Abstract
Background
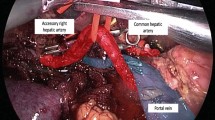
Sometimes, it seems to be difficult to preserve the aberrant hepatic artery (HA) during pancreaticoduodenectomy (PD), with respect to en bloc lymph node dissection, especially in the case of aberrant right hepatic artery (RHA). Therefore, we evaluated the influence of incomplete en bloc lymph node (LN) dissection when aberrant RHA arises.
Methods
We reviewed 103 patients with mid-to-distal common bile duct (CBD) cancers who underwent PD by one surgeon at Asan Medical Center from December 1994 to November 2005 (73 men, 30 women; mean age, 61.1 ± 9.4 (range: 40–84) years). The mean follow-up period was 32.7 months. We compared the normal RHA group with the aberrant RHA group.
Results
Eighty-eight cases showed normal RHA anatomy, including nine cases (8.7%) of aberrant left hepatic artery (LHA) with normal RHA cases (normal HA group). RHA anomalies were observed in 15 cases (14.6%, aberrant HA group). In all cases, there was no direct invasion of cancer to aberrant HA. Among two groups, 43 cases (41.7%) showed recurrence and there was no significant difference in recurrence between two groups (p = 0.202). Three-year and 5-year overall survivals were 33.3% and 28.5% in the normal HA group, whereas 47.1% and 28.3% in the aberrant RHA group, respectively. There also was no statistically significant difference in survival (p = 0.763).
Conclusions
When performing PD for CBD cancer, aberrant RHA should be preserved if there was no cancerous invasion and it does not seem to affect the recurrence of disease and overall survival of patients.



Similar content being viewed by others
References
Yang SH, Yin YH, Jang JY et al (2000) Assessment of hepatic arterial anatomy in keeping with preservation of the vasculature while performing pancreatoduodenectomy: an opinion. World J Surg 31:2384–2391
Koops A, Wojciechowski B, Broering DC et al (2004) Anatomic variations of the hepatic arteries in 604 selective celiac and superior mesenteric angiographies. Surg Radiol Anat 26:239–244
Michels NA (1996) Newer anatomy of the liver and its variant blood supply and collateral circulation. Am J Surg 112:337–347
Hiatt JR, Gabby J, Busuttil RW (1994) Surgical anatomy of the hepatic arteries in 1000 cases [review]. Ann Surg 200:50–52
Kennedy EP, Yeo CJ (2007) Pancreaticoduodenectomy with extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma. Surg Oncol Clin N Am 16:157–176
Seyama Y, Makuuchi M (2007) Current surgical treatment for bile duct cancer. World J Gastroenterol 13:1505–1515
López-Andújar R, Moya A, Montalvá E et al (2007) Lessons learned from anatomic variants of the hepatic artery in 1,081 transplanted livers. Liver Tranpl 13:1401–1404
Yang F, Long J, Fu DL et al (2008) Aberrant hepatic artery in patients undergoing pancreaticoduodenectomy. Pancreatology 8:50–54
Suzuki T, Nakayasu A (1971) Surgical significance of anatomic variations of the hepatic artery. Am J Surg 122:505–512
Volpe CM, Peterson S, Hoover EL et al (1998) Justification for visceral angiography prior to pancreaticoduodenectomy. Am Surg 64:758–761
Woods MS, Traverso LW (1993) Sparing a replaced common hepatic artery during pancreaticoduodenectomy. Am Surg 59:719–721
Traverso LW, Freeny PC (1989) Pancreaticoduodenectomy, the importance of preserving hepatic blood flow to prevent biliary fistula. Am Surg 55:421–426
Yamamoto S, Kubota K, Rokkaku K et al (2005) Disposal of replaced common hepatic artery coursing within the pancreas during pancreatoduodenectomy: report of a case. Surg Today 35:984–987
Michels NA (1955) Blood supply and anatomy of the upper abdominal organs with a descriptive atlas. Lippincott, Philadelphia, pp 139–182
Yeo CJ, Cameron JL, Sohn TA et al (1999) Pancreaticoduodenectomy with or without extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma. Ann Surg 229:613–624
Noie T, Harihara Y, Inoue K et al (2001) Ventral dissection of replaced right hepatic artery during pancreatoduodenectomy. Hepatogastroenterology 48:999–1000
Lee MW, Lee JM, Lee JY et al (2006) Preoperative evaluation of hepatic vascular anatomy in living liver donors: comparison of CT angiography and MR angiography. J Magn Reson Imaging 24:1081–1087
Rong GH, Sindelar WF (1987) Aberrant peripancreatic arterial anatomy. Considerations in performing pancreatectomy for malignant neoplasms. Am Surg 53:726–729
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, JM., Lee, YJ., Kim, CW. et al. Clinical Implications of an Aberrant Right Hepatic Artery in Patients Undergoing Pancreaticoduodenectomy. World J Surg 33, 1727–1732 (2009). https://doi.org/10.1007/s00268-009-0063-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-0063-x