Abstract
Background
The COVID-19 pandemic has upended graduate medical education globally. We investigated the COVID-19 impact on learning inputs and expected learning outputs of plastic surgery residents across the world.
Methods
We administered an online survey capturing training inputs before and during the pandemic and retrieved residents’ expected learning outputs compared with residents who completed their training before COVID. The questionnaire reached residents across the world through the mobilization of national and international societies of plastic surgeons.
Results
The analysis included 412 plastic surgery residents from 47 countries. The results revealed a 44% decline (ranging from − 79 to 10% across countries) and an 18% decline (ranging from − 76 to across 151% countries) in surgeries and seminars, respectively, per week. Moreover, 74% (ranging from 0 to 100% across countries) and 43% (ranging from 0 to 100% across countries) of residents expected a negative COVID-19 impact on their surgical skill and scientific knowledge, respectively. We found strong correlations only between corresponding input and output: surgeries scrubbed in with surgical skill (ρ = −0.511 with p < 0.001) and seminars attended with scientific knowledge (ρ = − 0.274 with p = 0.006).
Conclusions
Our ranking of countries based on their COVID-19 impacts provides benchmarks for national strategies of learning recovery. Remedial measures that target surgical skill may be more needed than those targeting scientific knowledge. Our finding of limited substitutability of inputs in training suggests that it may be challenging to make up for lost operating room time with more seminars. Our results support the need for flexible training models and competency-based advancement.
Level of evidence V
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors http://www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The spread of the novel coronavirus forced healthcare systems globally to optimize resource allocation and re-deploy healthcare personnel to save lives [1, 2]. As a result, the increased needs of patient care eclipsed other hospital priorities and often impeded medical doctors’ training [3]. Early studies explored the impact of the COVID-19 pandemic on residents’ training [4,5,6,7]. Residents’ education in surgical specialties in particular is found to be more severely impacted by the pandemic [8,9,10,11,12,13,14,15,16,17]. Recent studies have revealed substantial learning losses among plastic surgery residents in specific regions [18,19,20,21,22]. In this study, we investigate the impact of the COVID-19 pandemic on learning outcomes of plastic surgery residents at the country and continent level worldwide.
Our cross-sectional survey study goes beyond previous research in four important ways. First, we target plastic surgery residents across the world, while previous studies have explored the impact of COVID-19 at a national or a regional level. Our analysis makes comparisons between countries and provides benchmarks for national strategies of learning recovery. Second, we investigate the impact of the pandemic directly on expected learning outcomes, overcoming the challenge of identifying the intermediate relation between learning inputs, such as surgeries and seminars, and outputs, such as surgical competence. Third, the data collection for our study began two years after the pandemic had started, giving us the opportunity to capture a rather complete picture of the impact of COVID-19 on plastic surgery residents across the world. According the CDC, prior pandemics lasted 1–2 years on average [23]. Fourth, our analysis provides two contextual benchmarks of pandemic-related impact: each country’s COVID-19 disease burden and its income level. These benchmarks allow us to investigate how the pandemic severity and resource availability may contribute to the magnitude of resident learning losses during COVID-19.
Methodology
We combined data from multiple sources. First, we collected survey responses from plastic surgery residents across the world regarding their learning inputs and outputs prior to and during the COVID-19 pandemic. Second, we obtained data on each country’s COVID-19 cases and COVID-19-related deaths per million through 2021 from the Institute for Health Metrics and Evaluation (IHME) [24]. The severity of the COVID-19 pandemic in each country, measured by COVID-19 cases and deaths, may be associated with the operational pressure on local healthcare systems and any interruptions in resident training. Third, we retrieved each country’s classification in economic development from the World Bank [25]. The financial context in each country is likely to influence the operational resilience of healthcare systems and consequently the level of disruption in resident training during COVID-19.
Survey Data
We developed a survey to capture demographics, reported changes in surgeries and seminars attended prior to and during the COVID-19 pandemic, and expected impact on surgical skill and scientific knowledge at the end of the training program due to the pandemic of plastic surgery residents across the world. The survey was administered automatically through an online link in English between January 10th and February 6th, 2022.
We followed Aucejo et al. in directly asking individuals for their expected learning outcomes with and without COVID-19 [26]. The responses allowed us to directly calculate the resident-level subjective treatment effect. Our approach builds on an established literature that uses subjective expectations on education outcomes to understand decision making under uncertainty [27,28,29]. The validity of our methodology relies on the assumption that residents have well-formed expectations regarding their learning outcomes in both in a reality with the COVID-19 pandemic and in a version of reality without the pandemic. This study was approved by the Institutional Review Board at Stanford University and followed the STROBE reporting guidelines [30].
We identify key learning inputs for plastic surgery residents: surgeries participated/scrubbed in and seminars attended. Residents were asked to report the number of surgeries and seminars per week or month before and during the COVID-19 pandemic. For each learning input, we calculated the percentage change in the number of surgeries and seminars attended per week, respectively, between prior to and during the pandemic. This information allowed us to understand the severity of the pandemic-related disruption in training inputs across the world. We focused on two main learning outcomes: surgical skill and scientific knowledge. We explicitly asked residents whether the impact of the pandemic on their surgical skill and scientific knowledge has been significantly negative, slightly negative, zero, slightly positive, or significantly positive relative to residents who completed their training prior to the COVID-19 pandemic. For each leaning outcome, we created binary variable that takes the value one when the respondent replied slightly or significantly less/negative impact.
With the help of the International Society for Aesthetic Plastic Surgery (ISAPS) we reached plastic surgery residents around the world. ISAPS is the leading professional body for board-certified plastic surgeons with a network of residents in more than 100 countries. The survey link was disseminated by 63 associations of plastic surgeons, including ISAPS, to their resident members via email and social media. The survey questions and the dissemination strategy are reported in Supplementary Appendix. All residents in plastic surgery programs in training when the pandemic started in early 2020 were eligible to participate in the survey. From administrative sources, we inferred that ISAPS had 1314 plastic surgery members in 2022. If half of them were in training during the pandemic, the maximum potential sample we could have would be around 657 residents.
Results
Demographics
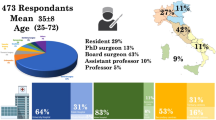
A total of 664 plastic surgery residents responded to the survey request. Two hundred and fifteen residents did not complete the survey.Footnote 1 Eleven responses were excluded from respondents who were not in training during the pandemic. Six duplicate responses were dropped. Twenty countries with single responses were excluded. The analytic sample included 412 respondents from 47 countries. Table 1 presents summary statistics of characteristics of participants and their training settings.
Females represent 42% of respondents. The majority (61%) of participants are non-Hispanic white. Sixty-three percent have prior general surgery experience of up to 2 years, while 42% of residents have had plastic surgery training prior to their residency. Our sampled residents are roughly equally distributed in PGY 1 through 5+. Nearly 60% of participants work in university-affiliated hospitals, followed by community (18.7%) and tertiary (13.1%) healthcare centers. More than 90% of respondents worked in a hospital that treated COVID-19 patients, while roughly 46% of those were redeployed to COVID-19 wards.
Learning Inputs
Figure 1 shows the average number of surgeries and seminars plastic surgery residents attended per week prior to and during the COVID-19 pandemic. The average number of surgeries declined from 10.01 to 5.61 per week, a 44% decrease. At the same time, the number of seminars decreased from 1.36 to 0.93 per week, an 18% decline.
Table 2 shows the percentage change in surgeries and seminars attended between prior to and during the pandemic by respondents in each country (also shown in Figure 2). Respondents from every country except for the Dominican Republic report a decrease in the number of surgeries they scrubbed in. Trainees from the Dominican Republic report that they participated in 10% more surgeries during the COVID-19 pandemic. Residents from Moldova, Japan, and the UK report the least decrease in their operation room time: − 10%, − 12%, and − 12%, respectively. On the other extreme, residents from Canada, Uruguay, Kenya, and Slovakia report that their surgical training decreased more than 70%.
Reported Changes in Learning Inputs during COVID-19 by Country Panel A: Surgeries Participated/Scrubbed in. Panel B: Seminars Attended. Notes: This map shows the percentage change between prior to and during the COVID-19 pandemic of surgeries residents participated/scrubbed in (Panel A) and seminars attended (Panel B) by country. Darker shades reflect more negatively impacted countries.
The median percentage change during the pandemic is four and seven percentage points closer to zero than the corresponding averages in surgeries (− 48% versus − 44%) and seminars (− 25% versus − 18%), respectively. This suggests that a limited number of countries had negligible or even positive percentage change in learning inputs during the pandemic, while the preponderance of nations experienced substantial declines in resident training inputs.
Learning Outputs
Figure 3 plots the survey responses regarding the impact of COVID-19 on residents’ skill and scientific knowledge. We find that 74% of the residents report a slightly negative (43.69%) or significantly negative (30.10%) impact on their surgical skill. In contrast, the scientific knowledge of plastic surgery residents was relatively preserved with 43.45% claiming slight or significant losses in their scientific knowledge attributed to the pandemic.
Table 3 shows the percentage of respondents in each country reporting slightly or significantly negative impact on their surgical skill and scientific knowledge due to the pandemic (also shown in Figure 4). Residents in the Dominican Republic, Russia, the USA, and Taiwan are the least likely to report surgical skill losses due to COVID-19. On the other extreme, residents from Turkey, the Netherlands, Mexico, Italy, Albania, Brazil, Czech Republic, and Denmark were the most likely to report a negative COVID-19 impact on their surgical dexterity. Respondents from Morocco were the only ones who did not report any surgical skill loss. Our analysis reveals a portion of countries in which residents cruised through the pandemic with their scientific knowledge intact. Six countries, Belgium, Canada, Morocco, the Netherlands, Pakistan, and Syria, had zero percent of trainees reporting scientific knowledge loss due to COVID-19. At the same time, Ethiopia, Venezuela, Serbia, and Egypt were the most heavily impacted with respect to the scientific knowledge of their trainees.
We find that the median losses level is four and one percentage point higher than the corresponding averages in surgeries (82% versus 78%) and scientific knowledge (41% versus 40%), respectively. This suggests that a limited number of countries had limited or negligible impact of COVID-19 on residents’ surgical skill, while the preponderance of nations reported sizable losses in surgical skill.
We investigate the statistical association between changes in surgeries and seminars during COVID-19 and the share of respondents reporting declined surgical skill (ρ = −0.511 with p < 0.001 for surgeries; ρ = −0.079 with p = 0.600 for seminars) and decreased scientific knowledge (ρ = −0.118 with p = 0.428 for surgeries; ρ = −0.274 with p = 0.006 for seminars). It is important to note the significant correlations between corresponding input and output (i.e., surgeries scrubbed in with surgical skill). We find weak cross-correlations between inputs and outputs (i.e., surgeries attended with scientific knowledge and seminars attended with surgical skill). This suggests limited substitutability of inputs in training. In other words, it may be challenging to make up for lost operating room time with more seminars.
COVID-19 Pandemic Burden
The COVID-19 burden of disease may reflect pressures to each country’s healthcare system and is likely to have influenced disruptions in resident training during the pandemic. Tables 2 and 3 report the pandemic-related burden of disease in each country next to the corresponding pandemic-related change in learning inputs and outputs, respectively.
We investigate the association between pandemic-induced changes in plastic surgery residents’ learning inputs and outputs, and the number of COVID-19 cases and COVID-19-related deaths through the end of 2021. We find substantial correlations between COVID-19 prevalence per country until the end of 2021 and the percentage change in the number of surgeries residents scrubbed in during COVID-19 (ρ = − 0.188 with p = 0.206 for cases; ρ = 0.202 with p = 0.174 for deaths). We find limited association between COVID-19 prevalence and the percentage change in seminars residents attended during the pandemic in each country (ρ = −0.056 with p = 0.709 for cases; ρ = 0.077 with p = 0.605 for deaths). Turning to learning outputs, we find sizable correlations between COVID-19 prevalence per country until the end of 2021 and the share of respondents reporting declined surgical skill (ρ = 0.207 with p = 0.163 for cases; ρ = 0.2840 with p = 0.053 for deaths). The correlation of COVID-19 disease burden and reported decreased scientific knowledge is found to be relatively weak (ρ = − 0.094 with p = 0.530 for cases; ρ = 0.120 with p = 0.422 for deaths).
Regional Analysis
Tables 4 and 5 show the COVID-19 impact on learning inputs (outputs) by geographical region. South America reports the largest decline in surgeries and surgical skill during the pandemic compared with other regions. Trainees in Europe, Asia, and Africa follow in terms of surgical skill losses. Plastic surgery residents in North America and Oceania seem to be the least affected by the pandemic. Even at the regional level, we observe smaller losses in areas with lower input declines (e.g., residents from North America report attending 28% more seminars during the pandemic and only 20% of them claim a negative COVID-19 impact on their scientific background).
World Bank Income Classification
Table 6 shows the percentage change in surgeries and seminars by respondents from countries in each World Bank income-level classification. We find that the decline in reported surgeries was roughly 40%, on average, across all four income classifications, suggesting a ubiquitous impact of COVID-19 on operating volume across countries regardless of their income. In contrast, we find varying levels of COVID-19 impact on the seminars trainees attended. Residents from low-income countries reported the most dramatic negative impact on seminars (i.e., more than 60% decrease). Table 7 shows the percentage of respondents reporting negative impact on their surgical skill and scientific knowledge due to the pandemic in countries in each World Bank income-level classification. Residents from low-income countries stand out, as 100% of them report a negative impact in their surgical skill and half of them report a decline in their scientific knowledge as a result of COVID-19.
Discussion
Our results show that the preponderance of plastic surgery residents across the world expects their surgical skill and scientific knowledge to be lower compared with previous cohorts due to the pandemic. Residents are much more likely to report surgical skill losses than scientific knowledge losses (i.e., 73.79% versus 43.45%). At the same time, pockets of residents may have experienced positive consequences from COVID-19 on personal and professional dimensions, such as trauma and emergency case care [14, 17]. Roughly one-third (31.31%) of residents reported no COVID-19 impact on their scientific knowledge, while more than one-fifth (20.87%) experienced a positive impact from the pandemic. Some residents might have been able to invest time in self-study or research during the pandemic, preserving their knowledge capital from depreciation [18, 31,32,33].
Digital resources, such as video recordings of operations, webinars, and teleconferences, might have also benefited residents’ scientific knowledge [18, 34]. Remedial measures that target surgical skill may be more needed than those targeting scientific knowledge. Potential remedial strategies include a surgical skills laboratory or simulating surgical procedures on practice models [35, 36].
Our results corroborate previous studies on the COVID-19 impact on the surgical logged hours of residents across surgical specialties at the national and regional level [6, 37, 38]. This suggests that our findings on learning outputs of plastic surgery residents may constitute a benchmark for the pandemic-related learning losses of residents more broadly [39,40,41,42,43,44].
Our finding that surgical skill is primarily driven by the surgeries residents scrub in and less so by seminars provides clear guidance regarding the necessary remedial strategies. Program directors, health policy makers, and health system administrators can leverage our findings into designing recovery plans that provide residents with operation room exposure to help mitigate their pandemic-induced learning losses [45].
Our results support the need for flexible training models, competency-based advancement, and regular assessment of trainees. This training approach may be best suited to mitigate crisis-driven training deficits [1]. National associations such as the American Board of Plastic Surgery and the Accreditation Council for Graduate Medical Education can lead the efforts to design effective recovery plans for plastic surgery residents [46].
Our study brings forth two contextual benchmarks of the impact of COVID-19 on the plastic surgery residents in each country: the COVID-19-related disease burden and the income level. Countries with substantial learning losses and a COVID-19 caseload close to the average (e.g., Mexico) may experience low system resilience more generally [47].Footnote 2 These countries may need to invest in fortifying their healthcare system (e.g., through resource redundancy) and in the learning recovery of their residents to ensure they become effective health professionals.
Each country’s income level may be correlated with resource availability that would make healthcare systems and training programs more resilient to crises and more likely to bounce back after a crisis. Residents in high-income countries like Japan, the UK, South Korea, and New Zealand, who suffered lower loss levels, may have better access to tools that would help them recover compared with their counterparts in less affluent countries.
This study has certain limitations. First, our focus on plastic surgery trainees limits the statistical power of our analyses. Future studies can potentially reach residents across multiple specialties. Second, our convenient non-random sample of participants represents a broad geographic distribution of resident experiences during the pandemic. At the same time, the severity of pandemic may influence the likelihood of plastic surgery residents from specific countries to participate in the study. Future studies might be able to capture the pandemic-related training disruptions of plastic surgery residents in countries or communities not reachable at this time.
Third, our self-reported measures of learning inputs and anticipated outputs may contain recall and expectation bias. Further research could explore the availability of administrative data on log books and board examinations scores to measure training inputs and outputs and obtain more accurate estimates of the COVID-19 impact.
At the same time, this study can serve as a blueprint for future research on resident training inputs and outputs, especially following system-wide shocks. The COVID-19 pandemic impaired resident training across the world. Future epidemics, natural phenomena associated with climate change, geopolitical instabilities also pose a significant threat to resident training in the future [48,49,50]. Our study contributes to a broader understanding of the resilience of each country’s resident training programs to crises. Our approach to quantifying resident learning inputs and expected outputs is general and can be applied in more contexts and specialties. Our measures of learning outputs, in particular, speak to current proposals to develop a “Surgical Preparedness Index” (SPI) to assess, monitor, and improve the resilience of training programs and healthcare systems across the world [48].
Notes
The average survey completion rate for those was less than 30%.
A low death toll combined with high learning losses in a country may be indicative of sacrificed training to save lives.
References
Weinstein DF (2022) Reengineering GME in a pandemic-looking back, and forward. N Engl J Med 386:97–100
Cucinotta D, Vanelli M (2020) WHO Declares COVID-19 a pandemic. Acta Biomed 91(1):157
Fleisher LA, Schreiber M, Cardo D, Srinivasan A (2022) Health care safety during the pandemic and beyond-building a system that ensures resilience. N Engl J Med 386(7):609–611
Bambakidis NC, Tomei KL (2020) Impact of COVID-19 on neurosurgery resident training and education. J Neurosurg 133(1):10–11
Rana T, Hackett C, Quezada T, Chaturvedi A, Bakalov V, Leonardo J, Rana S (2020) Medicine and surgery residents’ perspectives on the impact of COVID-19 on graduate medical education. Med Educ Online 25(1):1818439
Crowe CS, Lopez J, Morrison SD, Drolet BC, Janis JE (2021) The effects of the COVID-19 pandemic on resident education and wellness: a national survey of plastic surgery residents. Plast Reconstr Surg 148(3):462e–474e
CR Stewart, SR Lipner (2021) Experiences of resident dermatologists during the COVID-19 pandemic: a cross-sectional survey. Dermatol Ther
Ducournau F, Arianni M, Awwad S, Baur E-M, Beaulieu J-Y, Bouloudhnine M, Caloia M, Chagar K, Chen Z, Chin AY et al (2020) COVID-19: initial experience of an international group of hand surgeons. Hand Surg Rehabil 39(3):159–166
Mazingi D, Navarro S, Bobel MC, Dube A, Mbanje C, Lavy C (2020) Exploring the impact of COVID-19 on progress towards achieving global surgery goals. World J Surg 44(8):2451–2457
Collins C, Mahuron K, Bongiovanni T, Lancaster E, Sosa JA, Wick E (2021) Stress and the surgical resident in the COVID-19 pandemic. J Surg Educ 78(2):422–430
de Berker HT, Bressington MJ, Mayo IM, Rose A, Honeyman C (2021) Surgical training during the COVID-19 pandemic: challenges and opportunities for junior trainees. J Plast Recostr Aesthet Surg 74(3):644–710
Purdy AC, De Virgilio C, Kaji AH, Frey ES, Lee-Kong S, Inaba K, Gauvin JM, Neville AL, Donahue TR, Smith BR et al (2021) Factors associated with general surgery residents’ operative experience during the COVID-19 pandemic. JAMA Surg 156(8):767–774
Filobbos G, Sepehripour S, Kumar S (2018) Dissection of plastic surgery national selection. B R Coll Surg Engl 100(3):152–154
Leng C, Challoner T, Hausien O, Filobbos G, Baden J (2020) From chaos to a new norm: the birmingham experience of restructuring the largest plastics department in the UK in response to the COVID-19 pandemic. J Plast Recostr Aesthet Surg 73(12):2136–2141
Armstrong A, Jeevaratnam J, Murphy G, Pasha M, Tough A, Conway-Jones R, Mifsud RW, Tucker S (2020) A plastic surgery service response to COVID-19 in one of the largest teaching hospitals in Europe. J Plast Recostr Aesthet Surg 73(6):1174–1205
Walton M, Murray E, Christian MD (2020) Mental health care for medical staff and affiliated healthcare workers during the covid-19 pandemic. Eur Heart J Acute Cardiovasc Care 9(3):241–247
Cho DY, Yu JL, Um GT, Beck CM, Vedder NB, Friedrich JB (2020) The early effects of COVID-19 on plastic surgery residency training: the university of washington experience. Plast Reconstr Surg 146(2):447–454
Jahromi AH, Arnautovic A, Konofaos P et al (2020) Impact of the COVID-19 pandemic on the education of plastic surgery trainees in the United States. JMIR Med Educ 6(2):e22045
Ayush K Kapila, Michela Schettino, Yasser Farid, Socorro Ortiz, Moustapha Hamdi (2020) The impact of coronavirus disease 2019 on plastic surgery training: the resident perspective. Plast Reconstr Surg Glob Open 8(7)
Kumar S, More A, Harikar M et al (2020) The impact of COVID-19 and lockdown on plastic surgery training and practice in India. Indian J Plast Surg 53(02):273–279
Pagotto VPF, Abbas L, Goldenberg DC, Lobato RC, do Nascimento BB, Monteiro GGR, Camargo CP, de Fre-itas Busnardo F, Gemperli R (2020) The Impact of COVID-19 on the plastic surgery activity in a high- complexity university hospital in Brazil: the importance of reconstructive plastic surgery during the pandemic. Eur J Plast Surg 43(6):819–824
Zingaretti N, Negrini FC, Tel A, Tresoldi MM, Bresadola V, Parodi PC (2020) The impact of COVID-19 on plastic surgery residency training. Aesthetic Plast Surg 44(4):1381–1385
CDC Past Pandemics (2022) Center for Disease Control and Preventions, 2022. Accessed from 2 Oct 2022
WHO-Global-Initiative-for-Emergency-and-Essential-Surgical-Care (2023) Accessed from 27 Jan 2023
World Bank (2022) Country level income. The World Bank Group. https://data-helpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
Aucejo EM, French J, Araya MPU, Zafar B (2020) The impact of covid-19 on student experiences and expectations: evidence from a survey. J Public Econ 191:104271
Giustinelli P, MD Shapiro (2019) SEATE: Subjective ex ante treatment effect of health on retirement. Technical report, National Bureau of Economic Research
Peter Arcidiacono V, Hotz J, Maurel A, Romano T (2020) Ex ante returns and occupational choice. J Polit Econ 128(12):4475–4522
Wiswall M, Zafar B (2021) Human capital investments and expectations about career and family. J Polit Econ 129(5):1361–1424
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Van Denbroucke JP, Initiative S (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 147(8):573–577
Wise CE, Merrell SB, Sasnal M, Forrester JD, Hawn MT, Lau JN, Lin DT, Schmiederer IS, Spain DA, Nassar AK et al (2021) COVID-19 impact on surgical resident education and coping. J Surg Res 264:534–543
Karamitros G, Goulas S (2022) Human capital and productivity in plastic surgery research across nations. Aesthet Plast Surg. https://doi.org/10.1007/s00266-022-03223-9
Karamitros G, Goulas S (2023) Human capital and productivity in plastic surgery research during COVID-19: an artificial intelligence approach. J Plast Reconstr Aesthet Surg 78:29–32
Siotos C, Reid RR, Corcoran JF, Ko J, Agnew SP, Dorafshar AH (2021) Does pandemic crisis mean education crisis? the chicago academic plastic surgery collaborative response to COVID-19. Plast Reconst Surg 147(6):1469
Fisher M, Alba B, Duvvuri P, Kasabian AK, Thorne C, Janis JE, Gosain AK, Bradley JP, Tanna N (2020) The state of plastic surgery education outside of the operating room. Plast Reconst Surg 146(5):1189–1194
Awad L, Langridge B, Bollen E, Abdi Z, Butler PEM (2023) Development of a low-cost, remote plastic surgery skills training course during the COVID-19 pandemic. Int J Med Educ 14:1–3
Paskal AM, Jaremkow P-L, Lyszczak PM, Paskal W, Wojcik K, Jakub O-L, Paul MA (2021) Impact of COVID-19 pandemic on plastic surgery training in Europe. J Plast Recostr Aesthet Surg 75:1696–1703
Bregman DE, Cook T, Thorne C (2021) Estimated national and regional impact of covid-19 on elective case volume in aesthetic plastic surgery. Aesthet Surg J 41(3):358–369
Forrester JD, Liou R, Knowlton LM, Jou RM, Spain DA (2020) Impact of shelter-in-place order for COVID-19 on trauma activations: Santa Clara County, California, March 2020. Trauma Surg Acute Care Open 5(1):e000505
Coyan GN, Aranda-Michel E, Kilic A, Luketich JD, Okusanya O, Chu D, Morell VO, Schuchert M, Sultan I (2020) The impact of COVID-19 on thoracic surgery residency programs in the US: a program director survey. J Card Surg 35(12):3443–3448
Juprasert JM, Gray KD, Moore MXD, Obeid L, Peters AW, Fehling DX, Fahey TJ, Yeo HL (2020) Restructuring of a general surgery residency program in an epicenter of the coronavirus disease 2019 pandemic: lessons from New York city. JAMA Surg 155(9):870–875
Meneses E, McKenney M, Elkbuli A (2020) Reforming our general surgery residency pro- gram at an urban level 1 trauma center during the COVID-19 pandemic: towards maintaining resident safety and well-being. Am J Surg 220(4):847–849
Fero KE, Weinberger JM, Lerman S, Bergman J (2020) Perceived impact of urologic surgery training program modifications due to covid-19 in the United States. Urol 143:62–67
Adesoye T, Davis CH, Del Calvo H, Shaikh AF, Chegireddy V, Chan EY, Martinez S, Pei KY, Zheng F, Tariq N (2021) Optimization of surgical resident safety and education during the COVID-19 pandemic—lessons learned. J Surg Educ 78(1):315–320
Rashid P (2017) Surgical education and adult learning: integrating theory into practice. F1000Research 6:143
McGrath MH, PlasticSurgeryMilestoneWorkingGroup (2014) The plastic surgery milestone Project. J Grad Med Educ 6(1s1):222–224
Mattingly AS, Rose L, Eddington HS, Trickey AW, Cullen MR, Morris AM, Wren SM (2021) Trends in US surgical procedures and health care system response to policies curtailing elective surgical operations during the COVID-19 pandemic. JAMA Netw Open 4(12):e2138038–e2138038
NIHRGlobalHealthUnitonGlobal, Glasbey JC, Abbott TEF, Ademuyiwa A, Adisa A, AlAmeer E, Alshryda S, Arnaud AP, Kendall BB, Abou Chaar MK et al (2022) Elective surgery system strengthening: development, measurement, and validation of the surgical preparedness index across 1,632 hospitals in 119 countries. Lancet 400(10363):1607–1617
Marie Paule Kieny and Delanyo Dovlo (2015) Beyond ebola: a new agenda for resilient health systems. Lancet 385(9963):91–92
Quintana AV, Venkatraman R, Coleman SB, Martins D, Mayhew SH (2021) COP26: an opportunity to shape climate-resilient health systems and research. Lancet Planet Health 5(12):e852–e853
Funding
Open access funding provided by HEAL-Link Greece.
Author information
Authors and Affiliations
Contributions
SG has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. SG, GK helped in study concept and design, drafting of manuscript, critical revision of the manuscript for important intellectual content, and study supervision. GK, SG, PK, MW contributed to survey dissemination. GK acquired the data. SG was involved in statistical analysis and interpretation of data.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest to disclose.
Human or Animal Rights
This article does not contain any procedures with human participants or animals.
Informed Consent
This study obtained informed respondent consent.
Ethical Approval
This study was approved by the Institutional Review Board at Stanford University (protocol #63918).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Karamitros, G., Kontoes, P., Wiedner, M. et al. The Impact of COVID-19 on Plastic Surgery Residents Across the World: A Country-, Region-, and Income-level Analysis. Aesth Plast Surg 47, 2889–2901 (2023). https://doi.org/10.1007/s00266-023-03389-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-023-03389-w