Abstract
Purpose
Antibiotic loaded bone cement spacers provide high local antibiotic concentrations, preserve bone stock, and reduce soft tissue contractions. The objective of this in-vitro study was to compare antibiotic release from spacers, aiming to discover the most optimal preparation and identify modifiable factors that can further enhance antibiotic release.
Methods
Six distinct spacer preparation were created using three different bone cements and manual incorporation of antibiotics. During a six-week period, the release of antibiotics from each spacer was measured individually at ten predetermined time points using a chemiluminescent immunoassay.
Results
Manually adding 4 g of vancomycin to every 40 g of “Palacos R + G” yielded the most favorable release profile. Throughout all preparations, antibiotic release consistently and significantly decreased over the six-week period. When incorporating a higher concentration of vancomycin, a significantly higher cumulative release of vancomycin was observed, with varying effects on the release of gentamicin. The choice of bone cement had a significant impact on antibiotic release.
Conclusion
To enhance antibiotic release from spacers, surgeons should manually incorporate high antibiotic concentrations into the most appropriate bone cement and keep the interim period as short as possible. Specifically, we suggest manual incorporation of 4 g of vancomycin to every 40 g of gentamicin premixed "Palacos R + G" to create bone cement spacers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A periprosthetic joint infection (PJI) is one of the most serious complications after total joint replacement. According to the 2022 German Arthroplasty Registry Report (EPRD) it is the second most frequent reason for revision surgery [1]. The two-stage approach is still considered the “gold standard” treatment in the setting of most chronic PJIs [2, 3]. During first-stage surgery, the infected endoprosthesis is removed and thorough debridement is performed. After approximately six weeks, the two-stage procedure is completed with another round of thorough debridement and the insertion of a new endoprosthesis [4]. In the interim period the application of an antibiotic loaded bone cement spacer not only preserves the surrounding soft tissue and bone stock, but also results in high antibiotic concentrations within the infected joint, effectively supporting eradication of the infection [5,6,7,8,9]. Local antibiotic release has a major advantage, as it achieves high concentrations within the joint, while keeping systemic concentrations and thus the rate of adverse effects low [10,11,12]. Despite the clinical relevance and widespread use of antibiotic loaded bone cement spacers, there is limited data on antibiotic release from different preparations [13, 14]. Considering the existing literature, the practice of loading spacers with the vancomycin-gentamicin combination appears to be widely employed and highly effective against the majority of causative pathogens [10, 15,16,17,18,19,20]. But nevertheless, there are no specific recommendations available to guide surgeons in deciding which particular bone cement and antibiotic concentrations should be used for spacer fabrication. Therefore, this study aimed to examine and compare the antibiotic release of six different preparations of vancomycin and gentamicin loaded bone cement spacers over a six-week period. The main objective of this study was to determine the most ideal composition of a drug-eluting dual antibiotic loaded bone cement (dALBC) for spacer construction based on our findings. Our secondary goal was to identify modifiable factors that could enhance the release of antibiotics from bone cement spacers in general.
Materials and methods
An ethics approval was not necessary for this in vitro study, which analyzed the release of antibiotics from six different preparations (Groups A-F; Table 1) made of three different bone cements: “Copal spacem” (Heraeus Medical, Wehrheim, Germany): designed for spacer fabrication without any premixed antibiotics; “Copal G + V” (Heraeus Medical, Wehrheim, Germany): specifically formulated for revision surgery with 0.5 g of gentamicin and 2 g of vancomycin per 40 g of bone cement; “Palacos R + G” (Heraeus Medical, Wehrheim, Germany): a standard bone cement used in primary total joint replacement, containing 0.5 g of gentamicin.
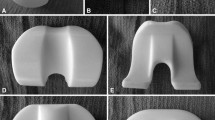
A total of 30 specimens (5 specimens from each of the 6 different preparations) were fabricated. Each spacer contained 0.5 g of gentamicin, either premixed or manually loaded (gentamicin powder, GENAXXON bioscience, Ulm, Germany) and 2 g (“low” concentration group) or 4 g (“high” concentration group) of vancomycin hydrochloride, either premixed or manually loaded (vancomycin powder, Hikma Pharmaceuticals, London, UK) per 40 g of bone cement. Manual antibiotic loading was performed following the recommendations by Kuhn et al. [21]. The powder of the added antibiotics was thoroughly ground in a mortar and then successively added to the powder of the bone cement while stirring. All cement-mixing procedures were performed without vacuum at a room temperature of 23 ± 1 °C and humidity of at least 40%. Exactly 60 s after bone cement mixing was started, the dALBCs were applied into specifically designed molds using a cement gun. The molds were clamped for an hour to achieve complete curing of the bone cement [22]. Finally, according to DIN ISO 5833 (International Organization for Standardization, Geneva, Switzerland), the surface of all specimens was carefully smoothened and measured to fulfill the geometry requirements of a rectangular block with a length of 75 ± 0.2 mm, a width of 10 ± 0.2 mm, and a total thickness of 3.3 ± 0.2 mm [23]. All specimens were then individually immersed into 40 ml of phosphate-buffered saline (PBS) with pH 7.4 at 37 °C for incubation. The antibiotic release of all specimens was separately analyzed using the chemiluminescent immunoassay (Advia Centaur XPT, Siemens Healthineers, Germany) at ten predetermined time points: five h, one day, two days, four days, one week, two weeks, three weeks, four weeks, five weeks, and six weeks. The incubation medium (40 ml of PBS) was completely replaced at each timepoint (complete wash-out), resulting in a total of 300 samples (Fig. 1).
Experimental set-up. (1) Each of the 30 dALBC spacers is immersed individually in a test tube containing 40 ml of PBS. (2) Incubation is initiated. (3) At 10 predetermined time points, the specimens are taken out from the test tubes and (4) transferred individually into new test tubes with fresh 40 ml of PBS. (5) The old test tubes are sent to the lab for analysis to determine the antibiotic concentrations of gentamicin and vancomycin within the PBS medium. Meanwhile, (2) incubation continues in new test tubes. This procedure is repeated for all time points and each spacer sample
Statistical analysis
All descriptive data is presented as the arithmetic mean, standard deviation and minimum and maximum. The Shapiro–Wilk test was performed to confirm normal distribution of the data. Then, a mixed ANOVA with post-hoc testing and Bonferroni correction was applied. The level of significance was set at p < 0.05 for all statistical tests. The statistical analyses were performed using the software SPSS (version 25.0; IBM Inc., Armonk, New York, NY, USA).
Results
Gentamicin release (Fig. 2 and Fig. 3)
Six-week mean cumulative antibiotic release of gentamicin (mg/l). (a) Comparison between two formulations of the same bone cement. (b) Comparison between the “low” concentration preparations. (c) Comparison between the “high” concentration preparations. The level of significance was set at p < 0.05 and marked with an asterisk. (* = significance; ns = no significance; low = “low” concentration group; high = “high” concentration group)
Comparison between the “low” and “high” concentration preparations of the same bone cement
The higher concentration of vancomycin had a varying impact on the release of gentamicin, depending on the type of bone cement used. A statistically significant enhancement was observed for spacers composed of Palacos R + G (group C: 149.4 mg/l ± SD 15 and group D: 226.1 mg/l ± SD 13.7; p < 0.001, respectively), but no effect was noticed for spacers made of Copal spacem (group A: 28.9 mg/l ± SD 3.2 and group B: 26.1 mg/l ± SD 1.1; p = 1.0, respectively) or Copal G + V (group E: 200.2 mg/l ± SD 24.4 and group F: 203.3 mg/l ± SD 18.7; p = 1.0, respectively).
Comparison of the three “high” concentration preparations
There was no statistically significant difference in the average cumulative concentration of gentamicin over six weeks between Palacos R + G (group D) and Copal G + V (group F): 226.1 mg/l ± SD 13.7 and 203.3 mg/l ± SD 18.7; p = 0.38, respectively. But significant differences were found in the average cumulative concentration of gentamicin between group B (26.1 mg/l ± SD 1.1) and group D (226.1 mg/l ± SD 13.7) (p < 0.001), as well as between group B (26.1 mg/l ± SD 1.1) and group F (203.3 mg/l ± SD 18.7) (p < 0.001).
Vancomycin release (Fig. 4 and Fig. 5)
Six-week mean cumulative antibiotic release of vancomycin (mg/l). (a) Comparison between the two formulations of the same bone cement. (b) Comparison between the “low” concentration preparations. (c) Comparison between the “high” concentration preparations. The level of significance was set at p < 0.05 and marked with an asterisk. (* = significance; ns = no significance; low = “low” concentration group; high = “high” concentration group)
Comparison between the “low” and “high” concentration preparations of the same bone cement
The "high" concentration groups, using 4 g of vancomycin powder per 40 g of bone cement, significantly outperformed the "low" concentration groups, using 2 g of vancomycin independent of the used bone cement. There was a significant difference in the 6-week mean cumulative release of vancomycin between group A (49.3 mg/l ± SD 2.6) and group B (110.2 mg/l ± SD 5; p < 0.001), also between group C (86.2 mg/l ± SD 8.8) and group D (293.5 mg/l ± SD 14.5; p < 0.001), and group E (91 mg/l ± SD 2.5) and group F (251.2 mg/l ± SD 13.8; p < 0.001).
Comparison of the three “high” concentration preparations
The highest six-week mean cumulative release of vancomycin was observed in spacers of group D (293.5 mg/l ± SD 14.5). They significantly outperforming spacers of group F (251.2 mg/l ± SD 13.8; p < 0.001) and group B (110.2 mg/l ± SD 5; p < 0.001). There were also significant differences in the six-week mean cumulative release of vancomycin between group B (110.2 mg/l ± SD 5) and group F (251.2 mg/l ± SD 13.8) (p < 0.001).
Discussion
In 1983, Insall et al. introduced the two-stage approach, which is still regarded as the most effective treatment for chronic PJIs [15, 24]. Critics of the two-stage approach argue that the six-week gap between stages leads to relevant mobility issues, patient discomfort, and pain. Additionally, the second-stage reimplantation is often complicated by the development of soft tissue contractures and arthrofibrosis. The use of an antibiotic-loaded bone cement spacer for the interim period is a significant enhancement to the original procedure. It helps to preserve the soft tissue envelope, maintains leg length, and provides a high dose of antibiotics locally [25,26,27]. Today, clinicians often use dALBC spacers, which effectively target an even broader range of pathogens. But an increasing number of surgeons hold the belief that commercially premixed dALBCs often lack adequate antibiotic concentrations to achieve a long-lasting bactericidal effect in the setting of PJIs. Because of this argument, the limited availability and high costs of commercially available dALBCs, it has become a common practice among many surgeons to manually add antibiotics to bone cements when constructing spacers for the interim period [5, 7, 15, 28, 29]. Despite the widespread clinical use of dALBC spacers, there are currently no specific national or international recommendations regarding the selection of particular bone cements, antibiotics, or antibiotic dosages for the construction of spacers. Consequently, the main objective of this study was to compare antibiotic release of different dALBC spacers. We have demonstrated that manual incorporation of 4 g of vancomycin to every 40 g of gentamicin premixed "Palacos R + G” resulted in the most ideal release profile over a period of six weeks. Furthermore, we have identified three key factors that surgeons can modify to enhance the release of antibiotics from dALBC spacers.
In accordance with previous studies, we have demonstrated that incorporating the same concentration of antibiotics into different bone cements results in significant variations in antibiotic release [30,31,32]. Additionally, we have demonstrated that antibiotic release consistently decreases even over the course of six weeks. Therefore, choosing the most appropriate bone cement and keeping the interim period short can have a great impact on local antibiotic concentrations and therefore infect eradication.
Frew et al. compared antibiotic release from manually prepared vancomycin-containing formulations with commercially available vancomycin-impregnated bone cements and suggests using spacers with manual incorporation of 2 g of vancomycin per 40 g of bone cement [29]. To the best of our knowledge, there are no commercially available premixed bone cements containing more than 2 g of vancomycin per 40 g of bone cement. But according to our results the "high" concentration groups, using 4 g of vancomycin powder per 40 g of bone cement, significantly outperformed the "low" concentration groups, using 2 g of vancomycin. This is objective evidence that commercially premixed dALBCs lack adequate antibiotic concentrations when used for spacer construction and therefore, we propose a new and higher standard concentration of 4 g of vancomycin per 40 g of bone cement for spacer construction. It is worth noting that the higher concentration of vancomycin had a varying impact on the release of gentamicin, depending on the type of bone cement used. A statistically significant enhancement was observed for spacers composed of “Palacos R + G”, but no effect was noticed for spacers made of “Copal spacem” or “Copal G + V”. Therefore, we recommend manually adding 4 g of vancomycin to the gentamicin premixed "Palacos R + G" to achieve a strong synergistic effect of both antibiotics. But it is important to note that manual antibiotic loading, especially with high antibiotic concentrations, can significantly decrease the mechanical strength of a bone cement, raising the risk for mechanical complications [33]. Therefore, from a legal point of view, it is crucial to obtain a written and signed informed consent prior to using manually dALBC spacers.
The current study has limitations. First of all, it is an in-vitro study and therefore, it is unlikely that all results and conclusions can be directly transferred into clinical practice. In-vivo, it is important to differentiate between antibiotic release from the spacer and antibiotic diffusion into the surrounding tissue. An in-vitro study can only address the release from the bone cement spacer, while diffusion into surrounding tissue is virtually impossible to imitate. But even the release is influenced by many factors. Therefore, we investigated the release in a highly standardized experimental setup and reduced all influencing factors by using predefined rectangular bone cement specimens instead of real joint spacers and periodically replaced the PBS incubation medium to analyze antibiotic release. Because this experimental set-up clearly does not resemble reality, we cannot definitively say that the release behaves exactly the same way in-vivo. However, it is reasonable to assume that reduced release under best-case conditions, as in our set-up, also demonstrates reduced releases in-vivo. Due to the in-vitro nature of this study, potential systemic complications arising from enhanced antibiotic release from spacers were not investigated. Therefore, it is necessary to address these issues in future clinical studies. Furthermore, our study design does not account for the potential influence of wear caused by articulating spacers on the release of antibiotics. Therefore, it is crucial to investigate this aspect in forthcoming research endeavors. Finally, our study focused on three bone cements loaded with gentamicin and vancomycin in two different concentrations. Future research should explore other cements, antibiotics, and concentrations. Nevertheless, the tested preparations are commonly used in clinical practice. Although all identified differences are statistically significant, their exact clinical impact has yet to be determined. Still, we believe, it is imperative for orthopedic surgeons to possess a comprehensive understanding of important modifiable factors and their demonstrated impact on antibiotic release from bone cement spacers.
Conclusion
In the management of chronic PJIs, it is common practice to manually incorporate antibiotics into bone cements during the construction of spacers in the operating theater. In this in-vitro study, we have identified three key factors that surgeons can modify to influence the release of antibiotics from spacers: Firstly, surgeons should keep the duration of the interim period as short as possible to effectively support infect eradication through high local antibiotic release. Secondly, the decision for a particular bone cement has significant impact on antibiotic release. And thirdly, dual antibiotic loading exhibits a synergistic effect on the release of antibiotics, particularly when employed at a high antibiotic concentration in conjunction with an appropriate bone cement. Based on the results of this study, we specifically suggest manual addition of 4 g of vancomycin to every 40 g of gentamicin premixed "Palacos R + G" for the construction of spacers.
Data availability
Available on request.
Code availability
Not applicable.
References
Grimberg A, Lützner J, Melsheimer O, Morlock M, Steinbrück A (2023) German arthroplasty registry (Endoprothesenregister Deutschland-EPRD) - Annual report 2022. https://doi.org/10.36186/reporteprd072023
Sukeik M, Haddad FS (2009) Two-stage procedure in the treatment of late chronic hip infections–spacer implantation. Int J Med Sci 6:253–257. https://doi.org/10.7150/ijms.6.253
Dombrowski ME, Wilson AE, Wawrose RA, O’Malley MJ, Urish KL, Klatt BA (2020) A Low Percentage of Patients Satisfy Typical Indications for Single-stage Exchange Arthroplasty for Chronic Periprosthetic Joint Infection. Clin Orthop Relat Res 478:1780–1786. https://doi.org/10.1097/corr.0000000000001243
Vielgut I, Sadoghi P, Wolf M, Holzer L, Leithner A, Schwantzer G, Poolman R, Frankl B, Glehr M (2015) Two-stage revision of prosthetic hip joint infections using antibiotic-loaded cement spacers: When is the best time to perform the second stage? Int Orthop 39:1731–1736. https://doi.org/10.1007/s00264-015-2751-5
Charette RS, Melnic CM (2018) Two-Stage Revision Arthroplasty for the Treatment of Prosthetic Joint Infection. Curr Rev Musculoskelet Med 11:332–340. https://doi.org/10.1007/s12178-018-9495-y
Shahpari O, Mousavian A, Elahpour N, Malahias MA, Ebrahimzadeh MH, Moradi A (2020) The Use of Antibiotic Impregnated Cement Spacers in the Treatment of Infected Total Joint Replacement: Challenges and Achievements. Arch Bone Jt Surg 8:11–20. https://doi.org/10.22038/abjs.2019.42018.2141
Anagnostakos K, Fink B (2018) Antibiotic-loaded cement spacers – lessons learned from the past 20 years. Expert Rev Med Devices 15:231–245. https://doi.org/10.1080/17434440.2018.1435270
Anagnostakos K, Kelm J (2009) Enhancement of antibiotic elution from acrylic bone cement. J Biomed Mater Res B Appl Biomater 90:467–475. https://doi.org/10.1002/jbm.b.31281
Pinsornsak P, Niruktisarn T, Surabotsopon P, Boontanapibul K (2022) Novel molded antibiotic cement spacer: is it better than handmade cement spacer for treatment of chronically infected total hip arthroplasty? Int Orthop 46:1693–1700. https://doi.org/10.1007/s00264-022-05456-4
Lunz A, Omlor GW, Schmidt G, Moradi B, Lehner B, Streit MR (2021) Quality of life, infection control, and complication rates using a novel custom-made articulating hip spacer during two-stage revision for periprosthetic joint infection. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-04274-4
Cuckler JM (2005) The infected total knee: management options. J Arthroplasty 20:33–36. https://doi.org/10.1016/j.arth.2005.03.004
Li C, Renz N, Trampuz A, Ojeda-Thies C (2020) Twenty common errors in the diagnosis and treatment of periprosthetic joint infection. Int Orthop 44:3–14. https://doi.org/10.1007/s00264-019-04426-7
Anagnostakos K, Meyer C (2017) Antibiotic Elution from Hip and Knee Acrylic Bone Cement Spacers: A Systematic Review. Biomed Res Int 2017:4657874. https://doi.org/10.1155/2017/4657874
Boelch SP, Rueckl K, Fuchs C, Jordan M, Knauer M, Steinert A, Rudert M, Luedemann M (2018) Comparison of Elution Characteristics and Compressive Strength of Biantibiotic-Loaded PMMA Bone Cement for Spacers: Copal® Spacem with Gentamicin and Vancomycin versus Palacos® R+G with Vancomycin. Biomed Res Int 2018:4323518. https://doi.org/10.1155/2018/4323518
Izakovicova P, Borens O, Trampuz A (2019) Periprosthetic joint infection: current concepts and outlook. EFORT Open Rev 4:482–494. https://doi.org/10.1302/2058-5241.4.180092
Parvizi J, Gehrke T, Chen AF (2013) Proceedings of the International Consensus on Periprosthetic Joint Infection. Bone Joint J 95-b:1450–1452. https://doi.org/10.1302/0301-620x.95b11.33135
Penner MJ, Masri BA, Duncan CP (1996) Elution characteristics of vancomycin and tobramycin combined in acrylic bone-cement. J Arthroplasty 11:939–944. https://doi.org/10.1016/s0883-5403(96)80135-5
Faschingbauer M, Bieger R, Reichel H, Weiner C, Kappe T (2016) Complications associated with 133 static, antibiotic-laden spacers after TKA. Knee Surg Sports Traumatol Arthrosc 24:3096–3099. https://doi.org/10.1007/s00167-015-3646-0
Lausmann C, Citak M, Hessling U, Wolff M, Gehrke T, Suero EM, Zahar A (2018) Preliminary results of a novel spacer technique in the management of septic revision hip arthroplasty. Arch Orthop Trauma Surg 138:1617–1622. https://doi.org/10.1007/s00402-018-3038-2
Tsung JD, Rohrsheim JA, Whitehouse SL, Wilson MJ, Howell JR (2014) Management of periprosthetic joint infection after total hip arthroplasty using a custom made articulating spacer (CUMARS); the Exeter experience. J Arthroplasty 29:1813–1818. https://doi.org/10.1016/j.arth.2014.04.013
Kühn KD, Renz N, Trampuz A (2017) Local antibiotic therapy. Unfallchirurg 120:561–572. https://doi.org/10.1007/s00113-017-0372-8
Schonhoff M, Bormann T, Knappe K, Reiner T, Stange L, Jaeger S (2021) The Effect of Cement Aging on the Stability of a Cement-in-Cement Revision Construct. Appl Sci 11:2814
ISO 5833:2002 (2002) Implants for surgery—acrylic resin cements. International Organization for Standardization, Geneva
Insall JN, Thompson FM, Brause BD (2002) Two-stage reimplantation for the salvage of infected total knee arthroplasty. 1983. J Bone Joint Surg Am 84:490. https://doi.org/10.2106/00004623-200203000-00024
Haddad FS, Masri BA, Campbell D, McGraw RW, Beauchamp CP, Duncan CP (2000) The PROSTALAC functional spacer in two-stage revision for infected knee replacements. Prosthesis of antibiotic-loaded acrylic cement. J Bone Joint Surg Br 82:807–812. https://doi.org/10.1302/0301-620x.82b6.10486
Jones CW, Selemon N, Nocon A, Bostrom M, Westrich G, Sculco PK (2019) The Influence of Spacer Design on the Rate of Complications in Two-Stage Revision Hip Arthroplasty. J Arthroplasty 34:1201–1206. https://doi.org/10.1016/j.arth.2019.02.012
Gehrke T, Alijanipour P, Parvizi J (2015) The management of an infected total knee arthroplasty. Bone Joint J 97-b:20–29. https://doi.org/10.1302/0301-620x.97b10.36475
Chalmers BP, Mabry TM, Abdel MP, Berry DJ, Hanssen AD, Perry KI (2018) Two-Stage Revision Total Hip Arthroplasty With a Specific Articulating Antibiotic Spacer Design: Reliable Periprosthetic Joint Infection Eradication and Functional Improvement. J Arthroplasty 33:3746–3753. https://doi.org/10.1016/j.arth.2018.08.016
Frew NM, Cannon T, Nichol T, Smith TJ, Stockley I (2017) Comparison of the elution properties of commercially available gentamicin and bone cement containing vancomycin with “home-made” preparations. Bone Joint J 99-b:73–77. https://doi.org/10.1302/0301-620x.99b1.Bjj-2016-0566.R1
Funk GA, Burkes JC, Cole KA, Rahaman MN, McIff TE (2018) Antibiotic Elution and Mechanical Strength of PMMA Bone Cement Loaded With Borate Bioactive Glass. J Bone Jt Infect 3:187–196. https://doi.org/10.7150/jbji.27348
Slane J, Gietman B, Squire M (2018) Antibiotic elution from acrylic bone cement loaded with high doses of tobramycin and vancomycin. J Orthop Res 36:1078–1085. https://doi.org/10.1002/jor.23722
Bitsch RG, Kretzer JP, Vogt S, Büchner H, Thomsen MN, Lehner B (2015) Increased antibiotic release and equivalent biomechanics of a spacer cement without hard radio contrast agents. Diagn Microbiol Infect Dis 83:203–209. https://doi.org/10.1016/j.diagmicrobio.2015.06.019
Lunz A, Knappe K, Omlor GW, Schonhoff M, Renkawitz T, Jaeger S (2022) Mechanical strength of antibiotic-loaded PMMA spacers in two-stage revision surgery. BMC Musculoskelet Disord 23:945. https://doi.org/10.1186/s12891-022-05895-5
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Andre Lunz and Sebastian Jaeger. The first draft of the manuscript was written by Andre Lunz and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics
An ethics approval was not required for this in-vitro study.
Consent for publication
Not applicable.
Informed consent
Not applicable.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lunz, A., Schonhoff, M., Omlor, G.W. et al. Enhanced antibiotic release from bone cement spacers utilizing dual antibiotic loading with elevated vancomycin concentrations in two-stage revision for periprosthetic joint infection. International Orthopaedics (SICOT) 47, 2655–2661 (2023). https://doi.org/10.1007/s00264-023-05922-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05922-7