Abstract
Background
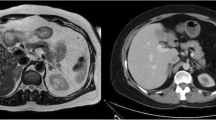
In patients with primary hyperaldosteronism, solitary adrenal adenomas are an indication for surgical intervention. In contrast, adrenal hyperplasia is almost exclusively treated by drugs.
Patients and methods
In a prospective clinical study 183 patients (81 men, 102 women; age 49.6 ± 12.8 years) with Conn’s syndrome were operated on using the posterior retroperitoneoscopic approach. Tumor size ranged from 0.2 to 5.0 cm (mean 1.5 ± 0.8 cm). Final histology described a solitary adenoma in 127 patients and adrenal hyperplasia in 56 patients. Partial adrenalectomies were performed in 47 operations.
Results
The perioperative complication rate was 4%, mortality zero. In none of the cases was conversion to open surgery necessary. The mean operating time was 58 ± 32 minutes (range 20–230 minutes) and was associated with sex (p < 0.001) but not with the extent of resection (partial vs. total, p = 0.51) or with tumor size (≤1.5 vs. >1.5 cm; p = 0.43) or tumor site (p = 0.77). Median blood loss was 15 ml. Median duration of postoperative hospitalization was 4 days. After a mean follow-up of nearly 5 years, 96% of patients are normokalemic, 30% of patients are cured (normotensive without medication), and 87% showed an improvement of hypertension (normotensive without or with reduced medication). Cure of hypertension depended on the patient’s age (p < 0.001) and sex (p < 0.001), duration of hypertension (p < 0.05), and histomorphology (p < 0.001). Improvement of hypertension was not associated with any of these factors.
Conclusions
Retroperitoneoscopic removal of adrenal glands in patients with Conn’s syndrome is a safe, rapidly performed surgical procedure and can thus be considered as first choice option for treatment of both solitary adrenal adenomas and hyperplasia presenting with a clinically predominating nodule.


Similar content being viewed by others
References
Young WF (2007) Primary aldosteronism: renaissance of a syndrome. Clin Endocrinol (Oxf) 66:607–618
Unger N, Lopez Schmidt I, Pitt C et al (2004) Comparison of active renin concentration and plasma renin activity for the diagnosis of primary hyperaldosteronism in patients with an adrenal mass. Eur J Endocrinol 150:517–523
Walz MK, Peitgen K, Hoermann R et al (1996) Posterior retroperitoneoscopy as a new minimally invasive approach for adrenalectomy: results of 30 adrenalectomies in 27 patients. World J Surg 20:769–774
Walz MK, Peitgen K, Walz MV et al (2001) Posterior retroperitoneoscopic adrenalectomy: lessons learned within five years. World J Surg 25:728–734
Walz MK, Alesina PF, Wenger FA et al (2006) Posterior retroperitoneoscopic adrenalectomy—results of 560 procedures in 520 patients. Surgery 140:943–948; discussion 948–950
Walz MK, Peitgen K, Saller B et al (1998) Subtotal adrenalectomy by the posterior retroperitoneoscopic approach. World J Surg 22:621–626
Walz MK, Peitgen K, Diesing D et al (2004) Partial versus total adrenalectomy by the posterior retroperitoneoscopic approach: early and long-term results of 325 consecutive procedures in primary adrenal neoplasias. World J Surg 28:1323–1329
Bonjer HJ, Sorm V, Berends FJ et al (2000) Endoscopic retroperitoneal adrenalectomy: lessons learned from 111 consecutive cases. Ann Surg 232:796–803
Sasagawa I, Suzuki Y, Itoh K et al (2003) Posterior retroperitoneoscopic partial adrenalectomy: clinical experience in 47 procedures. Eur Urol 43:381–385
Zhang X, He H, Chen Z et al (2004) [Retroperitoneal laparoscopic management of primary aldosteronism with report of 130 cases]. Zhonghua Wai Ke Za Zhi 42:1093–1095
Gagner M, Pomp A, Heniford BT et al (1997) Laparoscopic adrenalectomy: lessons learned from 100 consecutive procedures. Ann Surg 226:238–246
Henry JF, Sebag F, Iacobone M et al (2002) [Lessons learned from 274 laparoscopic adrenalectomies]. Ann Chir 127:512–519
Fernandez-Cruz L, Saenz A, Benarroch G et al (1996) Laparoscopic unilateral and bilateral adrenalectomy for Cushing’s syndrome: transperitoneal and retroperitoneal approaches. Ann Surg 224:727–734; discussion 734–726
Rossi H, Kim A, Prinz RA (2002) Primary hyperaldosteronism in the era of laparoscopic adrenalectomy. Am Surg 68:253–256; discussion 256–257
Meria P, Kempf BF, Hermieu JF et al (2003) Laparoscopic management of primary hyperaldosteronism: clinical experience with 212 cases. J Urol 169:32–35
Goh BK, Tan YH, Yip SK et al (2004) Outcome of patients undergoing laparoscopic adrenalectomy for primary hyperaldosteronism. JSLS 8:320–325
Zhang X, Fu B, Lang B et al (2007) Technique of anatomical retroperitoneoscopic adrenalectomy with report of 800 cases. J Urol 177:1254–1257
Giebler RM, Walz MK, Peitgen K et al (1996) Hemodynamic changes after retroperitoneal CO2 insufflation for posterior retroperitoneoscopic adrenalectomy. Anesth Analg 82:827–831
Imai T, Tanaka Y, Kikumori T et al (1999) Laparoscopic partial adrenalectomy. Surg Endosc 13:343–345
Kok KY, Yapp SK (2002) Laparoscopic adrenal-sparing surgery for primary hyperaldosteronism due to aldosterone-producing adenoma. Surg Endosc 16:108–111
Ikeda Y, Takami H, Sasaki Y et al (2003) Is laparoscopic partial or cortical-sparing adrenalectomy worthwile? Eur Surg 35:89–92
Jeschke K, Janetschek G, Peschel R et al (2003) Laparoscopic partial adrenalectomy in patients with aldosterone-producing adenomas: indications, technique, and results. Urology 61:69–72
Ishidoya S, Ito A, Sakai K et al (2005) Laparoscopic partial versus total adrenalectomy for aldosterone producing adenoma. J Urol 174:40–43
Shen WT, Lim RC, Siperstein AE et al (1999) Laparoscopic vs open adrenalectomy for the treatment of primary hyperaldosteronism. Arch Surg 134:628–631; discussion 631–622
Brunt LM, Moley JF, Doherty GM et al (2001) Outcomes analysis in patients undergoing laparoscopic adrenalectomy for hormonally active adrenal tumors. Surgery 130:629–635
Nwariaku FE, Miller BS, Auchus R et al (2006) Primary hyperaldosteronism: effect of adrenal vein sampling on surgical outcome. Arch Surg 141:497–502; discussion 502–493
Favia G, Lumachi F, Scarpa V et al (1992) Adrenalectomy in primary aldosteronism: a long-term follow-up study in 52 patients. World J Surg 16:680–683
Sawka AM, Young WF, Thompson GB et al (2001) Primary aldosteronism: factors associated with normalization of blood pressure after surgery. Ann Intern Med 135:258–261
Stowasser M, Klemm SA, Tunny TJ et al (1994) Response to unilateral adrenalectomy for aldosterone-producing adenoma: effect of potassium levels and angiotensin responsiveness. Clin Exp Pharmacol Physiol 21:319–322
Proye CA, Mulliez EA, Carnaille BM et al (1998) Essential hypertension: first reason for persistent hypertension after unilateral adrenalectomy for primary aldosteronism? Surgery 124:1128–1133
Gockel I, Heintz A, Polta M et al (2007) Long-term results of endoscopic adrenalectomy for Conn’s syndrome. Am Surg 73:174–180
Lo CY, Tam PC, Kung AW et al (1996) Primary aldosteronism: results of surgical treatment. Ann Surg 224:125–130
Celen O, O’Brien MJ, Melby JC et al (1996) Factors influencing outcome of surgery for primary aldosteronism. Arch Surg 131:646–650
Obara T, Ito Y, Okamoto T et al (1992) Risk factors associated with postoperative persistent hypertension in patients with primary aldosteronism. Surgery 112:987–993
Goh BK, Tan YH, Chang KT et al (2007) Primary hyperaldosteronism secondary to unilateral adrenal hyperplasia: an unusual cause of surgically correctable hypertension: a review of 30 cases. World J Surg 31:72–79
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walz, M.K., Gwosdz, R., Levin, S.L. et al. Retroperitoneoscopic Adrenalectomy in Conn’s Syndrome Caused by Adrenal Adenomas or Nodular Hyperplasia. World J Surg 32, 847–853 (2008). https://doi.org/10.1007/s00268-008-9513-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9513-0