Abstract
Purpose
This retrospective study aimed to investigate the clinical outcomes of DDE in adults.
Methods
From September 2010 to March 2020, adult patients with traumatic DDEs admitted to Beijing Chaoyang Hospital and Beijing Jishuitan Hospital were included in this study. Each patient underwent operative or conservative treatment during hospitalization. The clinical and radiological examinations were followed up. The primary outcomes included the Mayo Modified Wrist Score (MMWS), the Mayo Elbow Performance Score (MEPS), the Broberg and Morrey functional index, the Disabilities of the Arm, Shoulder and Hand (DASH) score, and the Visual Analogue Scale (VAS) score that were performed. Post-operative complications and secondary surgery details were also collected.
Results
Of the fourteen patients, clinical and radiographic results were reviewed at a mean of 53.2 months (18 to 110 months) postoperatively. There were 11 men and three women with an average age of 31.5 years (17 to 51 years). At the final follow-up, the average MMWS, MEPS, Broberg and Morrey functional index, and DASH scores were 91.4 points, 93.4 points, 92.6 points, and 10.7 points. The mean VAS at rest and during activities was 0.4 and 1.7 points. Two patients required a secondary procedure due to radial malalignment and elbow contracture, respectively. In addition, two patients were found degeneration.
Conclusions
Within the context of high-energy DDE combined with simultaneous upper limb injuries, our study recommended obtaining the mechanical benefit of the forearm ring with concentric elbow stability. Despite the various and complicated traumatic patterns of DDE, great clinical results could be acquired based on adequate surgical treatments and early rehabilitation training.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Divergent dislocation of the elbow (DDE) is an exceedingly rare elbow dislocation in which the distal humerus is caught between the proximal radius and ulna and then brings about the divergence of the proximal forearm bones [1]. All elbow articulations are involved, including humeroulnar, humeroradial, and proximal radioulnar joints. DDE has been divided into two types: the anteroposterior and the transverse dislocation, most commonly occurring in children.
To our knowledge, the first modern case of traumatic DDE was reported by DeLee in 1981 [1]. Since then, thirty-one cases were identified in reported studies, of which only five clinical literatures investigated this injury in adults [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28]. Most of these studies mentioned that conservative treatment could acquire great clinical outcomes. However, the eventual results of closed reduction of DDE depend on concomitant fractures and the damage degree. So far, the surgical indication of DDE remains an ongoing debate. It is disastrous that emergency surgeons underestimate this trauma pattern on initial evaluation and subsequent treatment in a delayed timing, which can result in elbow dysfunction and other post-operative complications. Moreover, other pathological data, including elbow joint stability and clinical functional scores associated with DDE, remain a relatively unworked area.
Hence, the purpose of this retrospective study was to report the traumatic DDE in adults and to discuss the present management, clinical outcomes, and functional scores.
Methods
Study design and participants
This retrospective cohort study was approved by the Ethics Committee of Beijing Chaoyang Hospital and Beijing Jishuitan Hospital to evaluate the medical records and radiographic outcomes of patients receiving treatments for DDE between September 2010 and March 2020. The Committee waived the requirement for written informed consent because the study was retrospective, did not have any adverse effect on patients’ health, and reported anonymized patient data.
The inclusion criteria consisted of adult patients who had suffered from a DDE. The diagnosis of a DDE was referred to a combination of clinical signs and radiographic evidence: elbow dislocation with separation of proximal radius and ulna in opposite directions. Exclusion criteria consisted of patients with a follow-up of less than 12 months, attendance more than two weeks after the injury, and patients requiring a secondary procedure after failed initial treatment in another hospital as a second-stage or salvage procedure.
Interventions
The details of initial and secondary operative procedures are summarized in Table 1. Each patient initially received a closed reduction by distal traction on the forearm with counter traction and compression of the proximal radius and ulna, which has previously been reported [29]. The clinical outcomes were confirmed radiologically. In order to determine the details of concomitant injuries and better perform subsequent treatments, CT scans were performed in twelve cases after a failed closed reduction. The elbow was reduced and obtained stability with a closed reduction in two patients: Figs. 1 and 2 demonstrate an isolated DDE and a DDE combined with a distal radius fracture.
Patients that combined with unstable elbow fractures required surgical treatment. For the concomitant elbow periarticular fracture, surgeons should double-check the stability of elbow joints during operation. Especially when there was an apparent rupture of the joint capsule with complete tears of the lateral and medial collateral ligaments. The origins of the lateral collateral ligament (LCL) were reattached to the lateral epicondyle with suture anchors (Arthrex, Florida, USA) through the lateral Kocher approach [30]. The medial “over the top” approach was applied to stabilize the type II ulnar coronoid process fracture (according to the Regan and Morrey classification) with a precontoured plate (Accumed, Portland, Oregon) [31, 32]. Surgeons also preferred repairing the anterior oblique ligament of the medial lateral ligament (MCL) and anterior joint capsule with suture anchors (Figs. 3 and 4). The relatively tiny fracture fragments of the radial head and coronoid process were not explicitly addressed. After confirming that the proximal radioulnar joint (PRUJ) was corrected and the instability of the radial head, one humeroradial joint was fixed with a 2.5-mm Kirschner wire (K wire) in 60° flexion of the elbow and the neutral position of the forearm. Of note, cross or parallel K wires fixation of the PRUJ should be avoided in this fresh injury, which seriously limited early rehabilitation (particularly in the extension of the elbow). Furthermore, Fig. 5 demonstrates that one patient was applicated with an additional hinged elbow external fixator (Stryker Corp., Kalamazoo, MI, USA).
A case of a 35-year-old right-hand dominant male sustained a DDE combined with an ulnar coronoid process fracture (a–b). The patient was treated with an external fixator and a repair of the elbow joint ligament. The relatively tiny fracture fragments were not specifically addressed (c–e). Worth mentioning was the full range of motion was obtained at 12 monthly post-operative (f–i)
A 20-year-old male suffering a DDE and ulnar coronoid process fracture. Closed reduction was performed immediately (a–b). However, post-operative radiographs presented the ulnar coronoid process fracture was visibly large and lodged in the elbow joint (c–f). In addition, ORIF of the ulnar coronoid process and a repair of the LCL were also applied (g–h)
Radiographs of a 44-year-old right-hand dominant male exhibiting a DDE and a radial shaft fracture (a–c). Post-operative radiographs of the elbow showed good reduction and fixation with an external fixator and an ORIF of the radial shaft (d–e). The external fixator was removed at 6 weeks post-operative (f–g) and he has full range of motion at 18 monthly follow-up (h–k)
Two patients with open fracture-dislocation required staged operation. Firstly, sufficient irrigation and debridement were performed. The fracture-dislocation was provisionally reduced with K wires and a splint. Several days later, open reduction and internal fixation (ORIF) was performed for combined fractures (humeral/ulnar/radial shaft and the ulnar styloid process) with locking compression plates (LCP) or hook plates (Synthes, Paoli, USA).
In addition, it was worth mentioning that the distal radioulnar joint (DRUJ) was stable after fracture reduction and fixation (Fig. 6).
Post-operative treatment
The post-operative treatment depended on the severity of fracture-dislocations and clinical outcomes. Patients without hinged external fixators or pin-crossings were splinted in 90° of flexion for two to three weeks with the forearm in the neutral position. Active mobilization, including forearm rotation and elbow flexion and extension, was encouraged after two weeks under the guidance of doctors. Range of motion was gradually increased at three weeks postoperatively.
Active and passive elbow mobilization within pain limits started immediately for the patients with hinged external fixators. The fixator was not removed until six weeks post-operatively, and rehabilitation was continued without restriction. The DRUJ and humeroradial K wires were removed in four weeks.
Resistance exercises were performed when bone healing was obtained.
In addition, non-steroid anti-inflammatories (Indomethacin 25 mg orally three times daily) were administered for three weeks to prevent heterotopic ossifications.
Clinical evaluation
There were 14 patients contacted and returned for at least 18 months of follow-up, including clinical outcomes, radiographic evaluation, and measurement of the range of motion using a goniometer. Follow-up evaluation was undertaken by the same surgeon who performed the operation.
The function of the wrist was assessed using the Mayo Modified Wrist Score (MMWS) [33]. The elbow function was assessed using the Mayo Elbow Performance Score (MEPS) and the Broberg and Morrey rating index [34, 35]. The Disabilities of the Arm, Shoulder and Hand (DASH) score was also performed [36]. Valgus and varus activity was tested in maximum extension and in 30° of flexion. The pivot-shift test was performed to evaluate posterolateral rotation, graded as normal, mild, moderate, or severely unstable [37]. Pain at rest and during the activity was assessed using a visual analogue score (VAS, 0 to 10, no pain to severe pain).
The radiographic examination was performed for fracture union, congruency of the humeroulnar and humeroradial joints, and signs of degenerative arthritis. Degeneration was classified according to Broberg and Morrey as grade 0 (normal joint), grade 1 (slight joint space narrowing and minimum osteophyte formation), grade 2 (moderate joint space narrowing and osteophyte formation), or grade 3 (severe degenerative changes with gross destruction of the joint). Fracture union was referred to bridging bone on anteroposterior and lateral radiographs. Heterotopic ossification was graded according to Brooker as grade I, II, III, or IV [38].
Statistical analysis
The software SPSS 24.0 (IBM Corp. Armonk, NY, USA) was used for the statistical analysis of all follow-up data. Continuous variables were summarized as means (ranges).
Results
Twenty-two adult patients were collected in the institutional database to be diagnosed with DDE between September 2010 and 31 March 2020. Of these, eight patients were excluded: four had a follow-up time of less than 12 months and four received a secondary procedure after failed initial treatment in another hospital. Finally, there were fourteen patients available for clinical and radiological review for an average of 53.2 months, with 11 males and two females, ranging from 17 to 51 years (the average age was 31.5 years) (Table 1). These patients’ left and right sides were injured in six and eight cases. The mechanism of injury involved falling from a great height (8 cases), traffic accidents (3 cases), and machine accidents (3 cases).
Of these fourteen patients, one patient was an isolated DDE. Three patients sustained combined ulnar coronoid process fractures, and one of them with a radial head fracture. Four patients underwent simultaneous radial shaft fractures. The remaining six patients presented the bipolar fracture-dislocation of the forearm (DDE + DRUJ subluxation/ dislocation + at least one fracture of the ulnar and radius). According to Gustilo and Anderson classification, there were two patients with open wounds at the forearm classified as type II and type IIIA, respectively [39, 40]. One patient suffered an ipsilateral radial nerve injury and one had multiple injuries with traumatic pneumothorax and rib fractures in the accident.
The mean activity of the elbow was from 133.2° (100 to 140°) of flexion to 8° (0 to 20°) of extension (Table 2). The average range of motion of the wrist was from 78.2° (60 to 90°) of flexion to 74.2° (40 to 90°) of extension. No patients showed elbow or wrist instability. The mean grip strength was 90.1% (81 to 99%), compared with the uninjured side. The mean pronation and supination of the forearm were 81.1° (10 to 90°) and 82.2° (45 to 90°), respectively. Functional scores were performed at the final follow-ups (Table 3). Of these 14 patients, the mean Mayo Modified Wrist Score (MMWS) was 91.4 points (80 to 100) (8 excellent (57%), six good (43%)), and the mean Mayo Elbow Performance Score (MEPS) was 93.4 points (70 to 100) (7 excellent (50%), five good (35.7%), two fair (14.3%)). The mean Broberg and Morrey functional index was 92.6 points (79 to 100) (7 excellent (50%), five good (35.7%), two fair (14.3%)). The mean Disabilities of the Arm, Shoulder and Hand (DASH) score was 10.7 (0 to 36). In addition, minimal pain was reported with a mean Visual Analogue Scale (VAS) score of 0.4 (0 to 1) at rest and 1.7 (0 to 3) during activities.
Eleven patients were found great radiographic outcomes without any sign of degeneration or heterotopic ossification in the elbow region. Two patients, combined with radius/ulna shaft fracture and DRUJ injury, showed grade 1 degeneration (Figs. 7 and 8). Figures 7 and 9 also involve an asymptomatic grade 1 heterotopic ossification.
Post-operative radiographs of the right elbow revealed a DDE and a multiple fracture (a–d). However, this patient sustained an elbow malrotation (arrow and circle), which failed to restore the anatomical radial bow (e–f). Eight weeks later, a secondary operation consisting of radius shortening and release of an elbow contracture was required to restore motion (g–j)
a–b One case suffering a DDE combined with a radial shaft fracture: he received surgical treatment immediately and was found asymptomatic grade 1 heterotopic ossification (c–d). Clinical photos of the elbow 2 years after surgery showed an excellent clinical outcome compared with the opposite side after a regular rehabilitation training (e–j)
Of note, case 10 presented a slight hypoaesthesia of the radial nerve on admission, which was attributed to the fracture displacement and traction of the nerve. Therefore, surgeons performed the ORIF without radial nerve exploration. At three months follow-up, the patient demonstrated that the forearm muscle strength was recovered and the Tinel test presented the dorsoradial paralysis disappeared. Finally, this symptom resolved entirely at six months postinjury.
Two patients received secondary treatments. One case was attributed to elbow malrotation, which failed to restore the anatomical radial bow inhibiting the humeroulnar joint reduction (Fig. 8). The revision surgery was performed at eight weeks after the initial operation, consisting of malalignment correction, re-fixation with a 3.5 mm locking compression plate, and iliac bone autograft for the radial shaft fracture and the elbow reduction. The clinical outcome was satisfactory compared with the opposite side. The other one underwent subsequent surgery for elbow contracture release, with an activity of flexion and extension was 70° and 5° for the elbow. Then, the range of motion improved to 130° and 5° after secondary treatment.
Discussion
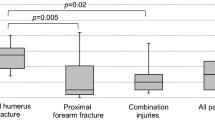
Although studies regarding pediatric cases have been increasingly published, literature reporting DDE in adults remained sparse. In 1854, Warmont first described this trauma in a child [41]. In 1981, DeLee reported the first case of divergent elbow dislocation confirmed by radiographic evidence [1]. We collected the most extensive series of adult patients with clearly defined traumatic DDE and the clinical outcomes were also assessed. In contrast to paediatric cases that DDE is mainly caused by a simple fall, high-energy trauma frequently presents in adults, which results in associated fracture/dislocation of the forearm. Our study divided patients into four types of injury patterns according to the combined fractures of forearms as follows:
Type A isolated DDE (1/14, 7.1%).
Type B DDE + periarticular elbow fractures (radial head fracture, ulnar coronoid fracture, etc.) (3/14, 21.4%).
Type C DDE + radial and/or ulnar shaft fracture (4/14, 28.6%).
Type D bipolar fracture-dislocation of the forearm (DDE + DRUJ subluxation/ dislocation + at least one ulnar and radius fracture) (6/14, 42.9%).
Each type in our study was demonstrated in previous literature [2,3,4,5,6]. These concomitant fracture-dislocations of the forearms further complicated the DDE in adults, which brought a considerable challenge to orthopaedic surgeons.
In a recent study, DDE was associated with periarticular elbow disruptions, including the LCL, MCL, interosseous membrane, and capsule. This injury consisted of anteroposterior and mediolateral (or transverse) dislocations. However, our study found that the anteroposterior and lateral views of the elbow joint showed the radial head was dislocated laterally and the proximal ulna was dislocated in a posteromedial direction, respectively. A nonstandard radiographic analysis always implied a confounding diagnosis of two types of DDE. Hence, our results were consistent with Altuntas et al., which demonstrated that only the posterior DDE existed [17]. With regard to the significance of radial head position and other traumas (forearm and distal radial fractures, interosseous membrane and DRUJ instability, etc.) in initial clinical examination, our study preferred a pre-operative CT scanning for patients with DDE of high-energy injury.
The operative indication for DDE has become into question because of its complex anatomical structure. Previous literature stated that a resultant and axial violence is applied parallel to the longitudinal axis of the forearm and in association with the rupture of the annular ligament and interosseous membrane [2, 12, 13]. Cadaver studies demonstrated that radial head dislocation occurred by pronating violence of the forearm after the MCL rupture existed. This evidence showed that the forearm was in a position of supination and the displaced humerus divorced the radius and ulna. Moreover, recent literature mentioned that annular ligament (AL) reconstruction should be considered due to a posterolateral dislocated radial head [6]. However, our surgeon did not find the AL damage due to the dislocated radial head during surgery.
For paediatric cases, physiologic or pathologic joint laxity related to three articulations separation is highly unusual. Casstevens et al. proposed that a valgus stress and axial loading due to an outstretched forearm with soft-tissue lesions was the primary injury mechanism for a traumatic DDE [3]. Recently, Greene et al. presented a traumatic DDE case receiving a forearm amputation. This grown patient underwent a machine accident caused by auger type, who was observed with generalized swelling of the elbow, severe torsion, ulnar and radial shaft fractures, an LCL tear, and traumatic amputation of the distal aspect of the forearm and the wrist [5]. A case report revealed that a patient with Ehlers-Danlos syndrome (EDS) fell while snowboarding and developed a DDE without a fracture that required an ORIF [6]. Clinical features of this disease included soft-tissue fragility, hyperextension, and joint laxity. However, the exact traumatic mechanism remained unknown, and at least one above-mentioned factor was involved in the present cases.
Closed reduction for DDE in most pediatric cases could obtain a great eventual outcome if the diagnosis was precise after admission [23]. Reduction techniques have been mentioned in published studies [1,2,3, 7, 8, 11, 13]. For patients with a persistent unstable PRUJ/ DRUJ, an additional hinged external fixator or K wire fixation was optional. Considering the difference in the severe nature of the injury between DDE in adults and children, surgeons should pay particular attention to ORIF combined ligamentous reconstructions in high-energy cases, which provide patients with great possibilities of maintaining long-term painless rehabilitation without complications. In our study, the overall function outcome was satisfactory, consistent with the previous works in adults (Table 4).
Until now, it remains an ongoing debate for standard treatment of DDE in adults due to the infrequency and diversity of this damage and the relatively insufficient data available in the previous literature. Nonetheless, according to our experience and the clinical data, the following principles are presented: (i) The elbow dislocation should be reduced immediately. Clinical tests and radiographic evidence are conducted to check the residual elbow instability. (ii) The conservative treatment with closed reduction is an alternative option for the isolated DDE, providing sufficient humeroulnar and PRUJ stability. (iii) DDE combined with elbow periarticular fractures (such as the ulnar coronoid process fracture, radial head/neck fracture) or the ligaments/capsule disruption should be treated with ORIF because of its unstable structure and all three elbow articulations involved, which requires anatomic reduction and stable plate fixation to restore the concentric elbow stability and permits early mobilization. It would be advisable that the forearm fracture acquires anatomic alignment, contributing to DDE reduction. Occasionally, the DDE combined with a stable fracture received a closed reduction and was maintained with a splint (Table 1, no. 11). (iv) The elbow joint stability is checked in a full range of motion. Any residual instability should be treated with additional LCL /MCL repair. (v) We suggest paying particular attention to the DRUJ and the forearm longitudinal stable. Currently, four complex DDE combined with the DRUJ instability are referred to Essex-Lopresti injuries. In this situation, three lockers of the forearm ring are destroyed, causing longitudinal instability of the forearm. Then, the elbow joint, PRUJ and DRUJ stability should be confirmed and further repair to prevent residual instability. (vi) Early post-operative functional training is recommended, and elbow immobilization should not exceed three weeks to avoid stiffness. When residual post-operative instability or the related reconstruction is found to be tenuous, a hinged elbow fixation results in an excellent clinical outcome.
This study has several limitations worth mentioning, including its retrospective design. The relatively small series size limits the reliability of our study. However, our study included the largest number of cases in DDE-related literature. There is no consensus on the treatment principle of DDE, causing a lack of consistent treatment algorithms. Of note, this study does not consist of any case with delayed treatment (more than 2 weeks after injury) due to its more complex pathogenic condition and surgical treatment. In addition, several surgical interventions caused a longitudinal separation of the forearm and poor clinical outcomes. Our institution will report a series of delayed treatments for elbow dislocation in future studies.
Conclusion
Based on providing the anatomic stability of the elbow joints, the treatment effect for DDE with concomitant injuries could be relatively warranted. In DDE associated with periarticular fractures (and/or ligamentous injuries), the closed reduction and subsequent procedures, including ORIF (and/or ligament repair) and early rehabilitation training, are performed instantly. In addition, early rehabilitation training under the guidance of doctors was beneficial for eventual outcomes.
Data availability
The data and material that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
DeLee JC (1981) Transverse divergent dislocation of the elbow in a child. Case report. J Bone Joint Surg Am 63(2):322–323. https://doi.org/10.1007/BF00267846
Kazuki K, Miyamoto T, Ohzono K (2005) A case of traumatic divergent fracture dislocation of the elbow combined with Essex-Lopresti lesion in an adult. J Shoulder Elbow Surg 14(2):224–226. https://doi.org/10.1016/j.jse.2004.06.004
Casstevens EC, Calfee RP, Stern PJ (2012) Traumatic divergent elbow dislocation in an adult with an associated fracture of the distal part of the humeral shaft and an open peri lunate dislocation: a case report. JBJS Case Connect 2(4):e61. https://doi.org/10.2106/JBJS.CC.K.00181
Laratta JL, Yoon RS, Frank MA, Koury K, Donegan DJ, Liporace FA (2014) Divergent elbow dislocation with radial shaft fracture, distal ulnar deformation, and distal radioulnar joint instability: an unclassifiable Monteggia variant. J Orthop Traumatol 15(1):63–67. https://doi.org/10.1007/s10195-013-0239-x
Greene RM, Bader JE, Mauter L, Sears BW, Tirre CJ, Hatzidakis AM (2018) Traumatic divergent elbow dislocation with associated forearm amputation in an adult: a case report. JBJS Case Connect 8(4):e92–e95. https://doi.org/10.2106/JBJS.CC.17.00252
Onode E, Takamatsu K, Kuroda T, Kazuki K, Nakamura H (2021) Divergent dislocation of the elbow in an adult with Ehlers-Danlos syndrome: a case report. JBJS Case Connect 11(3):e21. https://doi.org/10.2106/JBJS.CC.21.00159
Carey RP (1984) Simultaneous dislocation of the elbow and the proximal radio-ulnar joint. J Bone Joint Surg Br 66(2):254–256. https://doi.org/10.1007/BF00269920
Andersen K, Mortensen AC, Gron P (1985) Transverse divergent dislocation of the elbow. A report of two cases. Acta Orthop Scand 56(5):442–443. https://doi.org/10.1097/00003086-200004000-00018
Sovio OM, Tredwell SJ (1986) Divergent dislocation of the elbow in a child. J Pediatr Orthop 6(1):96–97. https://doi.org/10.1097/01241398-198601000-00018
McAuliffe TB, Williams D (1988) Transverse divergent dislocation of the elbow. Injury 19(4):279–280
Holbrook JL, Green NE (1988) Divergent pediatric elbow dislocation. A case report. Clin Orthop Relat Res 234:72–74
Hemmadi SS, Trivedi JM (1991) Divergent dislocation of the elbow in a child (a case report). J Postgrad Med 37(4):221–222. https://doi.org/10.1111/pan.12728
Nakano A, Tanaka S, Hirofuji E, Yasuwaki Y, Yamamoto T, Kubota S, Dan H, Yanase Y (1992) Transverse divergent dislocation of the elbow in a six-year-old boy: case report. J Trauma 32(1):118–119. https://doi.org/10.1097/00005373-199201000-00026
Vicente P, Orduña M (1993) Transverse divergent dislocation of the elbow in a child. A case report. Clin Orthop Relat Res 294:312–313. https://doi.org/10.1097/00003086-199309000-00046
Shankarappa YK (1998) Transverse divergent dislocation of the elbow with ipsilateral distal radius epiphyseal injury in a seven-year-old. Injury 29(10):798–802. https://doi.org/10.1016/s0020-1383(98)00175-2
Zaricznyj B (2000) Transverse divergent dislocation of the elbow. Clin Orthop Relat Res 373:146–152. https://doi.org/10.1097/00003086-200004000-00018
Altuntas AO, Balakumar J, Howells RJ, Graham HK (2005) Posterior divergent dislocation of the elbow in children and adolescents: a report of three cases and review of the literature. J Pediatr Orthop 25(3):317–321. https://doi.org/10.1097/01.bpo.0000153877.20561.8a
Basanagoudar P, Pace A, Ross D (2006) Paediatric transverse divergent dislocation of the elbow. Acta Orthop Belg 72(3):359–361
Nanno M, Sawaizumi T, Ito H (2007) Transverse divergent dislocation of the elbow with ipsilateral distal radius fracture in a child. J Orthop Trauma 21(2):145–149. https://doi.org/10.1097/BOT.0b013e318032c4be
Afshar A (2007) Divergent dislocation of the elbow in an 11-year-old child. Arch Iran Med 10(3):413-6. 07103/AIM.0027
van Wagenberg JM, van Huijstee PJ, Verhofstad MH (2011) Pediatric complex divergent elbow dislocation. J Orthop Trauma 25(1):e5-8. https://doi.org/10.1097/BOT.0b013e3181f8d9a8
Eylon S, Lamdan R, Simanovsky N (2011) Divergent elbow dislocation in the very young child: easily treated if correctly diagnosed. J Orthop Trauma 25(1):e1-4. https://doi.org/10.1097/BOT.0b013e3181db7da7
George HL, Unnikrishnan PN, Bass A, Waseem M, Brownson P (2011) Transverse divergent dislocation of elbow in a child: a case report and review of current literature. Pediatr Emerg Care 27(5):411–413. https://doi.org/10.1097/PEC.0b013e3182187438
Parikh SN, Lykissas MG, Mehlman CT, Sands S, Herrera-Soto J, Panchal A, Crawford AH (2014) Convergent and divergent dislocation of the pediatric elbow: two case reports and comprehensive review of literature. J Pediatr Orthop B 23(2):158–167. https://doi.org/10.1097/01.bpb.0000434242.64440.5a
Kasse AN, Diallo M, Sane JC, Thiam B, Bousso A, Sy MH (2014) Open anterior transverse (divergent) dislocation of the elbow joint: a case report and review of the literature. JBJS Case Connect 4(2 suppl 2):1–7. https://doi.org/10.2106/JBJS.CC.M.00140
Mansuripur PK, Deren ME, Lareau CR, Eberson CP (2015) Divergent elbow dislocation and risk of compartment syndrome. R I Med J 98(5):25–27
Suzuki T, Yoshida H, Matsumura N, Iwamoto T, Ochi K, Sato K (2015) Anterior transverse divergent dislocation of the elbow in a child: a case report. JBJS Case Connect 5(3):e75. https://doi.org/10.2106/JBJS.CC.O.00012
Wu Y, Jiang H, Miao W (2016) A case report of children’s divergent dislocation of the elbow and review of literature. Medicine (Baltimore) 95(44):e4772. https://doi.org/10.1097/MD.0000000000004772
Beaty JH, Rockwood and Wilkins’ fractures in children (2015) J Bone Joint Surg Am 88(10):2313. https://doi.org/10.2106/JBJS.8811.ebo3
Morrey BF (2009) Surgical exposures of the elbow. In: Morrey BF, Sanchez Sotelo J (eds) The elbow and its disorders. Saunders Elsevier p, Philadelphia, pp 115–142
Hotchkiss RN, Kasparyan NG (2000) The medial over the top approach to the elbow. Tech Orthop 15:105–112. https://doi.org/10.1097/00013611-200015020-00003
Regan W, Morrey B (1989) Fractures of the coronoid process of the ulna. J Bone Joint Surg Am 71-A:1348–1354
Cooney WP, Bussey R, Dobyns JH, Linscheid RL (1987) Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res 214:136–147. https://doi.org/10.1007/BF00456877
Morrey BF, An KN, Chao EYS (1993) Functional evaluation of the elbow. In: Morrey BF (ed) The elbow and its disorders, 2nd edn. PA: WB Saunders Company, Philadelphia, pp 95
Broberg MA, Morrey BF (1986) Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am 68-A:669–674. https://doi.org/10.1007/BF02555068
Hudak PL, Amadio PC, Bombardier C (1996) The Upper Extremity Collaborative Group (UECG). Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand). Am J Ind Med 29:602–608. https://doi.org/10.1002/(SICI)1097-0274(199606)29:63.0.CO;2-L
O’Driscoll SW, Bell DF, Morrey BF (1991) Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am 73-A:440–446
Brooker AF, Bowerman JW, Robinson RA, Riley LHJr, (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 55-A:1629–1632. https://doi.org/10.1007/978-1-4471-5451-8_25
Gustilo RB, Anderson JT (1976) Prevention of infection in the treatment of one thousand and twenty-five open fractures of the long bones: retrospective and prospective analysis. J Bone Joint Surg 58A:453–458. https://doi.org/10.1007/978-1-4471-5451-8_138
Gustilo RB, Mendoza RM, Williams DN (1984) Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma Acute Care Surg 24:742–746. https://doi.org/10.1097/00005373-198408000-00009
Warmont A (1854) Luxation simultan´ee du cubitus en dedans et du radius en dehors, compliqu´ee de fracture de I’avant-bnas. Mon Hop J Prog Med Chir Prat 99:961–963
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Maoqi Gong and Hanzhou Wang. The first draft of the manuscript was written by Hanzhou Wang and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The Ethics Committee of the Beijing Chaoyang Hospital and Beijing Jishuitan Hospital has approved this study (2021-ke-441), and informed consent was obtained from all individual participants included in the study.
Consent for publication
All authors approved this manuscript and the submission to this journal.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gong, M., Wang, H., Jiang, X. et al. Traumatic divergent dislocation of the elbow in the adults. International Orthopaedics (SICOT) 47, 847–859 (2023). https://doi.org/10.1007/s00264-022-05679-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05679-5