Abstract
Purpose
Transoral approach can accomplish ventral decompression directly. However, surgical site infection (SSI) cannot be ignored. This paper aims to review the prevalence of infection and conduct advice for the treatment of SSI in the cervical spine following the transoral approach.
Methods
A retrospective analysis of patients with SSI after transoral atlantoaxial reduction plate (TARP) surgery was performed. SSI was classified into three kinds according to the modified American CDC criteria.
Results
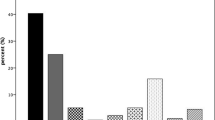
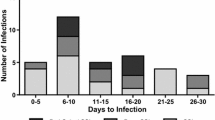
2.9% (17/581) patients who underwent TARP surgery, experienced SSI, of which five had superficial SSI (SI), eight had deep SSI (DI), and four had organ/space SSI (O/SI). The patients with SI underwent intravenous antibiotic treatment and were ultimately cured. Among the remaining 12 patients with DI and O/SI, 11 underwent reoperation for TARP system removal and subsequently one-stage posterior occipitocervical fixation, and one patient experienced infection two months post-operatively and died without receiving treatment. Among patients who underwent revision surgery, three experienced intracranial infection due to intra-operative dural tears, and continuous lumbar cerebrospinal fluid drainage and intrathecal injection of antibiotics were used as effective and appropriate treatments, with outcomes of one recovery and two deaths. All patients with SSI were begun on intravenous antibiotics with conversion to oral antibiotics.
Conclusions
The incidence of SSI was 2.9% (17/581). Adequate peri-operative preparation, early diagnosis, and appropriate treatment of SSI require further research.





Similar content being viewed by others
References
Li T, Yin YH, Qiao GY, Wang HW, Yu XG (2019) Three-dimensional evaluation and classification of the anatomy variations of vertebral artery at the craniovertebral junction in 120 patients of basilar invagination and atlas occipitalization. Oper Neurosurg (Hagerstown Md) 17(6):594–602. https://doi.org/10.1093/ons/opz076
Chen Q, Brahimaj BC, Khanna R, Kerolus MG, Tan LA, David BT, Fessler RG (2020) Posterior atlantoaxial fusion: a comprehensive review of surgical techniques and relevant vascular anomalies. J Spine Surg 6(1):164–180. https://doi.org/10.21037/jss.2020.03.05
Macki M, Hamilton T, Pawloski J, Chang V (2020) Occipital fixation techniques and complications. J Spine Surg 6(1):145–155. https://doi.org/10.21037/jss.2019.12.01
Yin Q, Ai F, Zhang K, Chang Y, Xia H, Wu Z, Quan R, Mai X, Liu J (2005) Irreducible anterior atlantoaxial dislocation: one-stage treatment with a transoral atlantoaxial reduction plate fixation and fusion Report of 5 cases and review of the literature. Spine 30(13):E375–E381. https://doi.org/10.1097/01.brs.0000168374.84757.d5
Macki M, Basheer A, Lee I, Kather R, Rubinfeld I, Abdulhak MM (2018) Surgical site infection after transoral versus posterior approach for atlantoaxial fusion: a matched-cohort study. J Neurosurg Spine 28(1):33–39. https://doi.org/10.3171/2017.5.SPINE161064
Amelot A, Terrier LM, Lot G (2018) Craniovertebral junction transoral approach: predictive factors of complications. World Neurosurg 110:568–574. https://doi.org/10.1016/j.wneu.2017.09.135
Tu Q, Chen H, Li Z, Chen Y, Xu A, Zhu C, Huang X, Ma X, Wang J, Zhang K, Yin Q, Xu J, Xia H (2021) Anterior reduction and C1-ring osteosynthesis with Jefferson-fracture reduction plate (JeRP) via transoral approach for unstable atlas fractures. BMC Musculoskelet Disord 22(1):745. https://doi.org/10.1186/s12891-021-04628-4
Steinberger J, Skovrlj B, Lee NJ, Kothari P, Leven DM, Guzman JZ, Shin J, Shrivastava R, Caridi JM, Cho SK (2016) Surgical morbidity and mortality associated with transoral approach to the cervical spine. Spine 41(9):E535–E540. https://doi.org/10.1097/BRS.0000000000001320
Wei G, Wang Z, Ai F, Yin Q, Wu Z, Ma XY, Xu J, Shi C, Xia H (2016) Treatment of basilar invagination with Klippel-Feil syndrome: atlantoaxial joint distraction and fixation with transoral atlantoaxial reduction plate. Neurosurg 78(4):492–498. https://doi.org/10.1227/NEU.0000000000001094
Zhu C, Wang J, Wu Z, Ma X, Ai F, Xia H (2019) Management of pediatric patients with irreducible atlantoaxial dislocation: transoral anterior release, reduction, and fixation [published online ahead of print, 2019 Jun 14]. J Neurosurg Pediatr. 2019;1–7. https://doi.org/10.3171/2019.4.PEDS1928
Yin QS, Li XS, Bai ZH, Mai XH, Xia H, Wu ZH, Ma XY, Ai FZ, Wang JH, Zhang K (2016) An 11-year review of the TARP procedure in the treatment of atlantoaxial dislocation. Spine 41(19):E1151–E1158. https://doi.org/10.1097/BRS.0000000000001593
Menezes AH (2008) Surgical approaches: postoperative care and complications “transoral-transpalatopharyngeal approach to the craniocervical junction.” Child’s Nerv Sys ChNS: Official J Int Society Pediatr Neurosurg 24(10):1187–1193. https://doi.org/10.1007/s00381-008-0599-3
Karhade AV, Vasudeva VS, Dasenbrock HH, Lu Y, Gormley WB, Groff MW, Chi JH, Smith TR (2016) Thirty-day readmission and reoperation after surgery for spinal tumors: a National Surgical Quality Improvement Program analysis. Neurosurg Focus 41(2):E5. https://doi.org/10.3171/2016.5.FOCUS16168
Fei Q, Li J, Lin J, Li D, Wang B, Meng H, Wang Q, Su N, Yang Y (2016) Risk factors for surgical site infection after spinal surgery: a meta-analysis. World Neurosurg 95:507–515. https://doi.org/10.1016/j.wneu.2015.05.059
Funding
This work was supported by ① Military Medical Science and Technology Youth Cultivation Program Incubation Project (NO.19QNP040, Q T); ② the Science and Technology Planning Project of Guangzhou City (NO.201904010349, Q T); ③ PhD projects of Third Military Medical University (NO.JSKT201904, Q T); ④ Army Logistics Research Project of PLA (CLB20J033, Q T); and ⑤ the National Natural Science Foundation of China (81972080, H X). These grants had no role in the design or execution of this study or the reporting of results.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by HC, CZ, and HY. The first draft of the manuscript was written by HC and QT. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval
This is an observational study. The General Hospital of Southern Theatre Command Research Ethics Committee has confirmed that no ethical approval is required.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, H., Zhu, C., Yi, H. et al. Incidence and management of surgical site infection in the cervical spine following a transoral approach. International Orthopaedics (SICOT) 46, 2329–2337 (2022). https://doi.org/10.1007/s00264-022-05492-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05492-0