Abstract
Purpose
We aimed to improve OR efficiency using machine learning (ML) to find relevant metrics influencing surgery time success and team performance on efficiency to create a model which incorporated team, patient, and surgery-related factors.
Methods
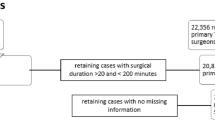
From 2012 to 2020, five surgeons, 44 nurses, and 152 anesthesiologists participated in 1199 four joint days (4796 cases): 1461 THA, 1496 TKA, 652 HR, 242 UKA, and 945 others. Patients were 2461f:2335 m; age, 64.1; BMI, 29.93; and ASA, 2.45. Surgical Success was defined as completing four joints within an eight hour shift using one OR. Time data was recorded prospectively using Surgical Information Management Systems. Hospital records provided team, patient demographics, adverse events, and anesthetic. Data mining identified patterns and relationships in higher dimensions. Predictive analytics used ML ranking algorithm to identify important metrics and created decision tree models for benchmarks and success probability.
Results
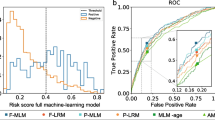
Five variables predicted success: anaesthesia preparation time, surgical preparation time, time of procedure, anesthesia finish time, and type of joint replacement. The model determined success rate with accuracy of 72% and AUC = 0.72. Probability of success based on mean performance was 77–89% (mean-median) if APT 14–15 minutes, PT 68–70 minutes, AFT four to five minutes, and turnover 25–27 minutes. With the above benchmarks maintained, success rate was 59% if surgeon exceeded 71.5-minutes PT or 89% if 64-minutes procedure time or 66% when anesthesiologist spent 17–19.5 minutes on APT.
Conclusion
AI-ML predicted OR success without increasing resources. Benchmarks track OR performance, demonstrate effects of strategic changes, guide decisions, and provide teamwork improvement opportunities.






Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, Dr. Paul Beaulé, upon reasonable request.
References
Fairley M, Scheinker D, Brandeau ML (2019) Improving the efficiency of the operating room environment with an optimization and machine learning model. Health Care Manag Sci 22:756–767. https://doi.org/10.1007/s10729-018-9457-3
Canadian Institute for Health Information. (2020) Hip and knee replacements in Canada: CJRR Quick Stats, 2018–2019. Ottawa, ON
Cram P, Landon BE, Matelski J et al (2018) Hip and knee arthroplasty utilization and outcomes in the United States and Canada: an analysis of New York and Ontario administrative data. Arthritis Rheumatol (Hoboken, NJ) 70:547. https://doi.org/10.1002/ART.40407
FJ W, DS G, NV G, et al (2020) Safety of a “swing room” surgery model at a high-volume hip and knee arthroplasty centre. Bone Joint J 102-B:112–115. https://doi.org/10.1302/0301-620X.102B7.BJJ-2019-1536.R1
Beaulé PE, Frombach AA, Ryu J-J (2015) Working toward benchmarks in orthopedic OR efficiency for joint replacement surgery in an academic centre. Can J Surg 58:408. https://doi.org/10.1503/CJS.001215
Gold R, Al Zoubi F, Brillinger J, et al Use of multidisciplinary positive deviance seminars to improve efficiency in a high-volume arthroplasty practice: a pilot study. Can J Surg
SD B, MH T, RD U (2018) The Association of Anesthesia Clinical Directors (AACD) glossary of times used for scheduling and monitoring of diagnostic and therapeutic procedures. J Med Syst 42. https://doi.org/10.1007/S10916-018-1022-6
Ying X (2019) An overview of overfitting and its solutions. J Phys Conf Ser 1168:022022. https://doi.org/10.1088/1742-6596/1168/2/022022
Shearer C (2000) The CRISP-DM model: the new blueprint for data mining. J data Warehous 5:13–22
Kursa MB, Jankowski A, Rudnicki WR (2010) Boruta - a system for feature selection. Fundam Informaticae 101:271–285. https://doi.org/10.3233/FI-2010-288
Berrar D (2018) Cross-validation. Encycl Bioinforma Comput Biol ABC Bioinforma 1–3:542–545. https://doi.org/10.1016/B978-0-12-809633-8.20349-X
High R Front cover the era of cognitive systems: an inside look at IBM Watson and how it works
G A, W G, R M et al (2016) Hybrid computing using a neural network with dynamic external memory. Nature 538:471–476. https://doi.org/10.1038/NATURE20101
Raghupathi W, Raghupathi V (2014) Big data analytics in healthcare: promise and potential. Heal Inf Sci Syst 2https://doi.org/10.1186/2047-2501-2-3
GW S, RS M, R H (2013) CancerLinQ and the future of cancer care. Am Soc Clin Oncol Educ book Am Soc Clin Oncol Annu Meet 430–434. https://doi.org/10.14694/EDBOOK_AM.2013.33.430
Bellini V, Guzzon M, Bigliardi B, et al (2020) Artificial intelligence: a new tool in operating room management. Role of machine learning models in operating room optimization. J Med Syst 44 https://doi.org/10.1007/S10916-019-1512-1
Luo L, Zhang F, Yao Y, et al (2018) Machine learning for identification of surgeries with high risks of cancellation 26 141–155. https://doi.org/10.1177/1460458218813602
Shahabikargar Z, Khanna S, Sattar A, Lind J (2017) Improved prediction of procedure duration for elective surgery. Stud Health Technol Inform 239:133–138. https://doi.org/10.3233/978-1-61499-783-2-133
Zhao B, Waterman RS, Urman RD, Gabriel RA (2019) A machine learning approach to predicting case duration for robot-assisted surgery. J Med Syst 43:
Maheshwari K, You J, Cummings KC et al (2017) Attempted development of a tool to predict anesthesia preparation time from patient-related and procedure-related characteristics. Anesth Analg 125:580–592. https://doi.org/10.1213/ANE.0000000000002018
Dp S, Ar S, Jh M, LG V, (2000) Surgeon and type of anesthesia predict variability in surgical procedure times. Anesthesiology 92:1454–1466. https://doi.org/10.1097/00000542-200005000-00036
Petis S, Howard J, Lanting B, et al In-hospital cost analysis of total hip arthroplasty: does surgical approach matter? Elsevier
Wu HL, Chang WK, Hu KH, et al (2015) A quantile regression approach to estimating the distribution of anesthetic procedure time during induction. PLoS One 10. https://doi.org/10.1371/journal.pone.0134838
Jung JJ, Jüni P, Lebovic G, Grantcharov T (2020) First-year analysis of the operating room black box study. Ann Surg 271:122–127. https://doi.org/10.1097/SLA.0000000000002863
Mascagni P, Padoy N (2021) OR black box and surgical control tower: recording and streaming data and analytics to improve surgical care. J Visc Surg 158:S18–S25. https://doi.org/10.1016/J.JVISCSURG.2021.01.004
Funding
This work was supported by the Ontario Ministry of Health.
Author information
Authors and Affiliations
Contributions
Farid Al Zoubi: Methodology, Formal analysis, Investigation, Software, Validation, Visualization, Writing–original draft, Writing–review and editing
Richard Gold: Data curation, Investigation, Validation, Visualization, Writing–original draft, Writing–review and editing
Stéphane PoitrasMethodology, Resources, Writing–original draft, Writing–review and editing
Cheryl Kreviazuk: Data curation, Investigation, Writing–review and editing
Julia Brillinger: Data curation, Investigation, Writing–review and editing
Pascal FallavollitaConceptualization, Methodology, Project administration, Resources, Software, Writing–original draft, Writing–review and editing
Paul Beaulé: Conceptualization, Funding acquisition, Project administration, Resources, Supervision, Writing–original draft, Writing–review and editing
Ethics declarations
Ethics approval
This project was reviewed and deemed as exempt from research by the Ottawa Health Science Research Ethics Board.
Consent to participate
Not applicable
Consent to publish
Not applicable
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Location: The work was performed at The Ottawa Hospital and The University of Ottawa. All authors have read and agree with the contents of this manuscript.
Rights and permissions
About this article
Cite this article
Al Zoubi, F., Gold, R., Poitras, S. et al. Artificial intelligence-driven prescriptive model to optimize team efficiency in a high-volume primary arthroplasty practice. International Orthopaedics (SICOT) 47, 343–350 (2023). https://doi.org/10.1007/s00264-022-05475-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05475-1