Dis 41(Suppl 6):S389–S393
Viscoli C, Girmenia C, Marinus A et al (1999) Candidemia in cancer patients: a prospective, multicenter surveillance study by the Invasive Fungal Infection Group (IFIG) of the European Organization for Research and Treatment of Cancer (EORTC). Clin Infect Dis 28:1071–1079
Bassetti M, Righi E, Costa A et al (2006) Epidemiological trends in nosocomial candidemia in intensive care. BMC Infect Dis 6:21
Blot SI, Vandewoude KH, De Waele JJ (2007) Candida peritonitis. Curr Opin Crit Care 13:195–199
Blot S, Vandewoude K (2004) Management of invasive candidiasis in critically ill patients. Drugs 64:2159–2175
Blot S, De Waele JJ (2005) Critical issues in the clinical management of complicated intra-abdominal infections. Drugs 65:1611–1620
Mean M, Marchetti O, Calandra T (2008) Bench-to-bedside review: candida infections in the intensive care unit. Critical Care (Lond) 12:204
Sawyer RG, Adams RB, Rosenlof LK et al (1995) The role of Candida albicans in the pathogenesis of experimental fungal/bacterial peritonitis and abscess formation. Am Surg 61:726–731
Roehrborn A, Thomas L, Potreck O et al (2001) The microbiology of postoperative peritonitis. Clin Infect Dis 33:1513–1519
Dupont H, Bourichon A, Paugam-Burtz C et al (2003) Can yeast isolation in peritoneal fluid be predicted in intensive care unit patients with peritonitis? Critical Care Med 31:752–757
Rex JH (2006) Candida in the peritoneum: passenger or pathogen? Crit Care Med 34:902–903
Sotto A, Lefrant JY, Fabbro-Peray P et al (2002) Evaluation of antimicrobial therapy management of 120 consecutive patients with secondary peritonitis. J Antimicrob Chemother 50:569–576
de Ruiter J, Weel J, Manusama E et al (2009) The epidemiology of intra-abdominal flora in critically ill patients with secondary and tertiary abdominal sepsis. Infection 37:522–527
Petri MG, Konig J, Moecke HP et al (1997) Epidemiology of invasive mycosis in ICU patients: a prospective multicenter study in 435 non-neutropenic patients. Paul-Ehrlich society for chemotherapy, divisions of mycology and pneumonia research. Intensive Care Med 23:317–325
Matuszkiewicz-Rowinska J (2009) Update on fungal peritonitis and its treatment. Perit Dial Int 29(Suppl 2):S161–S165
Gullo A (2009) Invasive fungal infections: the challenge continues. Drugs 69(Suppl 1):65–73
Leroy O, Gangneux JP, Montravers P et al (2009) Epidemiology, management, and risk factors for death of invasive Candida infections in critical care: a multicenter, prospective, observational study in France (2005–2006). Crit Care Med 37:1612–1618
Wang DH, Gao XJ, Wei LQ et al (2009) The preemptive treatment of invasive Candida infection with reference of corrected colonization index in critically ill patients: a multicenter, prospective, randomized controlled clinical study [in Chinese]. Chinese Crit Care Med 21:525–528
Islam S, Zaidi AK, Wilson J (2002) Peritoneal infection with multiple species of Candida: a case report. Surg Infect 3:35–37
Shan YS, Hsu HP, Hsieh YH et al (2003) Significance of intraoperative peritoneal culture of fungus in perforated peptic ulcer. Br J Surg 90:1215–1219
Montravers P, Dupont H, Gauzit R et al (2006) Candida as a risk factor for mortality in peritonitis. Critical Care Med 34:646–652
Solomkin JS, Flohr AB, Quie PG et al (1980) The role of Candida in intraperitoneal infections. Surgery 88:524–530
Calandra T, Bille J, Schneider R et al (1989) Clinical significance of Candida isolated from peritoneum in surgical patients. Lancet 2:1437–1440
Yang C, Yeh CT, Hung CF et al (1999) Case report: spontaneous peritonitis caused by Candida albicans. J Gastroenterol Hepatol 14:1041–1044
Nathens AB, Rotstein OD, Marshall JC (1998) Tertiary peritonitis: clinical features of a complex nosocomial infection. World J Surg 22:158–163. doi:10.1007/s002689900364
Rotstein OD, Pruett TL, Simmons RL (1986) Microbiologic features and treatment of persistent peritonitis in patients in the intensive care unit. Can J Surg 29:247–250
Sawyer RG, Rosenlof LK, Adams RB et al (1992) Peritonitis into the 1990s: changing pathogens and changing strategies in the critically ill. Am Surg 58:82–87
Sandven P, Qvist H, Skovlund E et al (2002) Significance of Candida recovered from intraoperative specimens in patients with intra-abdominal perforations. Crit Care Med 30:541–547
Khan ZU, Mustafa AS (2001) Detection of Candida species by polymerase chain reaction (PCR) in blood samples of experimentally infected mice and patients with suspected candidemia. Microbiol Res 156:95–102
Schulze J, Sonnenborn U (2009) Yeasts in the gut: from commensals to infectious agents. Deutsches Arzteblatt Int 106:837–842
Johnson DW, Cobb JP (2010) Candida infection and colonization in critically ill surgical patients. Virulence 1:355–356
Pittet D, Monod M, Suter PM et al (1994) Candida colonization and subsequent infections in critically ill surgical patients. Ann Surg 220:751–758
Dupont H, Paugam-Burtz C, Muller-Serieys C et al (2002) Predictive factors of mortality due to polymicrobial peritonitis with Candida isolation in peritoneal fluid in critically ill patients. Arch Surg 137:1341–1346; discussion 1347
Lee SC, Fung CP, Chen HY et al (2002) Candida peritonitis due to peptic ulcer perforation: incidence rate, risk factors, prognosis and susceptibility to fluconazole and amphotericin B. Diagn Microbiol Infect Dis 44:23–27
Diebel LN, Liberati DM, Diglio CA et al (1999) Synergistic effects of Candida and Escherichia coli on gut barrier function. J Trauma 47:1045–1050; discussion 1050–1041
Diebel LN, Liberati DM, Dulchavsky SA et al (1997) An in vitro model to assess mucosal immune function and bacterial translocation. J Surg Res 69:178–182
Kilian M, Reinholdt J, Lomholt H et al (1996) Biological significance of IgA1 proteases in bacterial colonization and pathogenesis: critical evaluation of experimental evidence. APMIS 104:321–338
Spanakis EK, Kourkoumpetis TK, Livanis G et al (2010) Statin therapy and decreased incidence of positive Candida cultures among patients with type 2 diabetes mellitus undergoing gastrointestinal surgery. Mayo Clinic Proc 85:1073–1079
Kourkoumpetis T, Manolakaki D, Velmahos G et al (2010) Candida infection and colonization among non-trauma emergency surgery patients. Virulence 1:359–366
Manolakaki D, Velmahos G, Kourkoumpetis T et al (2010) Candida infection and colonization among trauma patients. Virulence 1:367–375
Viale P (2009) Candida colonization and candiduria in critically ill patients in the intensive care unit. Drugs 69(Suppl 1):51–57
Peleg AY, Hogan DA, Mylonakis E (2010) Medically important bacterial-fungal interactions. Nat Rev Microbiol 8:340–349
Peleg AY, Tampakakis E, Fuchs BB et al (2008) Prokaryote-eukaryote interactions identified by using Caenorhabditis elegans. Proc Natl Acad Sci USA 105:14585–14590
Burd RS, Raymond CS, Dunn DL (1992) Endotoxin promotes synergistic lethality during concurrent Escherichia coli and Candida albicans infection. J Surg Res 52:537–542
Ikeda T, Suegara N, Abe S et al (1999) Efficacy of antibacterial drugs in mice with complex infection by Candida albicans and Escherichia coli. J Antibiot (Tokyo) 52:552–558
Neely AN, Law EJ, Holder IA (1986) Increased susceptibility to lethal Candida infections in burned mice preinfected with Pseudomonas aeruginosa or pretreated with proteolytic enzymes. Infect Immun 52:200–204
Roux D, Gaudry S, Dreyfuss D et al (2009) Candida albicans impairs macrophage function and facilitates Pseudomonas aeruginosa pneumonia in rat. Critical Care Med 37:1062–1067
Wang Y, Xu XL (2008) Bacterial peptidoglycan-derived molecules activate Candida albicans hyphal growth. Commun Integr Biol 1:137–139
Xu XL, Lee RT, Fang HM et al (2008) Bacterial peptidoglycan triggers Candida albicans hyphal growth by directly activating the adenylyl cyclase Cyr1p. Cell Host Microbe 4:28–39
Akagawa G, Abe S, Yamaguchi H (1995) Mortality of Candida albicans-infected mice is facilitated by superinfection of Escherichia coli or administration of its lipopolysaccharide. J Infect Dis 171:1539–1544
Klaerner HG, Uknis ME, Acton RD et al (1997) Candida albicans and Escherichia coli are synergistic pathogens during experimental microbial peritonitis. J Surg Res 70:161–165
Gale D, Sandoval B (1957) Response of mice to the inoculations of both Candida albicans and Escherichia coli. I. The enhancement phenomenon. J Bacteriol 73:616–624
Sawyer RG, Adams RB, May AK et al (1995) Development of Candida albicans and C. albicans/Escherichia coli/Bacteroides fragilis intraperitoneal abscess models with demonstration of fungus-induced bacterial translocation. J Med Vet Mycol 33:49–52
Carlson E (1982) Synergistic effect of Candida albicans and Staphylococcus aureus on mouse mortality. Infect Immun 38:921–924
Carlson E (1983) Enhancement by Candida albicans of Staphylococcus aureus, Serratia marcescens, and Streptococcus faecalis in the establishment of infection in mice. Infect Immun 39:193–197
Carlson E, Johnson G (1985) Protection by Candida albicans of Staphylococcus aureus in the establishment of dual infection in mice. Infect Immun 50:655–659
Onderdonk AB, Bartlett JG, Louie T et al (1976) Microbial synergy in experimental intra-abdominal abscess. Infect Immun 13:22–26
Rotstein OD, Kao J, Houston K (1989) Reciprocal synergy between Escherichia coli and Bacteroides fragilis in an intra-abdominal infection model. J Med Microbiol 29:269–276
Rotstein OD, Pruett TL, Simmons RL (1985) Lethal microbial synergism in intra-abdominal infections Escherichia coli and Bacteroides fragilis. Arch Surg 120:146–151
Tampakakis E, Peleg AY, Mylonakis E (2009) Interaction of Candida albicans with an intestinal pathogen, Salmonella enterica serovar Typhimurium. Eukaryot Cell 8:732–737
Hogan DA, Kolter R (2002) Pseudomonas–Candida interactions: an ecological role for virulence factors. Science 296:2229–2232
Kruppa M (2009) Quorum sensing and Candida albicans. Mycoses 52:1–10
De Sordi L, Muhlschlegel FA (2009) Quorum sensing and fungal-bacterial interactions in Candida albicans: a communicative network regulating microbial coexistence and virulence. FEMS Yeast Res 9:990–999
Azoulay E, Timsit JF, Tafflet M et al (2006) Candida colonization of the respiratory tract and subsequent pseudomonas ventilator-associated pneumonia. Chest 129:110–117
Groll AH, Shah PM, Mentzel C et al (1996) Trends in the postmortem epidemiology of invasive fungal infections at a university hospital. J Infect 33:23–32
Whicher J, Bienvenu J, Monneret G (2001) Procalcitonin as an acute phase marker. Ann Clin Biochem 38:483–493
Jemli B, Aouni Z, Lebben I et al (2007) Procalcitonin in invasive candidosis. Ann Biol Clin (Paris) 65:169–173
Charles PE, Castro C, Ruiz-Santana S et al (2009) Serum procalcitonin levels in critically ill patients colonized with Candida spp: new clues for the early recognition of invasive candidiasis? Intensive Care Med 35:2146–2150
Fisgin NT, Aliyazicioglu Y, Tanyel E et al (2010) The value of neopterin and procalcitonin in patients with sepsis. South Med J 103:216–219
Kedzierska A, Kochan P, Pietrzyk A et al (2007) Current status of fungal cell wall components in the immunodiagnostics of invasive fungal infections in humans: galactomannan, mannan and (1 → 3)-beta-d-glucan antigens. Eur J Clin Microbiol Infect Dis 26:755–766
Bayer AS, Blumenkrantz MJ, Montgomerie JZ et al (1976) Candida peritonitis. Report of 22 cases and review of the english literature. Am J Med 61:832–840
Fujita S (2008) Serologic diagnosis of fungal infections. Nippon Rinsho 66:2313–2318
Alam FF, Mustafa AS, Khan ZU (2007) Comparative evaluation of (1, 3)-beta-d-glucan, mannan and anti-mannan antibodies, and Candida species-specific snPCR in patients with candidemia. BMC Infect Dis 7:103
Alexander BD (2002) Diagnosis of fungal infection: new technologies for the mycology laboratory. Transpl Infect Dis 4(Suppl 3):32–37
Nichterlein T, Buchheidt D, Hein A et al (2003) Comparison of glucan detection and galactomannan enzyme immunoassay in gastrointestinal and systemic murine candidiasis. Diagn Microbiol Infect Dis 46:103–108
Odabasi Z, Mattiuzzi G, Estey E et al (2004) Beta-d-glucan as a diagnostic adjunct for invasive fungal infections: validation, cutoff development, and performance in patients with acute myelogenous leukemia and myelodysplastic syndrome. Clin Infect Dis 39:199–205
Ostrosky-Zeichner L, Alexander BD, Kett DH et al (2005) Multicenter clinical evaluation of the (1 → 3) beta-d-glucan assay as an aid to diagnosis of fungal infections in humans. Clin Infect Dis 41:654–659
Khan Z, Mustafa AS, Alam FF (2009) Real-time light cycler polymerase chain reaction and melting temperature analysis for identification of clinically important Candida spp. J Microbiol Immunol Infect 42:290–295
Lau A, Halliday C, Chen SC et al (2009) Comparison of whole blood, serum and plasma for early detection of candidemia by multiplex-tandem PCR. J Clin Microbiol 48:811–816
Garaizar J, Brena S, Bikandi J et al (2006) Use of DNA microarray technology and gene expression profiles to investigate the pathogenesis, cell biology, antifungal susceptibility and diagnosis of Candida albicans. FEMS Yeast Res 6:987–998
White PL, Perry MD, Barnes RA (2009) An update on the molecular diagnosis of invasive fungal disease. FEMS Microbiol Lett 296:1–10
Ibelings MS, Maquelin K, Endtz HP et al (2005) Rapid identification of Candida spp. in peritonitis patients by Raman spectroscopy. Clin Microbiol Infect 11:353–358
van Veen SQ, Claas EC, Kuijper EJ (2010) High-throughput identification of bacteria and yeast by matrix-assisted laser desorption ionization mass spectrometry (MALDI-TOF MS) in routine medical microbiology laboratory. J Clin Microbiol 48:900–907
Marinach-Patrice C, Fekkar A, Atanasova R et al (2010) Rapid species diagnosis for invasive candidiasis using mass spectrometry. PLoS One 5:e8862
Marinach-Patrice C, Lethuillier A, Marly A et al (2009) Use of mass spectrometry to identify clinical Fusarium isolates. Clin Microbiol Infect 15:634–642
Boer WH, van Ampting JM, Vos P (2007) Successful treatment of eight episodes of Candida peritonitis without catheter removal using intracatheter administration of amphotericin. B Perit Dial Int 27:208–210
Solomkin JS, Flohr A, Simmons RL (1982) Candida infections in surgical patients. Dose requirements and toxicity of amphotericin B. Ann Surg 195:177–185
Aperis G, Mylonakis E (2006) Newer triazole antifungal agents: pharmacology, spectrum, clinical efficacy and limitations. Expert Opin Investig Drugs 15:579–602
Aperis G, Myriounis N, Spanakis EK et al (2006) Developments in the treatment of candidiasis: more choices and new challenges. Expert Opin Investig Drugs 15:1319–1336
Pappas PG, Kauffman CA, Andes D et al (2009) Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis 48:503–535
Spanakis EK, Aperis G, Mylonakis E (2006) New agents for the treatment of fungal infections: clinical efficacy and gaps in coverage. Clin Infect Dis 43:1060–1068
Kwon DS, Mylonakis E (2007) Posaconazole: a new broad-spectrum antifungal agent. Expert Opin Pharmacother 8:1167–1178
Langner S, Staber PB, Neumeister P (2008) Posaconazole in the management of refractory invasive fungal infections. Ther Clin Risk Manag 4:747–758
Charlier C, Hart E, Lefort A et al (2006) Fluconazole for the management of invasive candidiasis: where do we stand after 15 years? J Antimicrob Chemother 57:384–410
Guinea J, Bouza E (2008) Isavuconazole: a new and promising antifungal triazole for the treatment of invasive fungal infections. Future Microbiol 3:603–615
Guinea J, Pelaez T, Recio S et al (2008) In vitro antifungal activities of isavuconazole (BAL4815), voriconazole, and fluconazole against 1,007 isolates of Zygomycete, Candida, Aspergillus, Fusarium, and Scedosporium species. Antimicrob Agents Chemother 52:1396–1400
Shan YS, Sy ED, Wang ST et al (2006) Early presumptive therapy with fluconazole for occult Candida infection after gastrointestinal surgery. World J Surg 30:119–126. doi:10.1007/s00268-005-7807-z
Bohnen JM (1998) Antibiotic therapy for abdominal infection. World J Surg 22:152–157. doi:10.1007/s002689900363
Kourkoumpetis TK, Velmahos GC, Ziakas PD et al (2011) The effect of cumulative length of hospital stay on the antifungal resistance of Candida strains isolated from critically ill surgical patients. Mycopathologia 171:85–91
O’Connell K, Lyons M, Hanahoe B et al (2011) Antifungal susceptibility testing and candidaemia at a tertiary referral hospital. Ir Med J 104:55–56
Slavin MA, Sorrell TC, Marriott D et al (2010) Candidaemia in adult cancer patients: risks for fluconazole-resistant isolates and death. J Antimicrob Chemother 65:1042–1051
Tan TY, Tan AL, Tee NW et al (2008) A retrospective analysis of antifungal susceptibilities of Candida bloodstream isolates from Singapore hospitals. Ann Acad Med Singapore 37:835–840
Solomkin JS, Mazuski JE, Bradley JS et al (2010) Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Clin Infect Dis 50:133–164
Morrell M, Fraser VJ, Kollef MH (2005) Delaying the empiric treatment of candida bloodstream infection until positive blood culture results are obtained: a potential risk factor for hospital mortality. Antimicrob Agents Chemother 49:3640–3645
Solomkin JS (2010) Evaluating evidence and grading recommendations: the SIS/IDSA guidelines for the treatment of complicated intra-abdominal infections. Surg Infect (Larchmt) 11:269–274
Fabris A, Pellanda MV, Gardin C et al (1993) Pharmacokinetics of antifungal agents. Perit Dial Int 13(Suppl 2):S380–S382
Piraino B, Bailie GR, Bernardini J et al (2005) Peritoneal dialysis-related infections recommendations: 2005 update. Perit Dial Int 25:107–131
Senn L, Eggimann P, Ksontini R et al (2009) Caspofungin for prevention of intra-abdominal candidiasis in high-risk surgical patients. Intensive Care Med 35:903–908
Playford EG, Webster AC, Sorrell TC et al (2006) Antifungal agents for preventing fungal infections in non-neutropenic critically ill and surgical patients: systematic review and meta-analysis of randomized clinical trials. J Antimicrob Chemother 57:628–638
Shorr AF, Chung K, Jackson WL et al (2005) Fluconazole prophylaxis in critically ill surgical patients: a meta-analysis. Crit Care Med 33:1928–1935; quiz 1936
Cruciani M, de Lalla F, Mengoli C (2005) Prophylaxis of Candida infections in adult trauma and surgical intensive care patients: a systematic review and meta-analysis. Intensive Care Med 31:1479–1487
Cruciani M, Mengoli C, Malena M et al (2006) Antifungal prophylaxis in liver transplant patients: a systematic review and meta-analysis. Liver Transpl 12:850–858
Leon C, Ruiz-Santana S, Saavedra P et al (2006) A bedside scoring system (“Candida score”) for early antifungal treatment in nonneutropenic critically ill patients with Candida colonization. Crit Care Med 34:730–737
van der Velden WJ, Plantinga TS, Donnelly JP et al (2010) Host-microbe interactions in stem cell transplantation: recognizing Candida in infection and inflammation. Virulence 1:180–184
Bond S, Stewart DL, Bendon RW (2000) Invasive Candida enteritis of the newborn. J Pediatr Surg 35:1496–1498
Rodrigues RJ, Wolff WI (1974) Fungal septicemia in surgical patients. Ann Surg 180:741–746
Eggimann P, Francioli P, Bille J et al (1999) Fluconazole prophylaxis prevents intra-abdominal candidiasis in high-risk surgical patients. Crit Care Med 27:1066–1072
Acknowledgments
The authors thank Dr. Nicholas Tritos for review of the manuscript.
Disclosures
EM has received research funding from Astellas Pharma, Inc. and T2 Biosystems, Inc.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Carneiro, H.A., Mavrakis, A. & Mylonakis, E. Candida Peritonitis: An Update on the Latest Research and Treatments. World J Surg 35, 2650–2659 (2011). https://doi.org/10.1007/s00268-011-1305-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-011-1305-2