Abstract
Purpose
Although various surgical procedures are available for osteochondral lesion of the talus (OLT), there is still no consensus on its best treatment. The purposes of this study were to describe a new surgical technique to treat OLT and to analyze its preliminary clinical results.
Methods
Eight patients were enrolled in this retrospective study between March 2019 and May 2022 in the Second Affiliated Hospital of Chongqing Medical University. All patients were treated by synthetic bone grafting with preserved cartilage flap via a medial malleolus osteotomy approach. The patients’ characteristics, operative time, and estimated blood loss were evaluated. Intraoperative photos, preoperative and postoperative X-ray and MRI imaging were recorded. The American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score and visual analog scale (VAS) score were also recorded before surgery and at each follow-up.
Results
At six months after the operation, all patients showed bone ingrowth and remodeling according to X-ray and MRI. No obvious defects or ladder was found on the cartilage surface of all patients according to MRI. The AOFAS score improved from 61.63 ± 8.85 (range, 49–74) to 91.13 ± 4.49 (range, 83–97) (p < 0.001) and VAS score improved from 5.50 ± 1.60 (range, 4–8) before surgery to 1.88 ± 0.83 (range, 1–3) (p < 0.001) at latest follow-up. In all eight patients, no wound infection, skin necrosis, or delayed healing of osteotomy was found.
Conclusion
We proposed a simple and effective technique that restored the shape of the cartilage surface by preserving the cartilage flap and restoring the natural congruency of the subchondral bone by synthetic bone grafting. We found satisfying clinical outcomes in short-term follow-up. Our new technique might be a new surgical option for the treatment of OLT and its effectiveness should be further evaluated.





Similar content being viewed by others
Code availability
Not applicable.
References
Kim YS, Kim TY, Koh YG (2021) Demographic predictors of concomitant osteochondral lesion of the talus in patients with chronic lateral ankle instability. Foot Ankle Orthop 6(2):1758290656. https://doi.org/10.1177/24730114211013344
DIGiovanni BF, Fraga CJ, Cohen BE, Shereff MJ (2000) Associated injuries found in chronic lateral ankle instability. Foot Ankle Int 21(10):809–815. https://doi.org/10.1177/107110070002101003
Qulaghassi M, Cho YS, Khwaja M, Dhinsa B (2021) Treatment strategies for osteochondral lesions of the talus: a review of the recent evidence. Foot 47:101805. https://doi.org/10.1016/j.foot.2021.101805
Hu Y, Yue C, Li X, Li Z, Zhou D, Xu H, Zhang N (2021) A novel medial malleolar osteotomy technique for the treatment of osteochondral lesions of the talus. Orthop J Sports Med 9(3):1813037412. https://doi.org/10.1177/2325967121989988
Chuckpaiwong B, Berkson EM, Theodore GH (2008) Microfracture for osteochondral lesions of the ankle: outcome analysis and outcome predictors of 105 cases. Arthroscopy 24(1):106–112. https://doi.org/10.1016/j.arthro.2007.07.022
Hannon CP, Bayer S, Murawski CD, Canata GL, Clanton TO, Haverkamp D, Lee JW, O'Malley MJ, Yinghui H, Stone JW (2018) Debridement, curettage, and bone marrow stimulation: proceedings of the International Consensus Meeting on cartilage repair of the ankle. Foot Ankle Int 39(1_suppl):16S–22S. https://doi.org/10.1177/1071100718779392
Ramponi L, Yasui Y, Murawski CD, Ferkel RD, DiGiovanni CW, Kerkhoffs G, Calder J, Takao M, Vannini F, Choi WJ, Lee JW, Stone J, Kennedy JG (2017) Lesion size is a predictor of clinical outcomes after bone marrow stimulation for osteochondral lesions of the talus: a systematic review. Am J Sports Med 45(7):1698–1705. https://doi.org/10.1177/0363546516668292
Guimaraes JB, Da CI, Nery C, Silva FD, Ormond FA, Carneiro BC, Nico M (2021) Osteochondral lesions of the talar dome: an up-to-date approach to multimodality imaging and surgical techniques. Skeletal Radiol 50(11):2151–2168. https://doi.org/10.1007/s00256-021-03823-7
Ikuta Y, Nakasa T, Ota Y, Kanemitsu M, Sumii J, Nekomoto A, Adachi N (2020) Retrograde drilling for osteochondral lesion of the talus in juvenile patients. Foot Ankle Orthop 5(2):683349589. https://doi.org/10.1177/2473011420916139
Nakasa T, Ikuta Y, Ota Y, Kanemitsu M, Adachi N (2019) Clinical results of bioabsorbable pin fixation relative to the bone condition for osteochondral lesion of the talus. Foot Ankle Int 40(12):1388–1396. https://doi.org/10.1177/1071100719868726
Hurley ET, Murawski CD, Paul J, Marangon A, Prado MP, Xu X, Hangody L, Kennedy JG (2018) Osteochondral autograft: proceedings of the International Consensus Meeting on cartilage repair of the ankle. Foot Ankle Int 39(1_suppl):28S–34S. https://doi.org/10.1177/1071100718781098
Jackson AT, Drayer NJ, Samona J, Dukes CA, Chen CS, Arrington EA, Ryan PM (2019) Osteochondral allograft transplantation surgery for osteochondral lesions of the talus in athletes. J Foot Ankle Surg 58(4):623–627. https://doi.org/10.1053/j.jfas.2018.11.020
Feeney KM (2022) The effectiveness of osteochondral autograft transfer in the management of osteochondral lesions of the talus: a systematic review and meta-analysis. Cureus 14(11):e31337. https://doi.org/10.7759/cureus.31337
Winkler PW, Geyer S, Walzl D, Woertler K, Paul J, Siebenlist S, Imhoff AB, Achtnich A (2022) Favorable long-term clinical and radiologic outcomes with high survivorship after autologous osteochondral transplantation of the talus. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07237-3
Smyth NA, Murawski CD, Adams SJ, Berlet GC, Buda R, Labib SA, Nunley JN, Raikin SM (2018) Osteochondral allograft: proceedings of the International Consensus Meeting on cartilage repair of the ankle. Foot Ankle Int 39(1_suppl):35S–40S. https://doi.org/10.1177/1071100718781097
Rothrauff BB, Murawski CD, Angthong C, Becher C, Nehrer S, Niemeyer P, Sullivan M, Valderrabano V, Walther M, Ferkel RD (2018) Scaffold-based therapies: proceedings of the International Consensus Meeting on cartilage repair of the ankle. Foot Ankle Int 39(1_suppl):41S–47S. https://doi.org/10.1177/1071100718781864
Hermanson E, Ferkel RD (2009) Bilateral osteochondral lesions of the talus. Foot Ankle Int 30(8):723–727. https://doi.org/10.3113/FAI.2009.0723
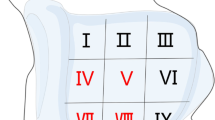
Elias I, Zoga AC, Morrison WB, Besser MP, Schweitzer ME, Raikin SM (2007) Osteochondral lesions of the talus: localization and morphologic data from 424 patients using a novel anatomical grid scheme. Foot Ankle Int 28(2):154–161. https://doi.org/10.3113/FAI.2007.0154
Funding
This research was supported by Medical Technology Innovation Project of The Second Affiliated Hospital of Chongqing Medical University.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Xiangjun Cheng designed and performed the surgery. Material preparation, data collection, and analysis were performed by Xudong Yao, Yun Zhu, and Yu Du. The first draft of the manuscript was written by Xudong Yao and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This is an observational study. The Medical Ethics Committee at the Second Affiliated Hospital of Chongqing Medical University has confirmed that no ethical approval is required.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The authors affirm that human research participants provided informed consent for publication of the images in Figs. 1 and 5.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yao, X., Yun, Z., Du, Y. et al. Synthetic bone grafting with preserved cartilage flap via a medial malleolus osteotomy approach to treat osteochondral lesion of the talus: technical note and preliminary clinical results. International Orthopaedics (SICOT) 47, 2743–2749 (2023). https://doi.org/10.1007/s00264-023-05920-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05920-9