Abstract
Background
Recent studies have suggested that the Model for End-Stage Liver Disease (MELD) may represent a promising alternative to the Child-Turcotte-Pugh classification as a predictive factor of operative mortality and morbidity. This study was designed to evaluate the value of MELD and four MELD-based indices (iMELD: integrated MELD; MESO: MELD to sodium ratio; MELD-Na: MELD with incorporation of sodium; MELD-XI: MELD excluding the International Normalized Ratio) in the quantification of surgical risk for patients with cirrhosis and compare its prognostic value with the Child-Turcotte-Pugh classification and two derived scores (proposed by Huo and Giannini, respectively).
Methods
A retrospective study of 190 patients with cirrhosis, operated on in our department between 1993 and 2008, was undertaken.
Results
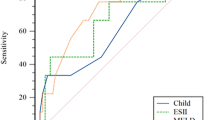
Forty-three percent of patients were included in Child-Turcotte-Pugh A class, and their mean MELD score was 12.2 ± 4.9 (range, 6.4–35.2). Mortality and morbidity rates were 13% and 24%, respectively. In global analysis of mortality, MELD-based indices presented an acceptable prognostic performance (auROC = 71–77%), similar to the three analyzed Child-Turcotte-Pugh-derived scores. iMELD demonstrated the highest prognostic capacity (auROC = 77%; 95% confidence interval (CI), 66–88; p = 0.0001); operative death probability was 4% (95% CI, 3.6–4.4) when the score was inferior to 35, 16.1% (95% CI, 14.4–17.9) between 35 and 45, and 50.1% (95% CI, 42.2–58.1) when superior to 45. In elective surgical procedures, iMELD represented a useful prognostic factor of operative mortality (auROC = 80%; 95% CI, 63–97; p = 0.044) with significant correlation and better accuracy then MELD and Child-Turcotte-Pugh-derived indices.
Conclusions
In this study, iMELD was a useful predictive parameter of operative mortality for patients with cirrhosis submitted to elective procedures. Further studies are necessary to define the relevance of MELD-based indices in the individual surgical risk evaluation.


Similar content being viewed by others
Abbreviations
- iMELD:
-
Integrated MELD
- MESO:
-
MELD to sodium ratio
- MELD-Na:
-
MELD with incorporation of sodium
- MELD-XI:
-
MELD excluding the international normalized ratio
- σ:
-
Spearman’s correlation coefficient.
References
del Olmo JA, Flor-Lorente B, Flor-Civera B et al (2003) Risk factors for nonhepatic surgery in patients with cirrhosis. World J Surg 27:647–652
Pugh RN, Murray-Lyon IM, Dawson JL et al (1973) Transection of the oesophagus for bleeding oesophageal varices. Br J Surg 60:646–649
Freeman RB (2005) MELD: the holy grail of organ allocation? J Hepatol 42:16–20
Mansour A, Watson W, Shayani V et al (1997) Abdominal operations in patients with cirrhosis: still a major surgical challenge. Surgery 122:730–736
O’Leary JG, Friedman LS (2007) Predicting surgical risk in patients with cirrhosis: from art to science. Gastroenterology 132:1609–1610
Durand F, Valla D (2005) Assessment of the prognosis of cirrhosis: Child-Pugh versus MELD. J Hepatol 42:S100–S107
Malinchoc M, Kamath PS, Gordon FD et al (2000) A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 31:864–871
Teh SH, Nagorney DM, Stevens SR et al (2007) Risk factors for mortality after surgery in patients with cirrhosis. Gastroenterology 132:1261–1269
Northup PG, Wanomaker RC, Lee VD et al (2005) Model for End-Stage Liver Disease (MELD) predicts nontransplant surgical mortality in patients with cirrhosis. Ann Surg 242:244–251
Cucchetti A, Ercolani G, Vivarelli M et al (2006) Impact of model for end-stage liver disease (MELD) score on prognosis after hepatectomy for hepatocellular carcinoma on cirrhosis. Liver Transpl 12:966–971
Befeler AS, Palmer DE, Hoffman M et al (2005) The safety of intra-abdominal surgery in patients with cirrhosis: model for end-stage liver disease is superior to Child-Turcotte-Pugh classification in predicting outcome. Arch Surg 140:650–654
Farnsworth N, Fagan SP, Berger DH et al (2004) Child-Turcotte-Pugh versus MELD score as a predictor of outcome after elective and emergent surgery in cirrhotic patients. Am J Surg 188:580–583
Perkins L, Jeffries M, Patel T (2004) Utility of preoperative scores for predicting morbidity after cholecystectomy in patients with cirrhosis. Clin Gastroenterol Hepatol 2:1123–1128
Huo TI, Lee SD, Lin HC (2008) Selecting an optimal prognostic system for liver cirrhosis: the model for end-stage liver disease and beyond. Liver Int 28:606–613
Kamath PS, Kim WR, Advanced liver disease study group (2007) The model for end-stage liver disease (MELD). Hepatology 45:797–805
Durand F, Valla D (2008) Assessment of prognosis of cirrhosis. Semin Liver Dis 28:110–122
Cholongitas E, Papatheodoridis GV, Vangeli M et al (2005) Systematic review: the model for end-stage liver disease–should it replace Child-Pugh’s classification for assessing prognosis in cirrhosis? Aliment Pharmacol Ther 22:1079–1089
Luca A, Angermayr B, Bertolini G et al (2007) An integrated MELD model including serum sodium and age improves the prediction of early mortality in patients with cirrhosis. Liver Transp 13:1174–1180
Biggins SW, Kim WR, Terrault NA et al (2006) Evidence-based incorporation of serum sodium concentration into MELD. Gastroenterology 130:1652–1660
Huo TI, Wang YW, Yang YY et al (2007) Model for end-stage liver disease score to serum sodium ratio index as a prognostic predictor and its correlation with portal pressure in patients with liver cirrhosis. Liver Int 27:498–506
Huo T, Lin H, Huo SC et al (2008) Comparison of four model for end-stage liver disease-based prognostic systems for cirrhosis. Liver Transpl 14:837–844
Heuman DM, Habib A, Abou-Assi S et al (2005) Rationally derived Child-Turcotte-Pugh (CTP) subclasses permit accurate stratification of near-term risk in cirrhotic patients referred for liver transplantation. Gastroenterology 128:A-734
Huo TI, Lin HC, Wu JC et al (2006) Proposal of a modified Child-Turcotte-Pugh scoring system and comparison with the model for end-stage liver disease for outcome prediction in patients with cirrhosis. Liver Transpl 12:65–71
Giannini E, Botta F, Fumagalli A et al (2004) Can inclusion of serum creatinine values improve the Child-Turcotte-Pugh score and challenge the prognostic yield of the model for end-stage liver disease score in the short-term prognostic assessment of cirrhotic patients? Liver Int 24:465–470
Papatheodoridis GV, Cholongitas E, Dimitriadou E et al (2005) MELD vs. Child-Pugh and creatinine-modified Child-Pugh score for predicting survival in patients with decompensated cirrhosis. World J Gastroenterol 11:3099–3104
Angermayer B, Koening F, Cejna M et al (2002) Creatinine-modified Child-Pugh score (CPSC) compared with MELD-score to predict survival in patients undergoing TIPS. Hepatology 36:860A
Ferenci P, Lockwood A, Mullen K et al (2002) Hepatic encephalopathy: definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th world congress of gastroenterology, Vienna, 1998. Hepatology 35:716–721
ASA physical status classification system. American Society of Anesthesiologists website. http://www.asahq.org/clinical/physical status.htm.2008. Accessed 28 Feb 2008
Lorimer JW, Doumit G (2007) Comorbidity is a major determinant of severity in acute diverticulitis. Am J Surg 193:681–685
Charlson ME, Szatrowski TP, Peterson J et al (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251
Sutton R, Bann S, Brooks M et al (2002) The surgical risk scale as an improved tool for risk-adjusted analysis in comparative surgical audit. Br J Surg 89:763–768
Neary WD, Prytherch D, Foy C et al (2007) Comparison of different methods of risk stratification in urgent and emergency surgery. Br J Surg 94:1300–1305
Heuman DM, Mihas AA, Habib A et al (2007) MELD-XI: a rational approach to “sickest first” liver transplantation in cirrhotic patients requiring anticoagulant therapy. Liver Transpl 13:30–37
Teh SH, Sheppard BC, Schwartz J et al (2008) Model for end-stage liver disease score fails to predict perioperative outcome after hepatic resection for hepatocellular carcinoma in patients without cirrhosis. Am J Surg 195:697–701
Durand F (2006) Risk scores in cirrhotic patients: from non-transplant surgery to transplantation and back. J Hepatol 44:620–621
Hoteit MA, Ghazale AH, Bain AJ et al (2008) Model for end-stage liver disease score versus child score in predicting the outcome of surgical procedures in patients with cirrhosis. World J Gastrenterol 14:1774–1780
Schroeder RA, Marroquin CE, Bute BP et al (2006) Predictive indices of morbidity and mortality after liver resection. Ann Surg 243:373–379
Bingener J, Cox D, Michalek J et al (2008) Can the MELD score predict perioperative morbidity for patients with liver cirrhosis undergoing laparoscopic cholecystectomy? Am Surg 74:156–159
Filsoufi F, Salzberg SP, Rahmanian PB et al (2007) Early and late outcome of cardiac surgery in patients with liver cirrhosis. Liver Transp 13:990–995
Londoño M, Cárdenas A, Guevara M et al (2007) MELD score and serum sodium in the prediction of survival of patients with cirrhosis awaiting liver transplantation. Gut 56:1283–1290
Lisman T, van Leeuwen Y, Adelmeijer J et al (2008) Interlaboratory variability in assessment of the model of end-stage liver disease score. Liver Int 28:1344–1351
Huo TI, Wu JC, Lin HC et al (2005) Evaluation of the increase in model for end-stage liver disease (MELD) score overtime as a prognostic predictor in patients with advanced cirrhosis: risk factor analysis and comparison with initial MELD and Child-Turcotte-Pugh score. J Hepatol 42:826–832
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Costa, B.P., Castro Sousa, F., Serôdio, M. et al. Value of MELD and MELD-Based Indices in Surgical Risk Evaluation of Cirrhotic Patients: Retrospective Analysis of 190 Cases. World J Surg 33, 1711–1719 (2009). https://doi.org/10.1007/s00268-009-0093-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-0093-4