Abstract
Purpose
The reason for graft failure after anterior cruciate ligament reconstruction (ACLR) is multifactorial. Controversies remain regarding the predominant factor and incidence of failure aetiology in the literature. This review aimed to provide a meta-analysis of the literature to evaluate the relative proportion of various failure modes among patients with ACLR failure.
Methods
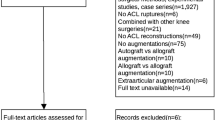
The PubMed, Embase, Cochrane Library, Web of Science, and EBSCO databases were searched for literature on ACLR failure or revision from 1975 to 2021. Data related to causes for ACLR surgical failure were extracted, and a random effects model was used to pool the results, which incorporates potential heterogeneity. Failure modes were compared between different populations, research methods, graft types, femoral portal techniques, and fixation methods by subgroup analysis or linear regression. Funnel plots were used to identify publication bias and small-study effects.
Results
A total of 39 studies were analyzed, including 33 cohort studies and six registry-based studies reporting 6578 failures. The results showed that among patients with ACLR failure or revision, traumatic reinjury was the most common failure mode with a rate of 40% (95% CI: 35–44%), followed by technical error (34%, 95% CI: 28–42%) and biological failure (11%, 95% CI: 7–15%). Femoral tunnel malposition was the most common cause of the technical error (29%, 95% CI: 18–41%), with more than two times higher occurrence than tibial tunnel malposition (11%, 95% CI: 6–16%). Traumatic reinjury was the most common factor for ACLR failure in European populations and in recent studies, while technical errors were more common in Asian populations, earlier studies, and surgery performed using the transtibial (TT) portal technique. Biological factors were more likely to result in ACLR failure in hamstring (HT) autografts compared to bone-patellar tendon-bone (BPTB) autografts.
Conclusion
Trauma is the most important factor leading to surgical failure or revision following ACLR. Technical error is also an important contributing factor, with femoral tunnel malposition being the leading cause of error resulting in failure.






Similar content being viewed by others
Data availability
Data and materials could be acquired by contacting the corresponding author.
References
Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE (2012) Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med 22:116–121. https://doi.org/10.1097/JSM.0b013e318246ef9e
Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA (2016) Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med 50:804–808. https://doi.org/10.1136/bjsports-2016-096031
Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE (2014) Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med 42:1567–1573. https://doi.org/10.1177/0363546514530088
Sanders TL, MaraditKremers H, Bryan AJ, Larson DR, Dahm DL, Levy BA, Stuart MJ, Krych AJ (2016) Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med 44:1502–1507. https://doi.org/10.1177/0363546516629944
Lefevre N, Klouche S, Mirouse G, Herman S, Gerometta A, Bohu Y (2017) Return to sport after primary and revision anterior cruciate ligament reconstruction: a prospective comparative study of 552 patients from the FAST cohort. Am J Sports Med 45:34–41. https://doi.org/10.1177/0363546516660075
Grassi A, Carulli C, Innocenti M, Mosca M, Zaffagnini S, Bait C (2018) New trends in anterior cruciate ligament reconstruction: a systematic review of national surveys of the last 5 years. Joints 6:177–187. https://doi.org/10.1055/s-0038-1672157
Lind M, Menhert F, Pedersen AB (2012) Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med 40:1551–1557. https://doi.org/10.1177/0363546512446000
Grassi A, Kim C, Muccioli GMM, Zaffagnini S, Amendola A (2017) What is the mid-term failure rate of revision ACL reconstruction? A systematic review. Clin Orthop Relat Res 475:2484–2499. https://doi.org/10.1007/s11999-017-5379-5
Wright RW, Gill CS, Chen L, Brophy RH, Matava MJ, Smith MV, Mall NA (2012) Outcome of revision anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am 94:531–536. https://doi.org/10.2106/jbjs.K.00733
Csintalan RP, Inacio MC, Funahashi TT, Maletis GB (2014) Risk factors of subsequent operations after primary anterior cruciate ligament reconstruction. Am J Sports Med 42:619–625. https://doi.org/10.1177/0363546513511416
George MS, Dunn WR, Spindler KP (2006) Current concepts review: revision anterior cruciate ligament reconstruction. Am J Sports Med 34:2026–2037. https://doi.org/10.1177/0363546506295026
Pache S, Del Castillo J, Moatshe G, Laprade RF (2020) Anterior cruciate ligament reconstruction failure and revision surgery: current concepts. Journal of ISAKOS 5:351–358. https://doi.org/10.1136/jisakos-2020-000457
Vermeijden HD, Yang XA, van der List JP, DiFelice GS, Rademakers MV, Kerkhoffs GMMJ (2020) Trauma and femoral tunnel position are the most common failure modes of anterior cruciate ligament reconstruction: a systematic review. Knee Surg Sports 28:3666–3675. https://doi.org/10.1007/s00167-020-06160-9
Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD (2016) Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med 44:1861–1876. https://doi.org/10.1177/0363546515621554
Wasserstein D, Khoshbin A, Dwyer T, Chahal J, Gandhi R, Mahomed N, Ogilvie-Harris D (2013) Risk factors for recurrent anterior cruciate ligament reconstruction: a population study in Ontario, Canada, with 5-year follow-up. Am J Sports Med 41:2099–2107. https://doi.org/10.1177/0363546513493580
Morgan JA, Dahm D, Levy B, Stuart MJ (2012) Femoral tunnel malposition in ACL revision reconstruction. J Knee Surg 25:361–368. https://doi.org/10.1055/s-0031-1299662
Ménétrey J, Duthon VB, Laumonier T, Fritschy D (2008) “Biological failure” of the anterior cruciate ligament graft. Knee Surg Sports 16:224–231. https://doi.org/10.1007/s00167-007-0474-x
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Moher D (2021) Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. J Clin Epidemiol 134:103–112. https://doi.org/10.1016/j.jclinepi.2021.02.003
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of observational studies in epidemiology (MOOSE) group. JAMA 283:2008–2012. https://doi.org/10.1001/jama.283.15.2008
Chen JL, Allen CR, Stephens TE, Haas AK, Huston LJ, Wright RW, Feeley BT (2013) Differences in mechanisms of failure, intraoperative findings, and surgical characteristics between single- and multiple-revision ACL reconstructions: a MARS cohort study. Am J Sports Med 41:1571–1578. https://doi.org/10.1177/0363546513487980
Wright RW, Huston LJ, Spindler KP, Dunn WR, Haas AK, Allen CR, Cooper DE, DeBerardino TM, Lantz BB, Mann BJ, Stuart MJ (2010) Descriptive epidemiology of the multicenter ACL revision study (MARS) cohort. Am J Sports Med 38:1979–1986. https://doi.org/10.1177/0363546510378645
Amiel D, Kleiner JB, Roux RD, Harwood FL, Akeson WH (1986) The phenomenon of “ligamentization”: anterior cruciate ligament reconstruction with autogenous patellar tendon. J Orth Res 4:162–172. https://doi.org/10.1002/jor.1100040204
Obremskey WT, Pappas N, Attallah-Wasif E, Tornetta P 3rd, Bhandari M (2005) Level of evidence in orthopaedic journals. The Journal of bone and joint surgery American 87:2632–2638. https://doi.org/10.2106/jbjs.E.00370
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T (2013) Meta-analysis of prevalence. J Epidemiol Commun Health 67:974–978. https://doi.org/10.1136/jech-2013-203104
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558. https://doi.org/10.1002/sim.1186
Ahmed I, Salmon L, Roe J, Pinczewski L (2017) The long-term clinical and radiological outcomes in patients who suffer recurrent injuries to the anterior cruciate ligament after reconstruction. Bone Joint J 99:337–343. https://doi.org/10.1302/0301-620x.99b3.37863
Ahn JH, Lee YS, Ha HC (2008) Comparison of revision surgery with primary anterior cruciate ligament reconstruction and outcome of revision surgery between different graft materials. Am J Sports Med 36:1889–1895. https://doi.org/10.1177/0363546508317124
Anand BS, Feller JA, Richmond AK, Webster KE (2016) Return-to-sport outcomes after revision anterior cruciate ligament reconstruction surgery. Am J Sports Med 44:580–584. https://doi.org/10.1177/0363546515618381
Ao YF, Ma Y, Cui GQ, Yu JK (2007) Factors leading to failure of anterior cruciate ligament reconstruction. Zhonghua wai ke za zhi [Chin J Surg] 45:86–89
Boyle C, Pagoti R, Eng KH, McMahon SE, Nicholas R (2019) Revision ACL reconstruction with autograft: long-term functional outcomes and influencing factors. Eur J Orthop Surg Traumatol 29:157–161. https://doi.org/10.1007/s00590-018-2277-9
Carson EW, Anisko EM, Restrepo C, Panariello RA, O’Brien SJ, Warren RF (2004) Revision anterior cruciate ligament reconstruction: etiology of failures and clinical results. J Knee Surg 17:127–132. https://doi.org/10.1055/s-0030-1248210
Colosimo AJ, Heidt RS Jr, Traub JA, Carlonas RL (2001) Revision anterior cruciate ligament reconstruction with a reharvested ipsilateral patellar tendon. Am J Sports Med 29:746–750. https://doi.org/10.1177/03635465010290061301
Di Benedetto P, Di Benedetto E, Fiocchi A, Beltrame A, Causero A (2016) Causes of failure of anterior cruciate ligament reconstruction and revision surgical strategies. Knee Surg Relat Res 28:319–324. https://doi.org/10.5792/ksrr.16.007
Diamantopoulos AP, Lorbach O, Paessler HH (2008) Anterior cruciate ligament revision reconstruction: results in 107 patients. Am J Sports Med 36:851–860. https://doi.org/10.1177/0363546507312381
Dini F, Tecame A, Ampollini A, Adravanti P (2021) Multiple ACL revision: failure analysis and clinical outcomes. J Knee Surg 34:801–809. https://doi.org/10.1055/s-0039-3400741
Ferretti A, Conteduca F, Monaco E, De Carli A, D’Arrigo C (2007) Revision anterior cruciate ligament reconstruction with doubled semitendinosus and gracilis tendons and lateral extra-articular reconstruction Surgical technique. J Bone Joint Surg Am 89(Suppl 2):196–213. https://doi.org/10.2106/jbjs.G.00310
Frank RM, McGill KC, Cole BJ, Bush-Joseph CA, Bach BR Jr, Verma NN, Slabaugh MA (2012) An institution-specific analysis of ACL reconstruction failure. J Knee Surg 25:143–149. https://doi.org/10.1055/s-0031-1286196
Garofalo R, Djahangiri A, Siegrist O (2006) Revision anterior cruciate ligament reconstruction with quadriceps tendon-patellar bone autograft. Arthrosc J Arthrosc Relat Surg 22:205–214
Inderhaug E, Raknes S, Østvold T, Solheim E, Strand T (2017) Increased revision rate with posterior tibial tunnel placement after using the 70-degree tibial guide in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 25:152–158. https://doi.org/10.1007/s00167-016-4341-5
Jaecker V, Zapf T, Naendrup JH, Kanakamedala AC, Pfeiffer T, Shafizadeh S (2018) Differences between traumatic and non-traumatic causes of ACL revision surgery. Arch Orthop Trauma Surg 138:1265–1272. https://doi.org/10.1007/s00402-018-2954-5
Jiang YF, Wang J, Wang YJ, Liu J, Pei Y, Liu XP, Ao YF, Ma Y (2021) Mid-to-long term clinical outcomes and predictors after anterior cruciate ligament revision. J Peking Univ Health Sci 53:857–864
Johnson DL, Swenson TM, Irrgang JJ, Fu FH, Harner CD (1996) Revision anterior cruciate ligament surgery: experience from Pittsburgh. Clin Orthop Relat Res 325:100–109. https://doi.org/10.1097/00003086-199604000-00011
Lee DW, Kim JG, Cho SI, Kim DH (2019) Clinical outcomes of isolated revision anterior cruciate ligament reconstruction or in combination with anatomic anterolateral ligament reconstruction. Am J Sports Med 47:324–333. https://doi.org/10.1177/0363546518815888
Lupetti E, Goretti C, Colombelli A, Belluati A, Flacco B (2014) When and why do our ACL reconstructions fail? Analysis of the causes and treatment strategies. J Orthop Traumatol 15:S62. https://doi.org/10.1007/s10195-014-0315-x
Ma Y, Ao YF, Yu JK, Dai LH, Shao ZX (2013) Failed anterior cruciate ligament reconstruction: analysis of factors leading to instability after primary surgery. Chin Med J (Engl) 126:280–285
Mahmoud SS, Odak S, Coogan S, McNicholas MJ (2014) A prospective study to assess the outcomes of revision anterior cruciate ligament reconstruction. Int Orthop 38:1489–1494. https://doi.org/10.1007/s00264-014-2324-z
Pascual-Garrido C, Carbo L, Makino A (2014) Revision of anterior cruciate ligament reconstruction with allografts in patients younger than 40 years old: a 2 to 4 year results. Knee Surg Sports Traumat Arthrosc 22:1106–1111. https://doi.org/10.1007/s00167-013-2507-y
Redler A, Iorio R, Monaco E, Puglia F, Wolf MR, Mazza D, Ferretti A (2018) Revision anterior cruciate ligament reconstruction with hamstrings and extra-articular tenodesis: a mid- to long-term clinical and radiological study. Arthroscopy 34:3204–3213. https://doi.org/10.1016/j.arthro.2018.05.045
Reverte-Vinaixa MM, Minguell J, Joshi N, Diaz-Ferreiro EW, Duarri G, Carrera L, Castellet E (2014) Revision anterior cruciate ligament reconstruction using tibial or hamstring tendon allografts. J Orthop Surg (Hong Kong) 22:60–64. https://doi.org/10.1177/230949901402200116
Salmon LJ, Pinczewski LA, Russell VJ, Refshauge K (2006) Revision anterior cruciate ligament reconstruction with hamstring tendon autograft: 5- to 9-year follow-up. Am J Sports Med 34:1604–1614. https://doi.org/10.1177/0363546506288015
Takazawa Y, Ikeda H, Saita Y, Ishijima M, Nagayama M, Kaneko H, Kobayashi Y, Hada S, Sadatsuki R, Kaneko K (2015) Case series: revision anterior cruciate ligament reconstructions using patellar tendon autografts. Knee 22:569–573. https://doi.org/10.1016/j.knee.2015.06.005
Akhtar MA, Bhattacharya R, Keating JF (2016) Generalised ligamentous laxity and revision ACL surgery: is there a relation? Knee 23:1148–1153. https://doi.org/10.1016/j.knee.2015.11.006
Denti M, Lo Vetere D, Bait C, Schonhuber H, Melegati G, Volpi P (2008) Revision anterior cruciate ligament reconstruction - causes of failure, surgical technique, and clinical results. Am J Sports Med 36:1896–1902. https://doi.org/10.1177/0363546508318189
Mayr H, Willkomm D, Stoehr A, Schettle M, Suedkamp N, Bernstein A, Hube R (2012) Revision of anterior cruciate ligament reconstruction with patellar tendon allograft and autograft: 2- and 5-year results. Arch Orthop Trauma Surg 132:867–874. https://doi.org/10.1007/s00402-012-1481-z
Wang DH, Lee KT (2014) Results of revision anterior cruciate ligament reconstruction using a transportal technique: an institutional experience. Ann Acad Med Singapore 43:S181
Vališ P, Sklenský J, Repko M, Rouchal M, Novák J, Otaševič T (2014) Most frequent causes of autologous graft failure in anterior cruciate ligament replacement. Acta Chir Orthop Traumatol Cech 81:371–379
Noyes FR, Barber-Westin SD (2006) Anterior cruciate ligament revision reconstruction - results using a quadriceps tendon-patellar bone autograft. Am J Sports Med 34:553–564. https://doi.org/10.1177/0363546505281812
Uribe JW, Hechtman KS, Zvijac JE, Tjin ATEW (1996) Revision anterior cruciate ligament surgery: experience from Miami. Clin Orthop Relat Res:91–99. https://doi.org/10.1097/00003086-199604000-00010
Wright RW, Huston LJ, Haas AK, Spindler KP et al (2014) Effect of graft choice on the outcome of revision anterior cruciate ligament reconstruction in the Multicenter ACL Revision Study (MARS) Cohort. Am J Sports Med 42:2301–2310. https://doi.org/10.1177/0363546514549005
Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M (2014) Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the danish registry of knee ligament reconstruction. Am J Sports Med 42:278–284. https://doi.org/10.1177/0363546513509220
Trojani C, Sbihi A, Djian P, Potel JF, Hulet C, Jouve F, Bussière C, Ehkirch FP, Burdin G, Dubrana F, Beaufils P, Franceschi JP, Chassaing V, Colombet P, Neyret P (2011) Causes for failure of ACL reconstruction and influence of meniscectomies after revision. Knee Surg Sports Traumatol Arthrosc 19:196–201. https://doi.org/10.1007/s00167-010-1201-6
Vap AR, Persson A, Fenstad AM, Moatshe G, LaPrade RF, Engebretsen L (2019) Re-revision anterior cruciate ligament reconstruction: an evaluation from the norwegian knee ligament registry. Arthroscopy 35:1695–1701. https://doi.org/10.1016/j.arthro.2019.01.027
Capogna BM, Mahure SA, Mollon B, Duenes ML, Rokito AS (2020) Young age, female gender, Caucasian race, and workers’ compensation claim are risk factors for reoperation following arthroscopic ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 28:2213–2223. https://doi.org/10.1007/s00167-019-05798-4
Trojian TH, Collins S (2006) The anterior cruciate ligament tear rate varies by race in professional Women’s basketball. Am J Sports Med 34:895–898. https://doi.org/10.1177/0363546505284384
Navarro RA, Prentice HA, Inacio MCS, Wyatt R, Maletis GB (2019) The association between race/ethnicity and revision following ACL reconstruction in a universally insured cohort. J Bone Joint Surg Am 101:1546–1553. https://doi.org/10.2106/jbjs.18.01408
Shelbourne KD, Gray T, Benner RW (2007) Intercondylar notch width measurement differences between African American and white men and women with intact anterior cruciate ligament knees. Am J Sports Med 35:1304–1307. https://doi.org/10.1177/0363546507300060
Jansson KA, Harilainen A, Sandelin J, Karjalainen PT, Aronen HJ, Tallroth K (1999) Bone tunnel enlargement after anterior cruciate ligament reconstruction with the hamstring autograft and endobutton fixation technique. A clinical, radiographic and magnetic resonance imaging study with 2 years follow-up. Knee Surg Sports Traumatol Arthrosc 7:290–295. https://doi.org/10.1007/s001670050166
Siebold R, Cafaltzis K (2010) Differentiation between intraoperative and postoperative bone tunnel widening and communication in double-bundle anterior cruciate ligament reconstruction: a prospective study. Arthrosc J Arthrosc Relat Surg 26:1066–1073. https://doi.org/10.1016/j.arthro.2009.12.019
Brown CH Jr (2018) Editorial commentary: how to increase hamstring tendon graft size for anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg 34:2641–2646. https://doi.org/10.1016/j.arthro.2018.06.014
Tajima T, Chosa E, Yamamoto K, Yamaguchi N (2012) Arthroscopic anatomical double-bundle anterior cruciate ligament reconstruction for asian patient using a bone-patellar tendon-bone and gracilis tendon composite autograft: a technical note. Sports Med Arthrosc Rehabil Ther Technol 4:9. https://doi.org/10.1186/1758-2555-4-9
Eysturoy NH, Nielsen TG, Lind MC (2019) Anteromedial portal drilling yielded better survivorship of anterior cruciate ligament reconstructions when comparing recent versus early surgeries with this technique. Arthrosc J Arthrosc Relat Surg 35:182–189. https://doi.org/10.1016/j.arthro.2018.08.030
Chen Y, Chua KH, Singh A, Tan JH, Chen X, Tan SH, Tai BC, Lingaraj K (2015) Outcome of single-bundle hamstring anterior cruciate ligament reconstruction using the anteromedial versus the transtibial technique: a systematic review and meta-analysis. Arthrosc J Arthrosc Relat Surg 31:1784–1794. https://doi.org/10.1016/j.arthro.2015.06.001
Yan L, Li JJ, Zhu Y, Liu H, Liu R, Zhao B, Wang B (2021) Interference screws are more likely to perform better than cortical button and cross-pin fixation for hamstring autograft in ACL reconstruction: a Bayesian network meta-analysis. Knee Surg Sports Traumatol Arthrosc 29:1850–1861. https://doi.org/10.1007/s00167-020-06231-x
Gupta R, Sood M, Malhotra A, Masih GD, Kapoor A, Raghav M, Dhillon M (2018) Low re-rupture rate with BPTB autograft and semitendinosus gracilis autograft with preserved insertions in ACL reconstruction surgery in sports persons. Knee Surg Sports Traumatol Arthrosc 26:2381–2388. https://doi.org/10.1007/s00167-017-4790-5
Cristiani R, Sarakatsianos V, Engstrom B, Samuelsson K, Forssblad M, Stalman A (2019) Increased knee laxity with hamstring tendon autograft compared to patellar tendon autograft: a cohort study of 5462 patients with primary anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 27:381–388. https://doi.org/10.1007/s00167-018-5029-9
Yue L, DeFroda SF, Sullivan K, Garcia D, Owens BD (2020) Mechanisms of bone tunnel enlargement following anterior cruciate ligament reconstruction. JBJS reviews 8:e0120. https://doi.org/10.2106/jbjs.Rvw.19.00120
Schüttler KF, Hoeger A, Heyse TJ, Figiel J, Timmesfeld N, Stein T, Ziring E, Efe T (2018) Femoral tunnel widening is associated with tunnel malposition but not with clinical failure after medial patellofemoral ligament reconstruction with a free gracilis tendon graft. Arch Orthop Trauma Surg 138:979–984. https://doi.org/10.1007/s00402-018-2923-z
Iio K, Tsuda E, Tsukada H, Yamamoto Y, Maeda S, Naraoka T, Kimura Y, Ishibashi Y (2017) Characteristics of elongated and ruptured anterior cruciate ligament grafts: an analysis of 21 consecutive revision cases. Asia-Pacific J Sports Med Arthrosc Rehabil Tech 8:1–7. https://doi.org/10.1016/j.asmart.2016.12.001
Funding
This study was supported by the National Natural Science Foundation of China (81802204), China Postdoctoral Science Foundation (2020M671453), Zhejiang University School of Medicine, the First Affiliated Hospital’s Foundation (G2022010-18), Alibaba Cloud and National Health and Medical Research Council (Australia; GNT1120249).
Author information
Authors and Affiliations
Contributions
Xiaoke Li: conceptualization-equal, data curation-equal, formal analysis-equal, writing-original draft-supporting, writing-review and editing-supporting.
Lei Yan: conceptualization-equal, formal analysis-equal, investigation-equal, writing-original draft-lead, writing-review and editing-lead.
Dijun Li: data curation-equal, investigation-equal, methodology-equal, writing-review and editing-supporting.
Zijuan Fan: data curation-equal, investigation-equal, methodology-equal, writing-review and editing-supporting.
Haifeng Liu: data curation-equal, investigation-equal, methodology-equal, writing-review and editing-supporting.
Guishan Wang: data curation-equal, investigation-equal, methodology-equal, writing-review and editing-supporting.
Jingwei Jiu: data curation-equal, investigation-equal, methodology-equal, writing-review and editing-supporting.
Ziquan Yang: data curation-equal, investigation-equal, methodology-equal, writing-review and editing-supporting.
Jiao Jiao Li: data curation-equal, investigation-equal, methodology-equal, writing-review and editing-supporting.
Bin Wang: conceptualization-equal, formal analysis-equal, funding acquisition-lead, supervision-equal, writing-original draft-supporting, writing-review and editing-equal.
Corresponding authors
Ethics declarations
Ethics statement
Not applicable.
Consent to participate
All authors have participated in preparing the manuscript.
Consent for publication
All authors have approved the submission of the manuscript for publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of evidence: IV.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, X., Yan, L., Li, D. et al. Failure modes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. International Orthopaedics (SICOT) 47, 719–734 (2023). https://doi.org/10.1007/s00264-023-05687-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05687-z