Abstract
Purpose
Severe acetabular bone defect is challenging in revision hip arthroplasty. In the present study, we aimed to present new treatment options with the 3D printing technique and analyze the clinical and radiographic outcomes of 3D-printed titanium implants for the treatment of severe acetabular bone defects in revision hip arthroplasty.
Methods
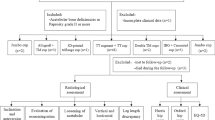
A total of 35 patients with Paprosky type 3 bone defect and pelvic discontinuity (PD), who underwent hip revisions using 3D-printed titanium implants between 2016 and 2019 at our institution, were retrospectively reviewed. Patient-specific 3D-printed titanium augments and shells (strategy A) were used in 22 type 3A and two type 3B patients. Custom 3D-printed flanged components (strategy B) were used in 11 type 3B patients, including five PD. The clinical outcomes were evaluated with the Harris hip score (HHS). In addition, radiographic results were analyzed by the hip centre of rotation (V-COR and H-COR), implant failure, and survivorship.
Results
The mean follow-up was 41.5 months (range, 16–62). The HHS was improved from 47.8 ± 8.2 pre-operatively to 78.1 ± 10.1 at one year follow-up and 86.4 ± 5.1 at the last follow-up (p < 0.01). Post-operative V-COR and H-COR of the operated side were 20.8 ± 2.0 mm and 30.2 ± 1.6 mm compared with 51.4 ± 4.1 mm and 33.9 ± 9.0 mm pre-operatively (p < 0.01). The complications included one dislocation and one partial palsy of the sciatic nerve. At the latest follow-up, no radiological component loosening or screw breakage was present.
Conclusions
3D-printed titanium implants showed satisfactory short- and mid-term clinical and radiographic outcomes. It was an effective therapeutic regimen with a low rate of complications, providing a patient-specific and reliable strategy for the severe acetabular bone defect in revision hip arthroplasty.



Similar content being viewed by others
References
Sloan M, Premkumar A, Sheth NP (2018) Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am 100:1455–1460. https://doi.org/10.2106/jbjs.17.01617
Schwartz AM, Farley KX, Guild GN, Bradbury TL Jr (2020) Projections and epidemiology of revision hip and knee arthroplasty in the United States to 2030. J Arthroplasty 35:S79-s85. https://doi.org/10.1016/j.arth.2020.02.030
Telleria JJ, Gee AO (2013) Classifications in brief: Paprosky classification of acetabular bone loss. Clin Orthop Relat Res 471:3725–3730. https://doi.org/10.1007/s11999-013-3264-4
Fryhofer GW, Ramesh S, Sheth NP (2020) Acetabular reconstruction in revision total hip arthroplasty. J Clin Orthop Trauma 11:22–28. https://doi.org/10.1016/j.jcot.2019.11.004
Löchel J, Janz V, Hipfl C, Perka C, Wassilew GI (2019) Reconstruction of acetabular defects with porous tantalum shells and augments in revision total hip arthroplasty at ten-year follow-up. Bone Joint J 101-b:311–316. https://doi.org/10.1302/0301-620x.101b3.Bjj-2018-0959.R1
Gustke KA, Levering MF, Miranda MA (2014) Use of jumbo cups for revision of acetabulae with large bony defects. J Arthroplasty 29:199–203. https://doi.org/10.1016/j.arth.2012.11.010
Hosny HAH, El-Bakoury A, Fekry H, Keenan J (2018) Mid-term results of graft augmentation prosthesis II cage and impacted allograft bone in revision hip arthroplasty. J Arthroplasty 33:1487–1493. https://doi.org/10.1016/j.arth.2017.11.060
Kosashvili Y, Backstein D, Safir O, Lakstein D, Gross AE (2009) Acetabular revision using an anti-protrusion (ilio-ischial) cage and trabecular metal acetabular component for severe acetabular bone loss associated with pelvic discontinuity. J Bone Joint Surg Br 91:870–876. https://doi.org/10.1302/0301-620x.91b7.22181
Baauw M, van Hooff ML, Spruit M (2016) Current construct options for revision of large acetabular defects: a systematic review. JBJS reviews 4. https://doi.org/10.2106/jbjs.Rvw.15.00119
Chang CY, Wu CT, Numan H, Kuo FC, Wang JW, Lee MS (2021) Survival analysis of allografting and antiprotrusio cage in treating massive acetabular bone defects. J Arthroplasty 36:682–687. https://doi.org/10.1016/j.arth.2020.08.050
Hipfl C, Janz V, Löchel J, Perka C, Wassilew GI (2018) Cup-cage reconstruction for severe acetabular bone loss and pelvic discontinuity: mid-term results of a consecutive series of 35 cases. Bone Joint J 100-b:1442–1448. https://doi.org/10.1302/0301-620x.100b11.Bjj-2018-0481.R1
Burastero G, Cavagnaro L, Chiarlone F, Zanirato A, Mosconi L, Felli L, de Lorenzo FDR (2020) Clinical study of outcomes after revision surgery using porous titanium custom-made implants for severe acetabular septic bone defects. Int Orthop 44:1957–1964. https://doi.org/10.1007/s00264-020-04623-9
Chiarlone F, Zanirato A, Cavagnaro L, Alessio-Mazzola M, Felli L, Burastero G (2020) Acetabular custom-made implants for severe acetabular bone defect in revision total hip arthroplasty: a systematic review of the literature. Arch Orthop Trauma Surg 140:415–424. https://doi.org/10.1007/s00402-020-03334-5
Tamayo JA, Riascos M, Vargas CA, Baena LM (2021) Additive manufacturing of Ti6Al4V alloy via electron beam melting for the development of implants for the biomedical industry. Heliyon 7:e06892. https://doi.org/10.1016/j.heliyon.2021.e06892
Paprosky WG, Sporer SS, Murphy BP (2007) Addressing severe bone deficiency: what a cage will not do. J Arthroplasty 22:111–115. https://doi.org/10.1016/j.arth.2007.01.018
Petrie J, Sassoon A, Haidukewych GJ (2013) Pelvic discontinuity: current solutions. Bone Joint J 95-b:109–113. https://doi.org/10.1302/0301-620x.95b11.32764
Tserovski S, Georgieva S, Simeonov R, Bigdeli A, Röttinger H, Kinov P (2019) Advantages and disadvantages of 3D printing for pre-operative planning of revision hip surgery. J Surg Case Rep 2019:rjz214. https://doi.org/10.1093/jscr/rjz214
Hughes AJ, DeBuitleir C, Soden P, O’Donnchadha B, Tansey A, Abdulkarim A, McMahon C, Hurson CJ (2017) 3D printing aids acetabular reconstruction in complex revision hip arthroplasty. Adv Orthop 2017:8925050. https://doi.org/10.1155/2017/8925050
Berasi CCT, Berend KR, Adams JB, Ruh EL, Lombardi AV Jr (2015) Are custom triflange acetabular components effective for reconstruction of catastrophic bone loss? Clin Orthop Relat Res 473:528–535. https://doi.org/10.1007/s11999-014-3969-z
Weber M, Witzmann L, Wieding J, Grifka J, Renkawitz T, Craiovan B (2019) Customized implants for acetabular Paprosky III defects may be positioned with high accuracy in revision hip arthroplasty. Int Orthop 43:2235–2243. https://doi.org/10.1007/s00264-018-4193-3
Durand-Hill M, Henckel J, Di Laura A, Hart AJ (2020) Can custom 3D printed implants successfully reconstruct massive acetabular defects? A 3D-CT assessment. J Orthop Res 38:2640–2648. https://doi.org/10.1002/jor.24752
Nwankwo CD, Ries MD (2014) Do jumbo cups cause hip center elevation in revision THA? A radiographic evaluation. Clin Orthop Relat Res 472:2793–2798. https://doi.org/10.1007/s11999-014-3632-8
Nwankwo C, Dong NN, Heffernan CD, Ries MD (2014) Do jumbo cups cause hip center elevation in revision THA? A computer simulation. Clin Orthop Relat Res 472:572–576. https://doi.org/10.1007/s11999-013-3169-2
Marongiu G, Podda D, Mastio M, Capone A (2019) Long-term results of isolated acetabular revisions with reinforcement rings: a 10- to 15-year follow-up. Hip Int 29:385–392. https://doi.org/10.1177/1120700018802750
Amenabar T, Rahman WA, Hetaimish BM, Kuzyk PR, Safir OA, Gross AE (2016) Promising mid-term results with a cup-cage construct for large acetabular defects and pelvic discontinuity. Clin Orthop Relat Res 474:408–414. https://doi.org/10.1007/s11999-015-4210-4
Taunton MJ, Fehring TK, Edwards P, Bernasek T, Holt GE, Christie MJ (2012) Pelvic discontinuity treated with custom triflange component: a reliable option. Clin Orthop Relat Res 470:428–434. https://doi.org/10.1007/s11999-011-2126-1
Goto M, Matsumine A, Yamaguchi S, Takahashi H, Akeda K, Nakamura T, Asanuma K, Matsushita T, Kokubo T, Sudo A (2021) Osteoconductivity of bioactive Ti-6Al-4V implants with lattice-shaped interconnected large pores fabricated by electron beam melting. J Biomater Appl 35:1153–1167. https://doi.org/10.1177/0885328220968218
Huang Y, Zhou YX, Tian H, Wang JW, Liu WG, Li H (2021) Minimum 7-year Follow-up of a porous coated trabecular titanium cup manufactured with electron beam melting technique in primary total hip arthroplasty. Orthop Surg 13:817–824. https://doi.org/10.1111/os.12846
De Martino I, Strigelli V, Cacciola G, Gu A, Bostrom MP, Sculco PK (2019) Survivorship and clinical outcomes of custom triflange acetabular components in revision total hip arthroplasty: a systematic review. J Arthroplasty 34:2511–2518. https://doi.org/10.1016/j.arth.2019.05.032
Berend ME, Berend KR, Lombardi AV, Cates H, Faris P (2018) The patient-specific triflange acetabular implant for revision total hip arthroplasty in patients with severe acetabular defects: planning, implantation, and results. Bone Joint J 100-b:50–54. https://doi.org/10.1302/0301-620x.100b1.Bjj-2017-0362.R1
Acknowledgements
This work was supported by the Youth Talents Science and Technology Project of Changzhou Health Commission (QN201919).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval
The study was approved by the internal review board and ethical committee of the Third Affiliated Hospital of Soochow University.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fang, S., Wang, Y., Xu, P. et al. Three-dimensional-printed titanium implants for severe acetabular bone defects in revision hip arthroplasty: short- and mid-term results. International Orthopaedics (SICOT) 46, 1289–1297 (2022). https://doi.org/10.1007/s00264-022-05390-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05390-5