Abstract
Purpose
The purpose of this multi-centre study was to report outcomes of a large cohort of reverse shoulder arthroplasty (RSA) at a minimum follow-up of two years and to determine patient and surgical factors that influence postoperative outcomes. The hypothesis was that surgical indication, surgical approach, and implant design would affect clinical outcomes significantly.
Methods
The authors reviewed records of 743 RSAs in patients with primary osteoarthritis (OA) with or without rotator cuff (RC) tears, secondary OA due to RC tears, and irreparable massive rotator cuff tears (mRCT). The deltopectoral (DP) approach was used in 540 and the anterosuperior (AS) approach in 203. Pre- and postoperative Constant scores (CS) were recorded. Multivariable linear analyses were performed to determine if CS was associated with indications for surgery, surgical approach, or implant design.
Results
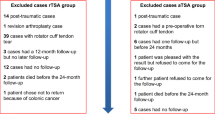
Of the 743 shoulders, 193 (25.7%) were lost to follow-up, 16 (2.1%) died, and 33 (4.4%) were revised, leaving 501 for analysis. At a mean follow-up of 3.2 ± 0.9 years, net improvement in CS was 29.2 ± 17.0. Multivariable analyses revealed that postoperative CS decreased with age and was worse in shoulders that had preoperative rotator cuff deficiency and in shoulders operated by the AS approach. Multivariable analyses also revealed worse net improvement in shoulders operated for secondary OA due to RC tears or for irreparable mRCT, as well as shoulders operated by the AS approach.
Conclusion
This large multi-centre study confirms that, at two or more years following RSA, Constant scores are not associated with implant design, but rather with rotator cuff deficiency and surgical approach. Multivariable analysis revealed that postoperative CS was worse for shoulders with preoperative rotator cuff deficiency and for shoulders operated by the AS approach. Multivariable analysis also revealed that net improvement in CS was worse in shoulders treated for secondary OA due to RC tears and for shoulders with irreparable mRCT, as well as for shoulders operated by the AS approach.

Similar content being viewed by others
References
Burden EG, Batten TJ, Smith CD, Evans JP (2021) Reverse total shoulder arthroplasty. Bone Joint J 103-b:813–821. https://doi.org/10.1302/0301-620x.103b.Bjj-2020-2101
Forlizzi JM, Puzzitiello RN, Hart PA, Churchill R, Jawa A, Kirsch JM (2022) Predictors of poor and excellent outcomes after reverse total shoulder arthroplasty. J Shoulder Elbow Surg 31:294–301. https://doi.org/10.1016/j.jse.2021.07.009
Gillespie RJ, Garrigues GE, Chang ES, Namdari S, Williams GR Jr (2015) Surgical exposure for reverse total shoulder arthroplasty: differences in approaches and outcomes. Orthop Clin North Am 46:49–56. https://doi.org/10.1016/j.ocl.2014.09.015
Carducci MP, Zimmer ZR, Jawa A (2019) Predictors of unsatisfactory patient outcomes in primary reverse total shoulder arthroplasty. J Shoulder Elbow Surg 28:2113–2120. https://doi.org/10.1016/j.jse.2019.04.009
Samitier G, Alentorn-Geli E, Torrens C, Wright TW (2015) Reverse shoulder arthroplasty. Part 1: systematic review of clinical and functional outcomes. Int J Shoulder Surg 9:24–31. https://doi.org/10.4103/0973-6042.150226
Baram A, Ammitzboell M, Brorson S, Olsen BS, Amundsen A, Rasmussen JV (2020) What factors are associated with revision or worse patient-reported outcome after reverse shoulder arthroplasty for cuff-tear arthropathy? A Study from the Danish Shoulder Arthroplasty Registry. Clin Orthop Relat Res 478:1089–1097. https://doi.org/10.1097/corr.0000000000001114
Aibinder W, Schoch B, Parsons M, Watling J, Ko JK, Gobbato B, Throckmorton T, Routman H, Fan W, Simmons C, Roche C (2021) Risk factors for complications and revision surgery after anatomic and reverse total shoulder arthroplasty. J Shoulder Elbow Surg 30:e689–e701. https://doi.org/10.1016/j.jse.2021.04.029
Neer CS 2nd, Craig EV, Fukuda H (1983) Cuff-tear arthropathy. J Bone Joint Surg Am 65:1232–1244
Hamada K, Fukuda H, Mikasa M, Kobayashi Y (1990) Roentgenographic findings in massive rotator cuff tears. a long-term observation. Clin Orthop Relat Res 254:92–96
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC (1994) Fatty muscle degeneration in cuff ruptures. pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 304:78–83
Lippe J, Spang JT, Leger RR, Arciero RA, Mazzocca AD, Shea KP (2012) Inter-rater agreement of the Goutallier, Patte, and Warner classification scores using preoperative magnetic resonance imaging in patients with rotator cuff tears. Arthroscopy 28:154–159. https://doi.org/10.1016/j.arthro.2011.07.016
Nunes J, Andrade R, Azevedo C, Ferreira NV, Oliveira N, Calvo E, Espregueira-Mendes J, Sevivas N (2022) Improved clinical outcomes after lateralized reverse shoulder arthroplasty: a systematic review. Clin Orthop Relat Res 480:949–957. https://doi.org/10.1097/corr.0000000000002065
Austin PC, Steyerberg EW (2015) The number of subjects per variable required in linear regression analyses. J Clin Epidemiol 68:627–636. https://doi.org/10.1016/j.jclinepi.2014.12.014
Rauck RC, Ruzbarsky JJ, Swarup I, Gruskay J, Dines JS, Warren RF, Dines DM, Gulotta LV (2020) Predictors of patient satisfaction after reverse shoulder arthroplasty. J Shoulder Elbow Surg 29:e67–e74. https://doi.org/10.1016/j.jse.2019.07.043
Werner BC, Wong AC, Mahony GT, Craig EV, Dines DM, Warren RF, Gulotta LV (2016) Causes of poor postoperative improvement after reverse total shoulder arthroplasty. J Shoulder Elbow Surg 25:e217–e222. https://doi.org/10.1016/j.jse.2016.01.002
Statz JM, Wagner ER, Houdek MT, Cofield RH, Sanchez-Sotelo J, Elhassan BT, Sperling JW (2016) Outcomes of primary reverse shoulder arthroplasty in patients with morbid obesity. J Shoulder Elbow Surg 25:e191–e198. https://doi.org/10.1016/j.jse.2015.12.008
Almasri M, Kohrs B, Fleckenstein CM, Nolan J, Wendt A, Hasan SS (2022) Reverse shoulder arthroplasty in patients 85 years and older is safe, effective, and durable. J Shoulder Elbow Surg 31:2287–2297. https://doi.org/10.1016/j.jse.2022.03.024
Georgoulas P, Fiska A, Ververidis A, Drosos GI, Perikleous E, Tilkeridis K (2021) Reverse shoulder arthroplasty, deltopectoral approach vs. anterosuperior approach: an overview of the literature. Front Surg 8:721054. https://doi.org/10.3389/fsurg.2021.721054
Molé D, Wein F, Dézaly C, Valenti P, Sirveaux F (2011) Surgical technique: the anterosuperior approach for reverse shoulder arthroplasty. Clin Orthop Relat Res 469:2461–2468. https://doi.org/10.1007/s11999-011-1861-7
Heifner JJ, Kumar AD, Wagner ER (2021) Glenohumeral osteoarthritis with intact rotator cuff treated with reverse shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg 30:2895–2903. https://doi.org/10.1016/j.jse.2021.06.010
Kennedy J, Klifto CS, Ledbetter L, Bullock GS (2021) Reverse total shoulder arthroplasty clinical and patient-reported outcomes and complications stratified by preoperative diagnosis: a systematic review. J Shoulder Elbow Surg 30:929–941. https://doi.org/10.1016/j.jse.2020.09.028
Acknowledgements
The authors are grateful to “GCS Ramsay Santé pour lʼEnseignement et la Recherche” for funding the statistical analysis and manuscript preparation for this study.
Contributors of ReSurg
Jacobus H Müller, MSc, PhD1
Aude Hibon, MEng1
Luca Nover, MSc1
1ReSurg SA, 1260 Nyon, Switzerland
Author information
Authors and Affiliations
Consortia
Contributions
AG, CN, MG, NB, JK, SoFEC, LNJ, PC: conceptualization, investigation, resources, supervision
ReSurg: data curation, formal analysis, writing–original draft
MS: methodology, writing–review and editing, project administration
PC: funding acquisition
Corresponding author
Ethics declarations
Conflict of interest
Arnaud Godenèche reports fees from Tornier SAS outside of the submitted work.
Cécile Nérot reports royalties from DePuy Synthes outside the submitted work.
Mathieu Girard has nothing to disclose.
Nicolas Bonnevialle reports personal fees from Stryker and Conmed outside the submitted work.
Jean Kany has nothing to disclose.
SoFEC has nothing to disclose.
Jacobus Muller, Aude Hibon, and Luca Nover (contributors to ReSurg) have nothing to disclose.
Mo Saffarini has nothing to disclose.
Laurent Nove-Josserand is a consultant and receives royalties from 3S Ortho.
Philippe Collotte is a consultant and receives royalties from 3S Ortho.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of evidence: Level IV
Institutions at which the work was performed
SoFEC-French Shoulder and Elbow Society, Paris, France
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Godenèche, A., Nérot, C., Girard, M. et al. Reverse shoulder arthroplasty renders better clinical scores at a minimum follow-up of two years for patients with no rotator cuff deficiency operated by the deltopectoral approach. International Orthopaedics (SICOT) 47, 2285–2293 (2023). https://doi.org/10.1007/s00264-023-05872-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05872-0