Abstract
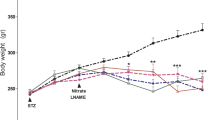
Streptozotocin administration in newborn rats (nSTZ-rats) leads to adults with mild insulin deficiency and normoglycemia, and is accepted as a model of type 2 diabetes. We examined possible differences in the production of inflammatory mediators between healthy and nSTZ-rats after ischemia-reperfusion (I-R). Two-month-old control and nSTZ-rats were randomly separated into control and intestinal I-R groups. After reperfusion, samples were obtained from the portal vein (PV) infrahepatic cava vein (ICV), suprahepatic cava vein (SCV), jejunal wall, and pancreas. Nitric oxide (NO), lipid hydroperoxides (LPO), tumor necrosis factor alpha (TNF-α), 60 kDa receptor (sTNF-R1), 80 kDa (sTNF-R2), and intercellular adhesion molecule-1 (ICAM-1), were determined. After I-R, nSTZ-rats showed increased plasma concentrations of LPO, NO, ICAM-1 (0.5141 ± 0.083 vs 0.024 ± 0.003, ICV; 0.574 ± 0.075 vs 0.023 ± 0.003, SCV; 0.528 ± 0.067 vs 0.027 ± 0.003 PV; ng/ml), TNF-α (42.4 ± 5.7 ICV, 248.4 ± 28.2 SCV, and 33.6 ± 4.0 PV. In n STZ-rats, vs 4.36 ± 0.57, 4.74 ± 0.77, and 3.16 ± 0.32, respectively, in control rats; pg/ml), and sTNF-R1. Both TNF-α and NO plasma levels were higher in SCV than in ICV and PV after I-R. In addition, after I-R, jejunal wall of nSTZ-rats showed an increase of TNF-α IL-1, and IL-10 levels. A pre-existing state of glucose intolerance intensifies the inflammatory response after intestinal I-R.






Similar content being viewed by others
References
Santini SA, Marra G, Giardino B, et al. Defective plasma antioxidant defenses and enhanced susceptibility to lipid peroxidation in uncomplicated IDDM. Diabetes 1997; 46:1853–1858
Panes J, Kurose I, Rodriguez-Vaca MD, et al. Diabetes exacerbates inflammatory responses to ischemia-reperfusion. Circulation 1996; 93:161–167
Welbourn CRB, Young Y. Endotoxin, septic shock and acute lung injury: neutrophils, macrophages and inflammatory mediators. Br J Surg 1992;79:998–1003
Jennings PE, Scott NA, Saniabadi AR, et al. Effects of gliclazide on platelet reactivity and free radicals in type II diabetic patients. Clinical assessment. Metabolism 1992 ;41:36–39
Aragno M, Parola S, Brignardello E, et al. Dehydroepiandrosterone prevents oxidative injury induced by transient ischemia/reperfusion in the brain of diabetic rats. Diabetes 2000; 49:1924–1931
Lawson S, Ward DT, Conner C, et al. Diabetic hyperglycemia: a facilitating factor in systemic capillary leak. J Surg Res 2002; 105:95–101
Giroix MH, Sener A, Bailbe D, et al. Impairment of the mitochondrial oxidative response to D-glucose in pancreatic islets from adult rats injected with streptozotocin during the neonatal period. Diabetologia 1990; 33:654–660
Portha B. Decreased glucose-induced insulin release and biosynthesis by islets of rats with non-insulin-dependent diabetes: effect of tissue culture. Endocrinology 1985; 117:1735–1741
Megison SM, Horton JW, Chao H, et al. A new model for intestinal ischemia in the rat. J Surg Res. 1990; 49:168–173
Holley AE, Cheesseman KH. Measuring free radical reactions in vivo. Br. Med. Bull. 1993; 49:494–505
Tatsishi T, Yoshimine N, Kuzuya F. Serum lipid peroxide assayed by a new colorimetric method. Exp. Gerontol. 1987;22:103–111
Arias-Diaz J, Vara E, Garcia C, et al. Evidence for a cyclic guanosine monophosphate–dependent, carbon monoxide-mediated, signaling system in the regulation of TNF-alpha production by human pulmonary macrophages. Arch Surg 1995; 130: 1287–1293
Portha B, Levacher C, Picon L, et al. Diabetogenic effect of streptozotocin in the rat during the perinatal period. Diabetes 1974; 23:880–895
Burcellin R, Eddouks M, Maury J, et al. Excessive glucose production, rather than insulin resistance, accounts for hyperglycemia in recent-onset-streptozotocin-diabetic rats. Diabetologia 1995;38:283–290
Edrees WK, Young IS, Lau LL, et al. Accentuated oxidative stress following reperfusion injury in diabetic rats. Int Angiol 2002; 21:58–62
Salas A, Panes J, Rosenbloom CL, et al. Differential effects of a nitric oxide donor on reperfusion-induced microvascular dysfunction in diabetic and non-diabetic rats. Diabetologia 1992; 42:1350–1358
Desfaits AC, Serrio D, Renier G. Normalization of plasma lipid peroxides, monocyte adhesion, and tumor necrosis factor-α production in NIDDM patients after gliclazide treatment. Diabetes Care 1998;21:487–493 http://care diabetes journals org/content/ro z1/issue 4/index.shtml
Nguyen P, Durlach V, Leutenegger M, et al. Explosion respiratoire des polynucléaris neutrophiles et profil des cytokines chez le diabétique non insulin-dépendant. J. Mal. Vasc. 1995; 20:102–105
Cavallo MG, Pozzili P, Bird C, et al. Cytokines in sera from insulin-dependent diabetic patients at diagnosis. Clin. Exp. Immunol. 1991; 86:256–259
Hotamisligil GS. The role of TNF-alpha and TNF receptors in obesity and insulin resistance. J. Intern. Med.1999; 245:621–625
Uysal KT, Wiesbrock SM, Hotamisligil GS. Functional analysis of tumor necrosis factor (TNF) receptors in TNF-α-mediated insulin resistance in genetic obesity. Endocrinology 1998; 139:4832–4838
Slotwinski R, Olszewski WL, Chaber A, et al. The soluble tumor necrosis factor receptor I is an early predictor of local infective complications after colorectal surgery. J. Clin. Immunol. 2002; 22:289–296
Vaisman N, Schattner A, Hahn T. Tumor necrosis factor production during starvation. Am. J. Med. 1989;87:115
Patel RT, Deen KI, Youngs DJ, et al. Interleukin-6 is a prognostic indicator of outcome in severe intra-abdominal sepsis. Br. J. Surg. 1994; 81:1306–1308
Damas P, Canivet JL, DeGrootte D, et al. Sepsis and serum cytokine concentrations. Crit. Care Med. 1997; 25:405–412
Katja B, Hartmut K, Pawel M, et al. The value of immune modulating parameters in predicting the progression from peritonitis to septic shock. Shock 2001;15:95–100
Presterl E, Staudinger T, Pettermann M, et al. Cytokine profile and correlation to the APACHE III and MPM II scores in patients with sepsis. Am. J. Respir. Crit. Care Med. 1997;156:825–832
Rapoport MJ, Mor A, Vardi P, et al. Decreased secretion of Th2 cytokines precedes up-regulated and delayed secretion of Th1 cytokines in activated peripheral blood mononuclear cells from patients with insulin-dependent diabetes mellitus. J. Autoimmun. 1998; 11:635–642
Vara E, Arias-Díaz J, Garcia C, et al. Production of TNF-alpha, IL-1, IL-6 and nitric oxide by isolated human islets. Transplant. Proc. 1995; 26:3367–3371
Yamada K, Takane N, Otabe S, et al. Pancreatic β-cell-selective production of tumor necrosis factor α induced by interleukin–1. Diabetes 1993;42:1026–1031
Campbell IL, Cutri A, Wilson A, et al. Evidence for IL-6 production by and effects on the pancreatic beta cell. J. Immunol. 1989;143:1188–1191
Rothlein R, Mainolgi EA, Czajkowski M. A form of circulating ICAM-1 in human serum. J. Immunol. 1991 147:3788–3793
Lo SK, Janakidevi K, Malik AB. Hydrogen peroxide-induced increase in endothelial adhesiveness is dependent on ICAM-1 activation. Am. J. Physiol. 1993;264:L406–L412
Sato Y, Hotta N, Sakamoto N et al. Lipid peroxide level in plasma of diabetic patients. Biochem. Med. 1979; 21:104–107
Ding AH, Nathan CF, Stuehr DJ. Release of reactive nitrogen and reactive intermediates from mouse peritoneal macrophages. Comparison of activating cytokines and evidence for independent production. J. Immunol. 1988; 141:2407–2412
Parks DA, Granger DN. Contributions of ischemia and reperfusion to mucosal lesion formation. Am. J. Physiol. 1986; 250:G749–753
Schoenberg MH, Fredholm BB, Haglund U. Studies on the oxygen radical mechanism involved in the small intestinal reperfusion damage. Acta Physiol. Scand. 1985; 124:581–589
Grisham MB, Hernandez LA, Granger DN. Xanthine oxidase and neutrophil infiltration in intestinal ischemia. Am. J. Physiol. 1986;251: G567–574
Kelly LW, Barden CA, Tiedeman JS, et al. Alterations in viscosity and filterability of whole blood and blood cell subpopulation in diabetic cats. Exp. Eye Res. 1993; 56:341–347
Freedman SF, Hatchell DL. Enhanced superoxide radical production by stimulated polymorphonuclear leukocytes in a cat model of diabetes. Exp. Eye Res. 1992; 55:767–773
Wierusz-Wysocka B, Wysochi H, Siekierba H, et al. Evidence of polymorphonuclear neutrophils (PMN) activation in patients with insulin-dependent diabetes mellitus. J. Leukocyte Biol. 1997; 42:519–523
Marzi I, Zhong Z, Zimmermann FA, et al. Xanthine and hypoxanthine accumulation during storage injury may contribute to reperfusion injury following liver transplantation in the rat. Transplant Proc. 1989; 21:1319–1320
Giugliano D, Ceriello A, Paolisso G. Oxidative stress and diabetic vascular complications. Diabetes Care 1996; 19:257–267
Huk I, Nanobash J, Neumayer CH, et al. Bioflavonoid quercetin scavenges superoxide and increases nitric oxide concentration in ischemia-reperfusion injury: an experimental study. Br. J. Surg. 1998; 85:1080–1085
Yu L, Genaro PE, Niederberger M, et al. Nitric oxide: a mediator in the rat tubular hypoxia/reoxygenation injury. Proc. Natl. Acad. Sci. USA 1994;91:1691–1695
Billiar TR, Curran RD, Stuehr DJ, et al. An L-arginine–dependent mechanism mediates Kupffer cell inhibition of hepatocyte protein synthesis in vitro. J. Exp. Med. 1989;169:1467–1472
Curran RD, Billiar TR, Stuehr DJ, et al. Hepatocytes produce nitrogen oxides from L-arginine in response to inflammatory products of Kupffer cells. J. Exp. Med. 1989;170:1769–1774
Goor Y, Peer G, Laina A, et al. Nitric oxide in ischaemic acute renal failure of streptozotocin diabetic rats. Diabetologia 1996;39:1036–1040. medscape.com
Conjer J, Robinette J, Villar A, et al. Increased nitric oxide synthase activity despite lack of response to endothelium-dependent vasodilators in postischemic acute renal failure in rats. J. Clin. Invest. 1995; 96:631–638
Schaeffer G, Wascher TC, Kostner GM, et al. Alterations in platelet Ca2+ signaling in diabetic patients are due to increased formation of superoxide anions and reduced nitric oxide production. Diabetologia 1999;42:167–176
Shi Y, Pan F, Li H, et al. Carbon monoxide concentrations in pediatric sepsis syndrome. Arch. Dis. Child. 2003; 88:889–890
Zegdi R, Perrin D, Burdin M, et al. Increased endogenous carbon monoxide production in severe sepsis. Intensive Care Med. 2002;28:793–796
Takano T, Honma K, Maeda H. Endogenous carbon monoxide production in alloxanized rats. Bull. Tokyo Med. Dent. Univ. 1997;24:1–6
Wolff DG, Bidlack WR. The formation of carbon monoxide during peroxidation of microsomal lipids. Biochem. Biophys. Res. Commun. 1976;73:850–857
Paredi P, Biernacki W, Invernizzi G, et al. Exhaled carbon monoxide levels elevated in diabetes and correlated with glucose concentration in blood; a new test for monitoring the disease? Chest 1999; 116:1007–1011
Ragnar H, Alm P, Ekström P, et al. Heme oxygenase and carbon monoxide: regulatory roles in islet hormone release. Diabetes 1999; 48:66–76
Lautier D, Luscher P, Tyrrell RM. Endogenous glutathione levels modulate both constitutive and UVA radiation/hydrogen peroxide inducible expression of the human heme-oxygenase gene. Carcinogenesis 1992; 13:227–232
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Garcia-Perez, J.C., Arias-Diaz, J., Vara, E. et al. Glucose Intolerance Modifies the Inflammatory Response After Intestinal Ischemia-Reperfusion. World J. Surg. 29, 1143–1150 (2005). https://doi.org/10.1007/s00268-005-7700-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-7700-9