Abstract
Purpose
Unstable pelvic ring injury can result in a life-threatening situation and lead to long-term disability. Established classification systems, recently emerged resuscitative and treatment options as well as techniques, have facilitated expansion in how these injuries can be studied and managed. This study aims to access practice variation in the management of unstable pelvic injuries around the globe.
Methods
A standardized questionnaire including 15 questions was developed by experts from the SICOT trauma committee (Société Internationale de Chirurgie Orthopédique et de Traumatologie) and then distributed among members. The survey was conducted online for one month in 2022 with 358 trauma surgeons, encompassing responses from 80 countries (experience > 5 years = 79%). Topics in the questionnaire included surgical and interventional treatment strategies, classification, staging/reconstruction procedures, and preoperative imaging. Answer options for treatment strategies were ranked on a 4-point rating scale with following options: (1) always (A), (2) often (O), (3) seldom (S), and (4) never (N). Stratification was performed according to geographic regions (continents).
Results
The Young and Burgess (52%) and Tile/AO (47%) classification systems were commonly used. Preoperative three-dimensional (3D) computed tomography (CT) scans were utilized by 93% of respondents. Rescue screws (RS), C-clamps (CC), angioembolization (AE), and pelvic packing (PP) were observed to be rarely implemented in practice (A + O: RS = 24%, CC = 25%, AE = 21%, PP = 25%). External fixation was the most common method temporized fixation (A + O = 71%). Percutaneous screw fixation was the most common definitive fixation technique (A + O = 57%). In contrast, 3D navigation techniques were rarely utilized (A + O = 15%). Most standards in treatment of unstable pelvic ring injuries are implemented equally across the globe. The greatest differences were observed in augmented techniques to bleeding control, such as angioembolization and REBOA, more commonly used in Europe (both), North America (both), and Oceania (only angioembolization).
Conclusion
The Young-Burgess and Tile/AO classifications are used approximately equally across the world. Initial non-invasive stabilization with binders and temporary external fixation are commonly utilized, while specific haemorrhage control techniques such as pelvic packing and angioembolization are rarely and REBOA almost never considered. The substantial regional differences’ impact on outcomes needs to be further explored.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Unstable pelvic ring injuries represent a challenging injury for trauma surgeons. Established classification systems, imaging, resuscitative methods, implant options, and surgical techniques have allowed for an improved understanding, stabilization, and treatment of these injuries [1,2,3].
Unstable pelvic ring according to Young and Burgess which is based on the injury mechanism is defined as anterior poster compression (APC) type II/III, lateral compression (LC) type III, vertical shear (VS), and combined mechanism (CM) [4, 5]. Using the AO/Tile classification which relies on vertically and rotational stability, type B (partially unstable) and C (completely unstable) are indicative of an unstable pelvic ring situation [6]. The terminology of an unstable pelvic ring is used due to the concomitant disruption of major ligaments and injuries to the soft tissue and internal organs as well as venous or arterial bleeding in these fracture patterns [7]. This constellation of injuries can result in substantial haemodynamic instability with possible exsanguination and death [8, 9].
Overall, the incidence of operations of the pelvic ring is drastically rising within the last years, whereas especially the usage of minimally invasive procedures with screw fixation seems to have found its way into frequently used practice over the last decade [10]. Nowadays, percutaneous screw stabilization of the posterior pelvic ring is also performed in emergency situation (“antishock/rescue screws”), which provides an alternative to otherwise used techniques such as C-clamp application [11]. In addition, a recent survey among international trauma surgeons provides evidence that percutaneous might provoke a smaller surgical load (second hit phenomenon) in polytraumatized patients [12].
Yet even with potential long-term disability associated with these injuries, no standard treatment algorithm exists, and variability among treating surgeons remains [13]. Still, a recently published treatment algorithm treatment for unstable pelvic ring injuries highlights the relevance of the physiological status on the surgical decision-making and proposes fixation strategies according to the injury pattern [14]. Prior studies examining variability among surgeons have highlighted heterogeneity in most facets of the treatment of these injuries, including timing of definitive fixation, anatomic location of fixation, and treatment of haemodynamically unstable pelvic ring injuries [15,16,17]. This dearth of high-quality evidence may be the impetus for the substantial management variability associated with these fractures. Yet, within the current literature, there is no investigation into geographical variation of treatment for unstable pelvic ring injuries.
This study aims to evaluate similarities and differences in treatment strategies for unstable pelvic ring care among an international cohort of surgeons. To gain this knowledge, responses were collected from a standardized questionnaire completed by surgeons from an international trauma society representing a large collection of differing nations and geographic regions.
Materials and methods
Study design
The initial survey was developed by the SICOT trauma committee and other experts of pelvic ring injuries.
Pilot study: The survey was preliminarily evaluated by experienced trauma surgeons (S.H, M.T R.P, H-C.P) and members of the SICOT trauma committee; annotations and suggestions were implemented.
The survey was then disseminated among members of SICOT, and responses were collected after voluntary participation and submission of survey responses.
Ethics approval statement
The survey was anonymous and voluntary. All participants agreed to the use of their provided data. The local ethic committee disclosed a general waiver for anonymous surveys.
Survey
The questionnaire was offered between September 05 and October 05, 2022, consisting of twelve possible selections between four different categories.
Sociodemographics: (Gender, country, working experience, level of education, and treatment frequency of unstable pelvic ring injuries); five questions.
Classification systems: Options: (1) Denis classification of sacral fractures, (2) Tile/AO classification, (3) Young-Burgess classification; one question.
Prehospital phase and diagnostic: Pelvic binders/sheets, preoperative 3D CT; 4-point rating scale: (1) never, (2) seldom, (3) often, (4) always; two questions.
Initial treatment: External fixation, rescue screws, C-clamps; 4-point rating scale: (1) never, (2) seldom, (3) often, (4) always; three questions.
Treatment of bleeding: Pelvic packing, REBOA, angioembolization; 4-point rating scale: (1) never, (2) seldom, (3) often, (4) always; three questions.
Secondary surgery and reconstruction: Staging of surgeries, percutaneous techniques, navigated techniques; 4-point rating scale: (1) never, (2) seldom, (3) often, (4) always; three questions.
The survey function in Google forms (Google LLC, “Standard practice in treatment of unstable pelvic ring injuries”, Accessed 10/05/22, https://forms.gle/ajSqUCktVKaQi7gr8) was used by which anonymity was guaranteed to all participants. The online survey (Appendix 1) was distributed to the members of SICOT. One reminder was sent after four weeks to members of SICOT.
Statistical analysis
Categorical and ordinal variables are shown as count and percentages and continuous variables as mean, median, or mode (most frequent answer). Groups of continuous variables were compared with Student’s t-test. Graphics were created utilizing the R-package ggplot (R Core Team (2019), R Foundation for Statistical Computing, Vienna, Austria (https://www.R-project.org). Statistical analysis was performed using R (R Core Team (2019), R Foundation for Statistical Computing, Vienna, Austria (https://www.R-project.org)) [18]. Stratification by continent was performed. A 4-point rating scale was chosen without a category such as “sometimes” in between “often” and “seldom” to avoid a central tendency, allowing for improved isolation of the actual treatment standards.
Results
Participant’s demographics
A total of 358 participants from 80 countries completed the questionnaire. Countries from Asia were most represented (n = 177, 50%), followed by African (n = 70, 19.8%) and European (n = 63, 17.8%) countries. Participants were mostly male (n = 331, 92.7%) and most commonly in consultant positions (n = 231, 64.5%), as well as head of department (n = 48, 13.4%) or fellows (n = 46, 12.8%). Experience was stated as > ten years in 48.3% (n = 173), 5–10 years in 30.4% (n = 109), and < five years in 21.2% (n = 76) of responses. The volume of treated unstable pelvic ring injuries was quantified as one to five per months for 66.5% of the participants (n = 238), whereas 13.1% (n = 47) reported treatment of five to ten unstable pelvic ring injuries per month. Additionally, 8.7% (n = 31) of participants stated to treat more than ten unstable pelvic ring injuries per month, and 11.7% (n = 42) participating surgeons indicated to not treat any. Summaries and additional demographic information can be seen in Table 1 and Appendix (Table 7).
Classification usage
The Tile/AO classification and the Young-Burgess classification were the most utilized classification systems (Tile/AO = 51.8% (n = 183), Y&B = 47% (n = 166)). The Denis classification of sacral fractures was only utilized by 1.1% (n = 4). Regional analysis indicated South American responders favoured the Tile/AO classification (AO/Tile = 100%, n = 16), while North American surgeons showed higher use of the Y&B classification (Y&B = 65%, n = 13). Participants from other continents reported a distribution closer to a 50:50 use of AO/Tile and Y&B classifications (Table 2, Fig. 1).
Pelvic binders
The usage of pelvic binders or sheets showed high accordance among all participating surgeons with approximately 87% (n = 308) of responders stating they always or often used them in the prehospital setting (median and mode = often). Mode and median of all individual participating surgeons from all continents were either “always” or “often”. Relevant differences in usage were not apparent among continents (Table 3, Fig. 2).
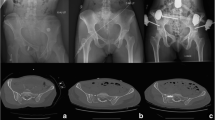
Preoperative 3D-computed tomography scan (CT scan)
65.5% and 20.8% of participants reported that they always or often used 3D CT scans preoperatively. Within each continent, the mode of responses was “always performing a preoperative 3D CT scans”. This was also observed with mean, with exception of the median from responses of surgeons in Africa, which was found to be often use of preoperative 3D CT scans (median = often) (Table 3, Fig. 2).
External fixation
Among all participants, 51.5% stated often performing external fixation (19.9% = always, 23% = seldom; mode and median = often). No large differences were observed in regard to central tendency. Individuals from all continents stated they often performed external fixation (mode), except for South American respondents, which tended to report always performing external fixation (median = often-always, mode = always) (Table 4, Fig. 3).
Rescue screw (acute percutaneous posterior pelvic ring stabilization) usage
Overall, 45.7% of respondents indicated never utilizing rescue screws and 30.3% reporting seldom use (median = seldom, mode = never). The only continent reaching a mode of “Seldom” was North America, whereas respondents from other continents most commonly answered “Never” using rescue screws, indicating a distinct lack of use outside of North America (Table 4, Fig. 3).
C-Clamp usage
C-Clamps were reported as rarely used, with 42.9% of all the participating trauma surgeons stated they never used C-clamps, while 33.3% stated seldom use (median and mode = never). The highest rate of use was observed among surgeons from Asia and Europe (median = seldom; mode Asia = seldom, mode Europe = never), whereas participants from other continents most commonly reported never using C-clamps, with calculated median and mode indicating “Never using c-clamps” (Table 4, Fig. 3).
Pelvic packing
Pelvic packing for hemostasis was reported with a central tendency to seldom performed (47%), 28% of participants stated never utilizing pelvic packing, and 19.8% stating often application of the technique. The highest rate of usage was found in surgeons from North America, though 5.3% of respondents still reported never using this technique. There was no difference in central tendencies among all continents (all continents: median and mode = seldom) (Table 5, Fig. 4).
REBOA usage
REBOA use was reportedly rare, with 67.7% of all participants stating no use and 24.7% reporting utilization (median and mode = never). Surgeons from Europe and North America indicated highest proportion of use (Europe: often = 15.9%, seldom = 39.7%; median = seldom, mode = never) (North America: often = 10%, seldom = 50%; median and Mode = seldom), whereas REBOA use by surgeons elsewhere in the world was most commonly reported as rare or never (median and mode = never) (Table 5, Fig. 4).
Angioembolization
Responses regarding angioembolization indicated rare or infrequent use (seldom = 32.4%, never = 46.2%; median = seldom, mode = never). Surgeons from Africa and Asia indicated least proportion of use (median and mode = never), followed by South America (median and mode = seldom) and Europe (median = seldom, mode = seldom-often). Surgeons from North America and Oceania reported highest usage, with 10.5% always (median = often, mode = seldom) and 42.1% often (12.5% always and 62.5% often; median and mode = often), respectively (Table 5, Fig. 4).
Percutaneous techniques
Percutaneous techniques were reported as often used by 51.1% of respondents (median and mode = often). No substantial differences were observed among surgeons within different continents (median and mode = often; median Asia = seldom-often) (Table 6, Fig. 5).
Navigated percutaneous techniques
Overall, navigated techniques were indicated as rarely utilized, with 65.4% having stated never using navigated techniques, and 19.5% reporting seldom use (median and mode = never). Surgeons from Oceania reported the highest use (median and mode = seldom), though with a small number of surgeons representing the region (n = 8) (Table 6, Fig. 5).
Secondary/staged procedures
Concerning the timing of secondary or staged procedures, 59.7% reported procession of secondary/staged procedures within the window of opportunity, whereas 30.4% reported normalization of resuscitation parameters prior to additional procedures. European (49.2%) and Oceanian (75%) surgeons reported highest proportion of reliance on normalization of resuscitative parameters as dictating their surgical timing. Surgeons from other continents indicated more frequently utilizing the window of opportunity as a gauge for surgical timing. Respondents indicating surgical procedures within 72 h were minimal (9.9%) (Table 6, Fig. 6).
Discussion
Pelvic ring injuries are associated with high-energy trauma, commonly involving multi-systems, requiring multi-disciplinary treatment and approach [8, 19]. Early approximation or restoration of native pelvic anatomy reduces pelvic volume, facilitating improved intrapelvic clot formation and haemostasis [20, 21].
Even with advancement in imaging and treatment modalities or techniques, along with improved resuscitative methods, broad international agreement in treatment of unstable pelvic ring injuries remains elusive. These fractures represent a challenge for trauma surgeons since they are associated with a high morbidity and mortality due to concomitant haemorrhage, shock, and coagulopathy [22].
Comparison and standardization of different treatment algorithms could potentially lead towards improved outcomes after these debilitating injuries. This study represents one of few studies examining international practice variation around the globe in regard to different facets of treatment for these injuries.
Study limitations
This expert opinion survey (evidence level IV) is limited to a certain degree. The questionnaire was provided to the entire SICOT society, but the demographic information of the ones not participating could not be retrieved. Therefore, it can only be assumed that the participating cohort is representative for the trauma society. Participants could only choose from and comment to predefined (treatment) options that are most common and determined by the authors. In addition, stratification was performed by continents, which implies homogenous practice in all the underlying countries. There is likely to have huge variability within practice in each continent, which is hidden in this survey. A more detailed (country-wise) analysis would not have been reasonable due to varying sample sizes.
Based on the results of this study:
-
1)
The Young-Burgess and Tile/AO classifications are the most commonly used and in approximate equal proportion.
-
2)
Initial stabilization with binders/sheet is commonly used worldwide.
-
3)
Most surgeons report temporizing stabilization of the pelvic ring with an external fixator.
-
4)
Haemostatic techniques such as pelvic packing and angioembolization are rarely used and REBOA almost never.
Our study participants reportedly use the Young-Burgess and Tile/AO classification systems equally without relevant geographic differences. The Tile/AO classification focuses primarily on posterior pelvic ring stability, whereas the YB classification emphasizes the trauma mechanisms. Prior studies have not established clinically relevant differences when comparing the classification systems in terms of mortality prediction and transfusion/infusion requirements [23]. Still, the interobserver reliability of both classification systems is frequently addressed in literature, whereas it seems that using the Young and Burgess classification provides a better agreement in between surgeons than the AO/Tile classification [24]. This suggests either classification could be used, predicated on consistence of use to improve observer reliability within the institution [24].
In this survey, majority of trauma surgeons, regardless of geographic location, indicated routine prehospital pelvic binder use. Application of a pelvic binder is widely accepted and has been associated with improved haemostasis and mortality reduction in patients with unstable pelvic ring fracture [25,26,27]. A recent study evaluated the influence of pelvic binder placement accuracy on the resuscitation requirements, whereas displacement of the binder always occurred cranially of the target structure (trochanteric region). No effect on resuscitation parameters or preclinical fluids was seen in this study [28]. Still, correct placement of the binder is of essential importance for the overall outcome [29]. We conclude that the pelvic binder is a simple and relatively benign procedure when applied correctly, with this study’s findings suggesting its use is seemingly uniformly agreed upon.
Overall, the usage of computer tomography seems to increase the agreement, especially in terms of differentiation in between stable and unstable fractures [30]. Additionally, there was wide agreement in preoperative imaging modalities, with most surgeons indicating a 3D CT is obtained preoperatively, further substantiating reports from a recent survey study [17]. The use of 3D CT allows improved evaluation of fracture morphology/classification and characteristics, as well as concomitant injury identification, such as vascular or soft tissue injuries. Prior studies have suggested that obtaining CT scans was associated with better outcome in severely injured patients [31, 32]. Yet, the overall infrastructure and localization of the computer tomography is from essential importance, whereas it needs to be performed quickly especially in haemodynamically unstable patients [33, 34]. The findings in this study are in accordance with the establishment of 3D CT scans as a reliable and beneficial imaging modality, suggesting preoperative 3D CT scans have become a standard diagnostic method for patients with unstable pelvic ring injuries [35].
Unstable pelvic ring injuries often require emergent restoration and mechanical stabilization of pelvic ring anatomy, in part to reduce bleeding and pain in patients [36, 37]. Our findings suggest that the pelvic ring is most commonly temporized with external fixation, with high accordance among surgeons who participated in this study. This is in line with recent literature reporting that surgeons tend to prefer supra-acetabular pin placement over iliac pins in a damage control setting [17, 37].
Temporal fixation with C-clamps was reported to be sparingly used, whereas a recent study reports a beneficial effect of C-clamp application on haemodynamically unstable patients in terms of the hemodynamic stabilization [38], and the high forces imparted with a C-clamp may increase risk of sacroiliac dislocation or over-compression [39]. This troublesome side effect profile has resulted in infrequent use. Gardner first described the usage of acute percutaneous posterior pelvic ring stabilization with “antishock iliosacral screws”, which are also referred to as “rescue screws” [11, 40]. However, this procedure requires substantial surgeon experience; mirrored by our findings, its use is predominated by those in high-volume centres. As such, the seemingly infrequent use of C-clamps and rescue screws might stem from these factors, and others, with unsurprising findings suggesting their use is sparse.
In the setting of persistent haemodynamic instability, further surgical interventions such as pelvic packing and/or angioembolization may be used to control pelvic bleeding [41,42,43,44]. Pelvic packing can be quickly performed within 30 min and aims to tamponade venous bleeding, which may also be performed in combination with external fixation [17, 45]. Angioembolization, in general, requires more time and institutional resources [46]. Due to the immense personnel and equipment requirements, not all trauma centres have permanent angioembolization capabilities. It is of note, however, the two techniques are not mutually exclusive, and can be utilized in tandem, and are more likely to be used in high-volume trauma centers [42, 47]. Prior studies have reported an association of angioembolization with reduction of mortality [48]. Yet, it has been discussed that this mortality reduction may be due, in part, to a requisite level of patient stability for patients to be amenable for angioembolization, as there may be increased time requirements for proper equipment and personal to perform the procedure. In contrast, patients who are too unstable to wait for angioembolization may require more expedient methods of hemostasis (e.g., pelvic packing) since angioembolization is usually performed in between two and four h [49]. Additionally, combination pelvic packing (primary) and angioembolization (secondary) has been suggested to be beneficial in patients without haemorrhage controlled primarily [50].
The use of REBOA showed a geographic skew. There was greater use in North America compared to other regions; possibly highlighting its use may require high resource institutions and more robust system processes [51]. In addition, lack of surgeon familiarity with its use, high mortality rates, and frequent complications such as vascular injury, malpositioning, postoperative thrombosis, limb amputation, and tissue necrosis may be reasons for surgeon deterrence of routine use, even in the setting of resource or institutional capabilities [52,53,54,55].
The timing of definitive reconstruction in patients with major fractures, such as a pelvic ring fractures, remains contested [56,57,58]. Early invasive surgery—especially in polytraumatized patients—may exaggerate immunologic and inflammatory responses provoking the “second hit” phenomena, possibly associated with adverse complications and outcomes [59, 60]. In response to this consideration, surgeons may consider physiologic markers or “window of opportunity” when deciding on timing of surgery. A prior study surveying European-based surgeons reported high reliance on a patient'’ physiologic status when determining timing of fracture fixation, rather than the “window of opportunity” when performing a secondary/staged reconstruction [61]. This study congruently aligned with those findings, with most surgeons identifying a patient’s physiology as the main determinant in surgical timing. Yet, even with physiologic status and response of immense importance, a large number of responding surgeons indicated utilization of the “window of opportunity” for timing of fracture fixation. In contrast, some retrospective studies suggest a more dogmatic early definitive stabilization for unstable pelvic ring injuries regardless of the physiology, reporting favorable outcomes [62,63,64]. Yet, high-quality evidence comparing various methods of determining timing of fracture fixation is lacking.
Recent publications have suggested using multiple parameters to identify when severely injured patient may be stable enough for secondary surgery [65]. Prior studies have incorporated evaluating multiple systems and parameters, such as acid–base balance, body temperature, coagulation, and tissue damage, to aid in improved prediction of early complications when compared to evaluating fewer or single parameters complications [66,67,68]. Moreover, repeated assessment of physiological parameters in patients with multi-systems injuries allows identification of patients who benefit from early fixation. Intuitively, minimally invasive surgical procedures such as percutaneous pelvic stabilization and navigation techniques allow for early fracture fixation without severely compromising the patient’s physiology commonly associated with open orthopaedic procedures [69,70,71]. These concepts were exemplified in our study, with percutaneous techniques reported as commonly used.
Conclusion
This survey of orthopaedic trauma surgeons in regard to treatment of unstable pelvic ring injuries revealed some areas of accordance and discordance in practice. Most surgeons utilize pelvic binders/sheets as an augment to initial stabilization. Additionally, most surgeons report commonly temporizing stabilization of the pelvic ring with an external fixator. Emergency stabilization of the posterior pelvic ring with C-clamps or rescue screws is less commonly performed. Haemostatic techniques such as pelvic packing and angioembolization are infrequently utilized. There was a high degree of variability in regard to determining surgical timing of sequential surgeries, which seems to be a topic under discussion. Most respondents indicated utilizing minimally invasive surgical techniques for definitive fixation of unstable pelvic ring fractures. The current survey study, with international distribution, presents regional agreements and discordances in treatment variation of unstable pelvic ring injuries. Future efforts may include comparison and evaluation of established protocols and treatment algorithms between regions of the world.
Data Availability
Data, (further) materials and code can be requested individually from the author team. The team of authors reserves the right to evaluate and decide individually to hand out the requested data/materials/code.
Abbreviations
- REBOA :
-
Resuscitative endovascular balloon occlusion of the aorta
- Tile/AO :
-
Tile/AO classification
- Y&B :
-
Young and Burgess classification
- APC :
-
Anterior posterior compression
- LC :
-
Lateral compression
- VS :
-
Vertical shear
- CM :
-
Combined mechanism
References
Alton TB, Gee AO (2014) Classifications in brief: young and burgess classification of pelvic ring injuries. Clin Orthop Relat Res 472:2338–2342
Tile M, Helfet DL, Kellam JF, Vrahas M (2015) Fractures of the Pelvis and Acetabulum. https://doi.org/10.1055/b-003-121618
Young JW, Burgess AR, Brumback RJ, Poka A (1986) Pelvic fractures: value of plain radiography in early assessment and management. Radiology 160:445–451
Mi M, Kanakaris NK, Wu X, Giannoudis PV (2021) Management and outcomes of open pelvic fractures: An update. Injury 52:2738–2745
Burgess AR, Eastridge BJ, Young JW, Ellison TS, Ellison PS Jr, Poka A, Bathon GH, Brumback RJ (1990) Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma 30:848–856
Tile M, Pennal GF (1980) Pelvic disruption: principles of management. Clin Orthop Relat Res 56–64. https://pubmed.ncbi.nlm.nih.gov/7418324/
Smith W, Williams A, Agudelo J, Shannon M, Morgan S, Stahel P, Moore E (2007) Early predictors of mortality in hemodynamically unstable pelvis fractures. J Orthop Trauma 21:31–37
Gänsslen A, Hildebrand F, Pohlemann T (2012) Management of hemodynamic unstable patients “in extremis” with pelvic ring fractures. Acta Chir Orthop Traumatol Cech 79:193–202
Giannoudis PV, Pape HC (2004) Damage control orthopaedics in unstable pelvic ring injuries. Injury 35:671–677
Lodde MF, Katthagen JC, Riesenbeck O, Raschke MJ, Hartensuer R (2021) Trends in the surgical treatment of fractures of the pelvic ring : a nationwide analysis of operations and procedures code (OPS) data between 2005 and 2017. Unfallchirurg 124:373–381
Gardner MJ, Chip Routt ML Jr (2010) The antishock iliosacral screw. J Orthop Trauma 24:e86-89
Klingebiel FK, Hasegawa M, Strähle O, Kalbas Y, Teuben M, Halvachizadeh S, Kumabe Y, Pape HC, Pfeifer R (2023) Surgical load in major fractures - results of a survey on the optimal quantification and timing of surgery in polytraumatized patients. Int Orthop 47:1677–1687. https://doi.org/10.1007/s00264-023-05828-4
Furey AJ, O’Toole RV, Nascone JW, Copeland CE, Turen C, Sciadini MF (2010) Surgeon variability in the treatment of pelvic ring injuries. Orthopedics 33:714
Tiziani S, Halvachizadeh S, Knöpfel A, Pfeifer R, Sprengel K, Tarkin I, Pape HC (2021) Early fixation strategies for high energy pelvic ring injuries - the Zurich algorithm. Injury 52:2712–2718
Moed BR, Barla J, Israel HA, Tovar S, Joeris A (2019) Current trends in the surgical treatment of open-book pelvic ring injuries: an international survey among experienced trauma surgeons. J Orthop Trauma 33(Suppl 2):S61-s65
Beckmann JT, Presson AP, Curtis SH, Haller JM, Stuart AR, Higgins TF, Kubiak EN (2014) Operative agreement on lateral compression-1 pelvis fractures. a survey of 111 OTA members. J Orthop Trauma 28:681–685
Parry JA, Funk A, Heare A, Stacey S, Mauffrey C, Starr A, Crist B, Krettek C, Jones CB, Kleweno CP, Firoozabadi R, Sagi HC, Archdeacon M, Eastman J, Langford J, Oransky M, Martin M, Cole P, Giannoudis P, Byun SE, Morgan SJ, Smith W, Giordano V, Trikha V (2021) An international survey of pelvic trauma surgeons on the management of pelvic ring injuries. Injury 52:2685–2692
Carstensen B, Plummer M, Laara E, Hills M (2022) Epi: a pack age for statistical analysis in epidemiology. R package version 2.47.1. https://cran.r-project.org/web/packages/Epi/citation.html
Balogh Z, King KL, Mackay P, McDougall D, Mackenzie S, Evans JA, Lyons T, Deane SA (2007) The epidemiology of pelvic ring fractures: a population-based study. J Trauma 63:1066–1073 (discussion 1072-1063)
Tzioupis CC, Kobbe P, Tarkin IS, Pape HC (2007) Pelvic stabilization Prehospital management of traumatic pelvic injuries. Jems 32:64–66 (68, 70-65; quiz 76)
Pastor T, Tiziani S, Kasper CD, Pape HC, Osterhoff G (2019) Quality of reduction correlates with clinical outcome in pelvic ring fractures. Injury 50:1223–1226
Stahel PF, Burlew CC, Moore EE (2017) Current trends in the management of hemodynamically unstable pelvic ring injuries. Curr Opin Crit Care 23:511–519
Osterhoff G, Scheyerer MJ, Fritz Y, Bouaicha S, Wanner GA, Simmen HP, Werner CM (2014) Comparing the predictive value of the pelvic ring injury classification systems by Tile and by Young and Burgess. Injury 45:742–747
Berger-Groch J, Thiesen DM, Grossterlinden LG, Schaewel J, Fensky F, Hartel MJ (2019) The intra- and interobserver reliability of the Tile AO, the Young and Burgess, and FFP classifications in pelvic trauma. Arch Orthop Trauma Surg 139:645–650
Jain S, Bleibleh S, Marciniak J, Pace A (2013) A national survey of United Kingdom trauma units on the use of pelvic binders. Int Orthop 37:1335–1339
Jang JY, Bae KS, Kang BH, Lee GJ (2022) Comparison between external fixation and pelvic binder in patients with pelvic fracture and haemodynamic instability who underwent various haemostatic procedures. Sci Rep 12:3664
Audretsch CK, Mader D, Bahrs C, Trulson A, Höch A, Herath SC, Küper MA (2021) Comparison of pelvic C-clamp and pelvic binder for emergency stabilization and bleeding control in type-C pelvic ring fractures. Sci Rep 11:2338
Tiziani S, Janett AS, Alkadhi H, Osterhoff G, Sprengel K, Pape HC (2022) Does the accuracy of prehospital pelvic binder placement affect cardiovascular physiological parameters during rescue? A clinical study in patients with pelvic ring injuries. OTA Int 5:e186
Coccolini F, Stahel PF, Montori G, Biffl W, Horer TM, Catena F, Kluger Y, Moore EE, Peitzman AB, Ivatury R, Coimbra R, Fraga GP, Pereira B, Rizoli S, Kirkpatrick A, Leppaniemi A, Manfredi R, Magnone S, Chiara O, Solaini L, Ceresoli M, Allievi N, Arvieux C, Velmahos G, Balogh Z, Naidoo N, Weber D, Abu-Zidan F, Sartelli M, Ansaloni L (2017) Pelvic trauma: WSES classification and guidelines. World J Emerg Surg 12:5
Koo H, Leveridge M, Thompson C, Zdero R, Bhandari M, Kreder HJ, Stephen D, McKee MD, Schemitsch EH (2008) Interobserver reliability of the young-burgess and tile classification systems for fractures of the pelvic ring. J Orthop Trauma 22:379–384
Huber-Wagner S, Lefering R, Kanz KG, Biberthaler P, Stengel D (2017) The importance of immediate total-body CT scanning. Lancet 389:502–503
Huber-Wagner S, Kanz KG, Hanschen M, van Griensven M, Biberthaler P, Lefering R (2018) Whole-body computed tomography in severely injured patients. Curr Opin Crit Care 24:55–61
Huber-Wagner S, Biberthaler P, Häberle S, Wierer M, Dobritz M, Rummeny E, van Griensven M, Kanz KG, Lefering R (2013) Whole-body CT in haemodynamically unstable severely injured patients–a retrospective, multicentre study. PLoS ONE 8:e68880
Lendemans S, Ruchholtz S (2012) S3 guideline on treatment of polytrauma/severe injuries. Trauma room care. Unfallchirurg 115:14–21
Pérez RM, Chana FR, Vaquero JM (2010) Utility of 3D computed tomography for the surgical planning of pelvic fractures. Acta Ortop Mex 24:306–311
Poenaru DV, Popescu M, Anglitoiu B, Popa I, Andrei D, Birsasteanu F (2015) Emergency pelvic stabilization in patients with pelvic posttraumatic instability. Int Orthop 39:961–965
Tiziani S, Dienstknecht T, Osterhoff G, Hand TL, Teuben M, Werner CML, Pape HC (2019) Standards for external fixation application: national survey under the auspices of the German Trauma Society. Int Orthop 43:1779–1785
Gewiess J, Luedi MM, Schnüriger B, Tosounidis TH, Keel MJB, Bastian JD (2022) Effect of C-clamp application on hemodynamic instability in polytrauma victims with pelvic fracture. Medicina (Kaunas) 58:1291. https://doi.org/10.3390/medicina58091291
Bartlett C, Asprinio D, Louis S, Helfet D (1997) Intrapelvic dislocation of the left hemipelvis as a complication of the pelvic “C” clamp: a case report and review. J Orthop Trauma 11:540–542
Benders KEM, Leenen LPH (2020) Management of hemodynamically unstable pelvic ring fractures. Front Surg 7:601321
Karadimas EJ, Nicolson T, Kakagia DD, Matthews SJ, Richards PJ, Giannoudis PV (2011) Angiographic embolisation of pelvic ring injuries. Treatment algorithm and review of the literature. Int Orthop 35:1381–1390
Hundersmarck D, Hietbrink F, Leenen LPH, Heng M (2021) Pelvic packing and angio-embolization after blunt pelvic trauma: a retrospective 18-year analysis. Injury 52:946–955
Cothren CC, Osborn PM, Moore EE, Morgan SJ, Johnson JL, Smith WR (2007) Preperitonal pelvic packing for hemodynamically unstable pelvic fractures: a paradigm shift. J Trauma 62:834–839 (discussion 839-842)
Burlew CC (2017) Preperitoneal pelvic packing for exsanguinating pelvic fractures. Int Orthop 41:1825–1829
Ertel W, Keel M, Eid K, Platz A, Trentz O (2001) Control of severe hemorrhage using C-clamp and pelvic packing in multiply injured patients with pelvic ring disruption. J Orthop Trauma 15:468–474
Ciriano Hernández P, Moreno Hidalgo A, Grao Torrente I, Ruiz Moreno C, Seisdedos Rodrigez L, Kayser Mata S, Echenagusia Boyra MJ, González Leyte M, Pérez Díaz MD, Turégano Fuentes F (2019) Pelvic fractures with associated retroperitoneal hematoma: time until angioembolization and results. Cir Esp (Engl Ed) 97:261–267
Lustenberger T, Störmann P, Eichler K, Nau C, Janko M, Marzi I (2020) Secondary angio-embolization after emergent pelvic stabilization and pelvic packing is a safe option for patients with persistent hemorrhage from unstable pelvic ring injuries. Front Surg 7:601140
Anand T, El-Qawaqzeh K, Nelson A, Hosseinpour H, Ditillo M, Gries L, Castanon L, Joseph B (2023) Association between hemorrhage control interventions and mortality in us trauma patients with hemodynamically unstable pelvic fractures. JAMA Surg 158:63–71
Devaney GL, King KL, Balogh ZJ (2022) Pelvic angioembolization: how urgently needed? Eur J Trauma Emerg Surg 48:329–334
McDonogh JM, Lewis DP, Tarrant SM, Balogh ZJ (2022) Preperitoneal packing versus angioembolization for the initial management of hemodynamically unstable pelvic fracture: a systematic review and meta-analysis. J Trauma Acute Care Surg 92:931–939
Werner NL, Moore EE, Hoehn M, Lawless R, Coleman JR, Freedberg M, Heelan AA, Platnick KB, Cohen MJ, Coleman JJ, Campion EM, Fox CJ, Mauffrey C, Cralley A, Pieracci FM, Burlew CC (2022) Inflate and pack! Pelvic packing combined with REBOA deployment prevents hemorrhage related deaths in unstable pelvic fractures. Injury 53:3365–3370
Castellini G, Gianola S, Biffi A, Porcu G, Fabbri A, Ruggieri MP, Coniglio C, Napoletano A, Coclite D, D’Angelo D, Fauci AJ, Iacorossi L, Latina R, Salomone K, Gupta S, Iannone P, Chiara O (2021) Resuscitative endovascular balloon occlusion of the aorta (REBOA) in patients with major trauma and uncontrolled haemorrhagic shock: a systematic review with meta-analysis. World J Emerg Surg 16:41
Granieri S, Frassini S, Cimbanassi S, Bonomi A, Paleino S, Lomaglio L, Chierici A, Bruno F, Biondi R, Di Saverio S, Khan M, Cotsoglou C (2022) Impact of resuscitative endovascular balloon occlusion of the aorta (REBOA) in traumatic abdominal and pelvic exsanguination: a systematic review and meta-analysis. Eur J Trauma Emerg Surg 48:3561–3574
Coccolini F, Ceresoli M, McGreevy DT, Sadeghi M, Pirouzram A, Toivola A, Skoog P, Idoguchi K, Kon Y, Ishida T, Matsumura Y, Matsumoto J, Reva V, Maszkowski M, Fugazzola P, Tomasoni M, Cicuttin E, Ansaloni L, Zaghi C, Sibilla MG, Cremonini C, Bersztel A, Caragounis EC, Falkenberg M, Handolin L, Oosthuizen G, Szarka E, Manchev V, Wannatoop T, Chang SW, Kessel B, Hebron D, Shaked G, Bala M, Ordoñez CA, Hibert-Carius P, Chiarugi M, Nilsson KF, Larzon T, Gamberini E, Agnoletti V, Catena F, Hörer TM (2020) Aortic balloon occlusion (REBOA) in pelvic ring injuries: preliminary results of the ABO Trauma Registry. Updates Surg 72:527–536
Ribeiro Junior MAF, Feng CYD, Nguyen ATM, Rodrigues VC, Bechara GEK, de-Moura RR, Brenner M (2018) The complications associated with resuscitative endovascular balloon occlusion of the aorta (REBOA). World J Emerg Surg 13:20
Kalbas Y, Pape HC (2022) What factors determine a “major fracture”? Injury 53:2701–2703
Kalbas Y, Klingebiel FK, Halvachizadeh S, Kumabe Y, Scherer J, Teuben M, Pfeifer R, Pape HC (2023) Developments in the understanding of staging a "major fracture" in polytrauma: results from an initiative by the polytrauma section of ESTES. Eur J Trauma Emerg Surg. https://doi.org/10.1007/s00068-023-02245-5
Pape HC, Giannoudis P, Krettek C (2002) The timing of fracture treatment in polytrauma patients: relevance of damage control orthopedic surgery. Am J Surg 183:622–629
Keel M, Trentz O (2005) Pathophysiology of polytrauma. Injury 36:691–709
Pape HC, Halvachizadeh S, Leenen L, Velmahos GD, Buckley R, Giannoudis PV (2019) Timing of major fracture care in polytrauma patients - an update on principles, parameters and strategies for 2020. Injury 50:1656–1670
Scherer J, Coimbra R, Mariani D, Leenen L, Komadina R, Peralta R, Fattori L, Marzi I, Wendt K, Gaarder C, Pape HC, Pfeifer R (2022) Standards of fracture care in polytrauma: results of a Europe-wide survey by the ESTES polytrauma section. Eur J Trauma Emerg Surg. https://doi.org/10.1007/s00068-022-02126-3
Enninghorst N, Toth L, King KL, McDougall D, Mackenzie S, Balogh ZJ (2010) Acute definitive internal fixation of pelvic ring fractures in polytrauma patients: a feasible option. J Trauma 68:935–941
Vallier HA, Cureton BA, Ekstein C, Oldenburg FP, Wilber JH (2010) Early definitive stabilization of unstable pelvis and acetabulum fractures reduces morbidity. J Trauma 69:677–684
Devaney GL, Bulman J, King KL, Balogh ZJ (2020) Time to definitive fixation of pelvic and acetabular fractures. J Trauma Acute Care Surg 89:730–735
Pfeifer R, Klingebiel FK, Halvachizadeh S, Kalbas Y, Pape HC (2023) How to clear polytrauma patients for fracture fixation: results of a systematic review of the literature. Injury 54:292–317
Roberts DJ, Bobrovitz N, Zygun DA, Ball CG, Kirkpatrick AW, Faris PD, Brohi K, D’Amours S, Fabian TC, Inaba K, Leppäniemi AK, Moore EE, Navsaria PH, Nicol AJ, Parry N, Stelfox HT (2016) Indications for use of damage control surgery in civilian trauma patients: a content analysis and expert appropriateness rating study. Ann Surg 263:1018–1027
Roberts DJ, Bobrovitz N, Zygun DA, Ball CG, Kirkpatrick AW, Faris PD, Parry N, Nicol AJ, Navsaria PH, Moore EE, Leppäniemi AK, Inaba K, Fabian TC, D’Amours S, Brohi K, Stelfox HT (2015) Indications for use of thoracic, abdominal, pelvic, and vascular damage control interventions in trauma patients: a content analysis and expert appropriateness rating study. J Trauma Acute Care Surg 79:568–579
Roberts DJ, Bobrovitz N, Zygun DA, Ball CG, Kirkpatrick AW, Faris PD, Stelfox HT (2015) Indications for use of damage control surgery and damage control interventions in civilian trauma patients: a scoping review. J Trauma Acute Care Surg 78:1187–1196
Blum L, Hake ME, Charles R, Conlan T, Rojas D, Martin MT, Mauffrey C (2018) Vertical shear pelvic injury: evaluation, management, and fixation strategies. Int Orthop 42:2663–2674
Giannoudis PV, Tzioupis CC, Pape HC, Roberts CS (2007) Percutaneous fixation of the pelvic ring: an update. J Bone Joint Surg Br 89:145–154
Lu S, Yang K, Lu C, Wei P, Gan Z, Zhu Z, Tan H (2021) O-arm navigation for sacroiliac screw placement in the treatment for posterior pelvic ring injury. Int Orthop 45:1803–1810
Acknowledgements
The authors thank the SICOT Trauma Research Group for their continuous support and valuable contribution in designing and conducting this study.
SICOT Trauma Research Group
Turki Bashir Al-Rouk (Orthopaedic Department, Al Khadra Hospital, Tripoli), Zsolt J. Balogh (John Hunter Hospital and University of Newcastle, Newcastle), Bergita Ganse (Clinics and Institutes of Surgery, Saarland University), Marc Hanschen (Technical University of Munich, Klinikum rechts der Isar), Ilir Hasani (University Clinic for Traumatology, Skopje), Felix Karl-Ludwig Klingebiel (Traumatology Department, University Hospital Zurich), Gleb Korobushkin (Pirogov Russian National Research Medical University, Moscow), Yohei Kumabe (Department of Orthopaedic Surgery, Kobe University Graduate School of Medicine), Jeannie McCaul (Department of Orthopaedic Surgery, Groote Schuur Hospital, Cape town), Joshua A Parry (Denver Health, University of Colorado School of Medicine, Denver), Mohamed Rashed (Lybian board of orthopaedics/Chair, Tripoli), Jordan Saveski (University Clinic for Traumatology, Medical Faculty, Skopje), Hemant Sharma (Trauma & Orthopaedics, Hull York Medical School, Hull), Mohammed Zarti (Orthopaedic Department, Al Khadra Hospital, Tripoli), Roman Pfeifer (Traumatology Department, University Hospital Zurich), Boris A Zelle (University of Texas Health Science Centre at San Antonio, San Antonio).
Funding
Open access funding provided by University of Zurich
Author information
Authors and Affiliations
Consortia
Contributions
F.K.L.K.: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing–original draft, Writing–review and editing.
M.H.: Conceptualization, Investigation, Writing–original draft, English correction, Writing–review and editing.
J.P.: Conceptualization, Methodology, Writing–review and editing.
Z.J.B.: Conceptualization, Methodology, Writing–review and editing.
R.K.S.: Conceptualization, Methodology, Writing–review and editing.
Y.K.: Methodology, Writing–original draft, Writing–review and editing.
M.T.: Methodology, Writing–original draft, Writing–review and editing.
S.H.: Methodology, Writing–original draft, Writing–review and editing.
H.-C.P.: Conceptualization, Project administration, Supervision, Writing–review and editing.
R.P.: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing–review and editing.
All authors read and approved the final article.
Corresponding author
Ethics declarations
Ethical approval
The local ethic committee of the University Hospital Zurich disclosed a general waiver for anonymous surveys.
Consent to participate and publish
As this study was conducted as voluntary anonymous survey with the aim of publishing the obtained results, the participants agreed to the use and publication of their data by completing the questionnaire.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Survey Google forms “Standard practice in treatment of unstable pelvis ring injuries”
-
1.
Gender
-
a.
Male
-
b.
Female
-
a.
-
2.
Level of education/training
-
a.
Intern
-
b.
Resident
-
c.
Fellow
-
d.
Consultant/Attending
-
e.
Head of Department
-
a.
-
3.
Professional experience (in years)
-
a.
< 5 years
-
b.
5–10 years
-
c.
> 10 years
-
a.
-
4.
Number of unstable pelvic ring injuries treated in your institution (per month)
-
a.
0 per month
-
b.
1–5 per month
-
c.
5–10 per month
-
d.
> 10 per month
-
a.
-
5.
Country of your current employment
-
a.
[Free to fill]
-
a.
-
6.
What classification system is routinely or primarily used to classify high-energy pelvic ring injuries in your institution?
-
a.
Young-Burgess Classification
-
b.
Tile/AO Classification
-
c.
Denis Classification of Sacral Fractures
-
a.
-
7.
How often do you use pelvic binders/sheets in pre-hospital/trauma bay setting?
-
a.
Always
-
b.
Often
-
c.
Seldom
-
d.
Never
-
a.
-
8.
Hof often do you use “Rescue Screws”* for emergency stabilization of unstable pelvic ring fractures? (*Percutaneous screws of the posterior pelvic ring placed in case of emergency)
-
a.
Always
-
b.
Often
-
c.
Seldom
-
d.
Never
-
a.
-
9.
In your practice, how often in practice is pelvic packing performed in patients with pelvic ring injures and hemorrhage?
-
a.
Always
-
b.
Often
-
c.
Seldom
-
d.
Never
-
a.
-
10.
In your practice, how often is pelvic external fixation performed in patients with pelvic ring injures and hemorrhage?
-
a.
Always
-
b.
Often
-
c.
Seldom
-
d.
Never
-
a.
-
11.
How often is REBOA* performed for hemorrhage control in patients with pelvic fractures in your setting? (*Resuscitative endovascular balloon occlusion of the aorta)
-
a.
Always
-
b.
Often
-
c.
Seldom
-
d.
Never
-
a.
-
12.
How often is angioembolization utilized in patients with pelvic ring injuries and pelvic bleeding?
-
a.
Always
-
b.
Often
-
c.
Seldom
-
d.
Never
-
a.
-
13.
When do you perform secondary surgery (reconstruction in a staged procedure) in patients with high-energy pelvic ring injures?
-
a.
As soon as resuscitation parameters have normalized
-
b.
Within 72 h
-
c.
Always wait for the window of opportunity (5 days)
-
a.
-
14.
In your practice, how often is percutaneous techniques with navigation-guided technology used to stabilize pelvic ring injuries?
-
a.
Always
-
b.
Often
-
c.
Seldom
-
d.
Never
-
a.
-
15.
How often do you obtain a Three-Dimensional (3D) computed tomography (CT) scan to plan treatment of unstable pelvic ring injuries?
-
a.
Always
-
b.
Often
-
c.
Seldom
-
d.
Never
-
a.
-
16.
Comments (optional)
-
a.
[Free to fill]
-
a.
Appendix 2
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Klingebiel, F.KL., Hasegawa, M., Parry, J. et al. Standard practice in the treatment of unstable pelvic ring injuries: an international survey. International Orthopaedics (SICOT) 47, 2301–2318 (2023). https://doi.org/10.1007/s00264-023-05859-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05859-x