Abstract
Purpose
The assistance of robot technology is introduced into the operating theatre to improve the precision of a total knee arthroplasty. However, as with all new technology, new technology requires a learning curve to reach adequate proficiency. The primary aim of this study was to identify the learning curve of an imageless robotic system with standardised laxity testing. The secondary aim of this study was to evaluate the accuracy of the intra-operative coronal alignment during the learning curve.
Methods
A prospective study was performed on 30 patients undergoing robot-assisted total knee arthroplasty with an imageless robotic system (Corin, Massachusetts, USA) associated with a dedicated standardised laxity testing device. The learning curve of all surgical steps was assessed with intra-operative video monitoring. As comparison, the total surgical time of the last 30 patients receiving conventional total knee arthroplasty by the same surgeon and with the same implant was retrospectively assessed. Coronal lower limb alignment was evaluated pre- and post-operatively on standing full-leg radiographs.
Results
CUSUM (cumulative summation) analysis has shown inflexion points in multiple steps associated with robot-assisted surgery between one and 16 cases, which indicates the progression from the learning phase to the proficiency phase. The inflexion point for total operative time occurred after nine cases. Robot-assisted total knee surgery required significantly longer operative times than the conventional counterpart, with an average increase of 22 min. Post-operative limb and implant alignment was not influenced by a learning curve.
Conclusion
The introduction of an imageless robotic system with standardised laxity assessment for total knee arthroplasty results in a learning curve of nine cases based on operative time. Compared to conventional surgery, the surgeon is not able to reach time neutrality with the robotic platform. There is no learning curve associated with coronal limb or implant alignment. This study enables orthopaedic surgeons to understand the implementation of this surgical system and its specific workflow into clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the last decades, several surgical innovations have seen daylight in total knee arthroplasty. For example, surgical navigation has been introduced in the nineties to aid the surgeon to result in a more precise surgery compared to the conventional technique [1]. While the early results were promising, computer-assisted total knee arthroplasty failed to gain traction due to the absence of clear superior clinical results [2, 3]. Similarly, patient-specific instruments did not deliver a breakthrough to improved patient outcomes [4]. Currently, robotic systems have been introduced into the surgical workflow to improve the procedure precision even further [5]. Whether this technology can improve long-term clinical outcomes is yet to be defined.
In the advent of these new robotic platforms, the assessment of its learning curve is important, as it gives an idea on how an individual surgeon or hospital should prepare the workflow in the operating theatre for the cases following the introduction of new technology [6]. Initially, there is an expected increase of operative time during the learning phase, followed by a steady decrease during the proficiency phase of the surgeon [5, 7]. The length of the learning curve seems likely to be subject to the individual surgeon and robotic system. Although, to date, there is not enough information available to make assumptions on individual personal characteristics influencing one’s individual learning curve [8, 9].
Currently, several orthopaedic companies have released their own robotic device which can be used during total knee arthroplasty [7,8,9,10,11]. Each system is associated with unique characteristics related to their soft- and hardware, with both benefits and flaws. As such, the different aspects of the robotic systems should be analysed individually. For instance, the learning curve on other imageless systems has only been assessed in few studies, demonstrating a learning curve of six to 11 cases [10,11,12,13]. Currently, the knowledge on the learning curve associated with the OMNIBot platform (Corin, Massachusetts, USA) is lacking.
The aim of this study is therefore to assess the learning curve of robot-assisted total knee arthroplasty with an imageless robotic device capable of standardised laxity testing. A secondary aim of this study is to evaluate the accuracy of the coronal limb and implant alignment during the learning curve with the proposed robotic platform.
Material and methods
As part of a prospective study, 30 patients receiving a gap-balancing robot-assisted total knee arthroplasty were included in this study. All of these patients received the surgery by an arthroplasty surgeon with extensive experience with both image-based and imageless navigation. Prior to the start of the surgery, the surgeon received two hours of training on the specific robotic system. Institutional Review Board approval was obtained prior to the start of the study (B670201837736).
According to the inclusion criteria, all patients with end-stage primary osteoarthritis were included in this study. Exclusion criteria were post-traumatic arthritis, inflammatory arthritis, neurologic disorder limiting knee mobility, history of femur or tibia fracture and history of ligamentous knee injury.
Surgery
The Unity Posterior Stabilized implant (Corin, Massachusetts, USA) was used in this study. During the procedure, the exposition of the knee joint was obtained with a standard medial parapatellar approach. The imageless robotic system used in this study (OMNIBotics, Corin, Massachusetts, USA) requires a tibial-first technique. A Cartesian coordinate system was constructed after rigidly attaching tracking arrays, followed by registration of anatomical landmarks on femur and tibia. Native tibiofemoral kinematics and laxity were collected during full range of motion. A tibial cutting block was positioned while its position is monitored with navigation. A dedicated robotic tensioning device was inserted into the tibiofemoral space to distract the femur and tibia under a known force during full range of motion. Based on these gaps, the position of the femoral component was planned to obtain adequate tension on the soft tissue envelope. A femoral cutting guide was attached to the femur to perform all femoral cuts. After removal of the menisci and preparation of the femoral box, the trial components were inserted. The predicted gaps were validated by assessing the ligament tension with the dedicated robotic tensioning device once more. Once the tibial keel was prepared, all trial components were inserted to assess range of motion and joint stability. Finally, all implants were cemented, and the incision was closed.
Outcomes assessed
Operative times were assessed based on intra-operative videos of the surgeon and the surgical field. The operative time of the following steps was defined:
-
Attachment of the tibial array*
-
Exposure: skin incision until transition to the next phase
-
Attachment of the femoral array*
-
Registration*
-
Native kinematic assessment based on navigation*
-
Tibial guide positioning and tibial resection*
-
Initial gap evaluation*
-
Femoral component planning*
-
Femoral cutting guide position and femoral resection*
-
Gap validation*
-
Trial components — kinematic and laxity assessment
-
Cementing
-
Closure
-
Total surgical time: from attachment of the tibial array to closure of the wound*
The learning curve of all steps involving the robot was visualised with an asterisk. As comparison, the total surgical time, which is from skin incision to surgical closure of the wound, of the last 30 patients receiving conventional total knee arthroplasty by the same surgeon and with the same implant was retrospectively assessed.
Coronal lower limb alignment was evaluated pre- and post-operatively on standing full leg radiographs. The hip-knee-ankle axis (HKA) was defined as the angle between the mechanical axis of the femur and the mechanical axis of the tibia. Femoral coronal alignment was measured as the mechanical lateral distal femoral angle (mLDFA), which is the angle between the mechanical axis of the femur and the line connecting the most distal points on the medial and lateral femoral condyle. Tibial coronal alignment was defined as the mechanical medial proximal tibial angle (mMPTA), which is the angle between the mechanical axis of the tibia and the line connecting the medial to the lateral base of the tibial plateau.
Intra-operatively, the HKA, mLDFA and mMPTA were assessed based on the coordinate system of the imageless system.
Statistical analysis
Categorical data analysis was performed with chi square test. Homogeneity of variances was evaluated with Levene’s test. Normal distribution of continuous variables was tested with Shapiro Wilk test and visually verified with boxplots. Parametric data was analysed using independent t-test in case of unpaired variables and one-way ANOVA in case of multiple variables. Statistical significance was set at 0.05.
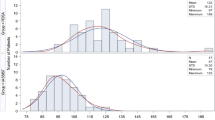
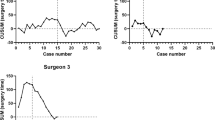
The learning curve of the specific steps and the total surgical time used during robot-assisted TKA were assessed with cumulative summation analysis (CUSUM). A cumulative sum is a running total of the sum of the deviations of all individual sample results from a prespecified target. In case there is a clear inflexion point in the visualised trend, it was defined as the transition from a learning phase to a proficiency phase. The target used in this study was the average time of all robot-assisted procedures. MATLAB 2016a (MathWorks, Massachusetts, USA) was used to perform the statistical analysis.
Results
Pre-operatively, there was no difference between the robot-assisted and conventional total knee arthroplasty cohorts based on age, body mass index, side, gender and HKA (Table 1).
Learning curve
The steps which are different to the robot-assisted total knee surgery have shown mostly no significant differences between the first and last ten cases performed in this series. Both the positioning of the femoral resection guide combined with the femoral resections and the total surgical time have shown significantly lower operative times in the last ten compared to the first 10 cases (p < 0.05). The total operative time was 106.4 min (SD 13.8) for the last 10 cases in the robot-assisted cohort, compared to 84.8 min (SD 15.8) in the conventional TKA cohort (p = 0.001) (Table 2).
CUSUM analysis has shown inflexion points in multiple steps associated with robot-assisted surgery between 1 and 16 cases (Fig. 1; Table 3). Both native kinematic assessment and planning of the femoral component position and its validation did not result in clear inflexion points.
Alignment
During the learning curve, CUSUM analysis did not lead to clear inflexion points based on HKA, femoral or tibial coronal implant alignment. The mean deviation of the post-operative alignment compared to the intra-operative planned alignment was 0.0° (SD 2.5) for HKA, 0.5° of valgus (SD 1.7) for the femoral component and 0.3° of varus (SD 1.3) for the tibial component.
Discussion
This is the first study describing the learning curve of this imageless robotic system with a standardised laxity assessment for total knee arthroplasty. The presented results deliver evidence on a short learning curve when introducing robot-assistance for total knee arthroplasty, encompassing nine cases based on total operative time. One of the strengths in this prospective study is the fact that all time stamps were based on intra-operative videos. As such, any bias on the acquisition of the different time points could be limited, which would not be the case when it would have been a retrospective assessment of a surgeon’s learning curve based on the patient intra-operative files.
Several orthopaedic companies have introduced their own robotic system to aid the surgeon in performing a total knee arthroplasty [7, 8, 10,11,12,13,14,15,16]. However, there are significant differences in the intra-operative steps between all available robotic platforms. More specifically, the presented imageless robot requires a tibial-first technique, possibly altering the routine sequence of a surgeon’s surgical steps. The dedicated robotic tool to perform a standardised laxity assessment introduces new intra-operative steps and intra-operative data compared to conventional total knee surgery [17]. Nonetheless, based on the total operative time, relatively few cases were necessary to transition from the learning phase to the proficiency phase in this study. These findings are comparable to other robot-assisted total knee arthroplasty platforms. First, in a study by Mahure et al., the introduction of the active image-based robot T-Solution One (ThinkSurgical, Fremont, CA, USA) has shown a learning curve of 12–19 cases based on CUSUM analysis [8]. Second, the imageless ROSA (Zimmer-Biomet, Warsaw, Indiana, USA) has presented the need to complete 6–11 cases in order to reach the inflexion point towards the proficiency phase in a study by Vanlommel and colleagues [11]. Third, Savov et al. have demonstrated a learning curve of 11 cases based on total surgical time with the imageless NAVIO (Smith&Nephew, Watford, UK) robot [12]. Most data is available on the MAKO (Stryker, Kalamazoo, Michigan, USA) platform, with evidence of a learning curve of seven to 41 cases required to transition from the learning phase to a more proficient phase in robot-assisted total knee arthroplasty [7, 9, 13, 15]. There is no clinical data available yet on the VELYS system (DePuy Synthes, Raynham, Massachusetts, USA). Regarding the imageless system presented in this study, there has been one published conference abstract by Keggi and Plaskos, describing a learning curve of seven cases [18]. Their results are in accordance with the presented results in this study.
Even though there is a short learning curve with the presented robotic system, the total surgical time of robot-assisted total knee arthroplasty after 30 cases was longer than a conventional cohort by the same surgeon, with an average increase of 26%. With the presented system, the positioning of the femoral resection guide and its associated resections was subject to the longest learning curve. While the total operative time is important for an individual surgeon to maximize operative efficiency, several studies have been able to demonstrate the possibility to achieve time neutrality with a robotic-assisted total knee arthroplasty [9, 13, 14]. However, Savov et al. and Vermue et al. have shown longer operative times in robot-assisted total knee arthroplasty after completing the learning curve compared to the conventional procedure [9, 12].
There was no learning curve associated with achieving the planned coronal implant positions in this study. The average difference between the intra-operative planned position and the post-operative alignment was less than one degree. Although the larger standard deviation for HKA compared to the coronal alignment of the femoral and tibial component should be considered. The fact that there is no learning curve associated with coronal implant position can assure future surgeons in achieving the desired implant position from the first case and onwards. These results are in line with published findings by Mahure et al. on the T-Solution One, by Savov et al. on the NAVIO, by Vanlommel et al. on the ROSA and by Kayani et al., Thiengwittayaporn et al. and Vermue et al. on the MAKO platform [7,8,9, 11,12,13].
The limitation is this study is threefold. First, the surgeon in this study is an experienced knee arthroplasty surgeon. Therefore, the findings presented in this study cannot be generalised to less experienced surgeons. Second, the surgeon assessed in this study has experience with multiple surgical navigation platforms and robotic systems. As such, the learning curve could be underestimated compared to surgeons with less experience with computer- and robot-assistance during total knee arthroplasty. Third, due to the COVID-19 pandemic, several scheduled surgeries had to be postponed. As a result, the surgeries were performed in a longer time frame than initially expected, possibly skewing the amount of cases necessary to complete the learning curve towards higher numbers.
Conclusion
The introduction of an imageless robotic system with standardised laxity assessment for total knee arthroplasty results in a learning curve of nine cases based on operative time. Compared to conventional surgery, the surgeon is not able to reach time neutrality with the robotic platform. There is no learning curve associated with coronal limb or implant alignment. This study enables orthopaedic surgeons to understand the implementation of this surgical system and its specific workflow into clinical practice.
Data availability
In case requested, the data can be deposited to a data repository.
References
Siston RA, Giori NJ, Goodman SB, Delp SL (2007) Surgical navigation for total knee arthroplasty: a perspective. J Biomech 40:728–735
Lee D-Y, Park Y-J, Hwang S-C, Park J-S, Kang D-G (2020) No differences in mid- to long-term outcomes of computer-assisted navigation versus conventional total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 28:3183–3192
de Steiger RN, Liu Y-L, Graves SE (2015) Computer navigation for total knee arthroplasty reduces revision rate for patients less than sixty-five years of age. J Bone Joint Surg Am 97:635–642
Kizaki K, Shanmugaraj A, Yamashita F, Simunovic N, Duong A, Khanna V, Ayeni OR (2019) Total knee arthroplasty using patient-specific instrumentation for osteoarthritis of the knee: a meta-analysis. BMC Musculoskelet Disord 20:561
Vermue H, Lambrechts J, Tampere T, Arnout N, Auvinet E, Victor J (2020) How should we evaluate robotics in the operating theatre? Bone Joint J 102-B:407–413
Mealy A, Sorensen J (2020) Effects of an aging population on hospital costs related to elective hip replacements. Public Health 180:10–16
Kayani B, Konan S, Huq SS, Tahmassebi J, Haddad FS (2019) Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg Sports Traumatol Arthrosc 27:1132–1141
Mahure SA, Teo GM, Kissin YD, Stulberg BN, Kreuzer S, Long WJ (2021) Learning curve for active robotic total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 30(8):2666–2676. https://doi.org/10.1007/s00167-021-06452-8
Vermue H, Luyckx T, Winnock de Grave P, Ryckaert A, Cools A-S, Himpe N, Victor J (2022) Robot-assisted total knee arthroplasty is associated with a learning curve for surgical time but not for component alignment, limb alignment and gap balancing. Knee Surg Sports Traumatol Arthrosc 30:593–602
Bell C, Grau L, Orozco F, Ponzio D, Post Z, Czymek M, Ong A (2021) The successful implementation of the Navio robotic technology required 29 cases. J Robot Surg 16(3):495–499. https://doi.org/10.1007/s11701-021-01254-z
Vanlommel L, Neven E, Anderson M, Bruckers L, Truijen J (2021) The initial learning curve for the ROSA® Knee System can be achieved in 6–11 cases for operative time and has similar 90-day complication rates with improved implant alignment compared to manual instrumentation in total knee arthroplasty. J Exp Orthop 8(1):119. https://doi.org/10.1186/s40634-021-00438-8
Savov P, Tuecking L-R, Windhagen H, Ehmig J, Ettinger M (2021) Imageless robotic handpiece-assisted total knee arthroplasty: a learning curve analysis of surgical time and alignment accuracy. Arch Orthop Trauma Surg 141:2119–2128
Thiengwittayaporn S, Uthaitas P, Senwiruch C, Hongku N, Tunyasuwanakul R (2021) Imageless robotic-assisted total knee arthroplasty accurately restores the radiological alignment with a short learning curve: a randomized controlled trial. Int Orthop 45:2851–2858
Ali M, Phillips D, Kamson A, Nivar I, Dahl R, Hallock R (2022) Learning curve of robotic-assisted total knee arthroplasty for non-fellowship-trained orthopedic surgeons. Arthroplast Today 13:194–198
Marchand KB, Ehiorobo J, Mathew KK, Marchand RC, Mont MA (2022) Learning curve of robotic-assisted total knee arthroplasty for a high-volume surgeon. J Knee Surg 35:409–415
Sodhi N, Khlopas A, Piuzzi NS, Sultan AA, Marchand RC, Malkani AL, Mont MA (2018) The learning curve associated with robotic total knee arthroplasty. J Knee Surg 31:17–21
Shalhoub S, Lawrence JM, Keggi JM, Randall AL, DeClaire JH, Plaskos C (2019) Imageless, robotic-assisted total knee arthroplasty combined with a robotic tensioning system can help predict and achieve accurate postoperative ligament balance. Arthroplast Today 5:334–340
Keggi J, Plaskos C (2017) Learning curve and early patient satisfaction of robotic-assisted total knee arthroplasty. Br Editor Soc Bone Jt Surg 99:59
Funding
One or more of the authors (HV) has received funding from FWO Flanders under the research grant 11F5919N.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Hannes Vermue, Lenka Stroobant, Gilles Thuysbaert and Jan Victor. The first draft of the manuscript was written by Hannes Vermue, and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Ghent University Hospital (B670201837736).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The authors affirm that human research participants provided informed consent for publication of the data used in this manuscript. No patient images or videos are included in this work.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of evidence: III
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vermue, H., Stroobant, L., Thuysbaert, G. et al. The learning curve of imageless robot-assisted total knee arthroplasty with standardised laxity testing requires the completion of nine cases, but does not reach time neutrality compared to conventional surgery. International Orthopaedics (SICOT) 47, 503–509 (2023). https://doi.org/10.1007/s00264-022-05630-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05630-8