Abstract
Background
The Medicine and Healthcare Products Regulatory Agency in the United Kingdom issued a Medical Device Alert (MDA/2010/025) through a press release on 31 March 2010 for clinicians not to use the Poly Implant Prothèse (PIP) implant.
Methods
Data were collected to analyze PIP and non-PIP implant failures as well as rates of capsular contracture between August 2008 and August 2012. Relevant data were retrieved for 143 patients with PIP (group A) and non-PIP (group B) implants.
Results
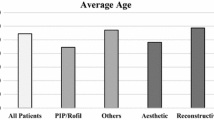
Group A (PIP): A total of 65 patients had PIP implants removed. The mean patient age was 37.1 ± 8.1 years (range 24–53 years). The mean duration of the implant was 7.2 ± 2.5 years (range 2–12 years), and the mean preoperative implant size was 327.1 ± 69.6 ml (range 255–495 ml). Of the implants in 65 patients, 18 (27.7 %) were damaged, and of the 64 patients with recorded capsular contractures, 16 (25 %) presented with grades 3 and 4 capsular contractures. Group B (non-PIP): A total of 79 patients had non-PIP implants removed. The mean patient age was 34.4 ± 8.0 years (range 19–54 years). The mean implantation time was 5.8 ± 3.9 years (range 0.2–26 years), and the mean preoperative implant size was 348.2 ± 79.0 ml (range 175–555 ml). Of the 79 patients, 6 had ruptured implants (7.6 %) and 21 (26.6 %) presented with grades 3 and 4 capsular contractures. There were no statistically significant differences in mean patient age (p = 0.046), preoperative size of the implants (p = 0.095), duration of the implantation (p = 0.08), or grades 3 and 4 capsular contractures (p = 0.830). The incidence of implant rupture was significantly higher with the PIP implants than with the non-PIP implants (p = 0.01).
Conclusion
The PIP implants were more prone to rupture than the other implants, although the incidence of clinical capsular contracture (grades 3 and 4) was not increased.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.





Similar content being viewed by others
References
Khan UD (2008) Lt unilateral breast autoinflation and intraprosthetic collection of sterile pus: an unusual operative finding of silicone gel bleed with silicone lymphadenitis. Aesthetic Plast Surg 32:684–687
Khan UD (2009) Breast autoinflation with sterile pus as a marker of implant rupture: single-stage treatment and outcome for five consecutive cases. Aesthetic Plast Surg 33:58–65
Khan UD (2009) Mondor’s disease: a review of the literature and a case report. Aesthetic Surg J 29:209–212
Khan UD (2010) Implant rupture and antegrade excision of axillary siliconoma through implant pocket. A case report and literature search. J Muhammad Med Coll 1:56–60
Medical Device Alert (2010). http://www.mhra.gov.uk/home/groups/dts-bs/documents/medicaldevicealert/con076500.pdf. Accessed 31 Mar 2010
Khan UD (2010) PIP implants investigated. Cosmetic Surg Aesth Guide 12:128–129
Poly implant prothèse (PIP) (2012) Breast implants: final report of the expert group. http://www.dh.gov.uk/health/2012/06/pip-report/. Accessed 18 Jan 2012
Bomdurant S, Ernster V, Herdman R (1999) Safety of silicon breast implants: Report of the committee on the safety of silicon breast implants (IOM). National Academy Press, Washington
Brandon HJ, Taylor ML, Powell TE, Walker PS (2007) Microscopy analysis of breast implant rupture caused by surgical instrument damage. Aesthetic Surg J 27:239–256
Brandon HJ, Young VL, Jerina KL, Wolf CJ (2001) Scanning electron microscopy characterization of surgical instrument damage to breast implants. Plast Reconstr Surg 108:52–61
Spear SL (1999) Breast implant technology: what can we count on? Aesthetic Surg J 19:347–349
Marotta J, Goldberg EP, Habel MB, Amery DP, Martin PJ, Urbaniak DJ, Widenhouse CW (2002) Silicon gel breast implant failure: evaluation of properties of shells and gels for explanted prosthesis and meta-analysis of literature rupture data. Ann Plast Surg 49:227–247
Holmich LR, Friis S, Fryzek JP, Vejborg IM, Conrad C, Sletting S, Kjoller K, McLaughlin JK, Olsen JH (2003) Incidence of silicon breast implant rupture. Arch Surg 138:801–806
Update on the safety of silicone gel-filled breast implants (FDA June 2011). http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/ImplantsandProsthetics/BreastImplants. Accessed 22 Jun 2011
Spear LS, Schwartz J, Dayan JH, Clemens MW (2009) Outcome assessment of breast distortion following submuscular breast augmentation. Aesthetic Plast Surg 33:44–48
Khan UD (2007) Muscle-splitting breast augmentation: a new pocket in a different plane. Aesthetic Plast Surg 31:553–558
Khan UD (2009) Dynamic breasts: a common complication following partial submuscular augmentation and its correction using muscle-splitting biplane technique. Aesthetic Plast Surg 33:353–360
Khan UD (2012) High transverse capsuloplasty for the correction of malpositioned implants following augmentation mammoplasty in partial submuscular plane. Aesthetic Plast Surg 36:590–599
Khan UD (2012) Secondary augmentation mammoplasties and periprosthetic infection: a three-year retrospective review of 92 secondary mammoplasties performed by a single surgeon. Aesthetic Surg J 32:465–473
Kjoller K, Holmich LR, Jacobson PH et al (2001) Capsular contracture after cosmetic breast implant surgery in Denmark. Ann Plast Surg 47:357–366
Khan UD (2010) Breast augmentation, antibiotic prophylaxis, and infection: comparative analysis of 1,628 primary augmentation mammoplasties to assess the role and efficacy of length of antibiotic prophylaxis. Aesthetic Plast Surg 34:42–47
Pajkos A, Deva AK, Vickery K, Cope C, Chang L, Cossart YE (2003) Detection of subclinical infections in significant breast implant capsules (abstract). Plast Reconstructr Surg 111:1605–1611
Acknowledgments
The statistical analysis was performed by Dr. Aamir Omair, Biostatistician in the Department of Medical Education at King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia.
Author information
Authors and Affiliations
Corresponding author
Additional information
International Master Course on Aging Skin 6/10/12/Hong Kong.
Rights and permissions
About this article
Cite this article
Khan, U.D. Poly Implant Prothèse (PIP) Incidence of Device Failure and Capsular Contracture: A Retrospective Comparative Analysis. Aesth Plast Surg 37, 906–913 (2013). https://doi.org/10.1007/s00266-013-0157-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-013-0157-6