Abstract
Purpose
This study was conducted to assess a stepwise surgical procedure applied to treat a continuous series of patients with aseptic atrophic nonunion of long bones.
Methods
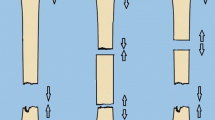
A retrospective review was performed of the medical files of patients treated by the senior author between January 2014 and January 2021 for aseptic atrophic nonunion of long bones using a standard stepwise surgical procedure consisting of four successive surgical steps: bridge locked plating, aggressive osteoperiosteal decortication, copious autologous iliac bone grafting, and tight closure without drainage. Patients were clinically and radiographically evaluated until bone healing, then at final follow-up for the purpose of the study. The primary objective of the study was to assess completion of bone healing; secondary objectives were the time required reaching bone union, the occurrence of complications at the iliac bone graft donor site, and the achievement of bone consolidation after a second attempt of treatment when indicated following failure of the index procedure.
Results
There were a total of 55 patients. One patient died from myocardial infarction before reaching bone healing and another one lost from early follow-up. There were remaining 53 patients with 37 years of mean age. The affected bone was the clavicle in five patients, humerus in 14, ulna in four, radius in one, femur in 13, and tibia in 16. The mean follow-up period was 3.4 years. A total of 52 patients (98.1%) achieved bone healing at a mean of 14.8 weeks from the index procedure. The only patient who did not reach bone healing after the index procedure was successfully revised using decortication-bone graft and new fixation with intra-medullary femoral nailing. Four patients (7.5%) developed local complications at the site of iliac bone harvesting.
Conclusion
Our stepwise surgical procedure was very effective treating aseptic atrophic nonunion of long bones. However, as this study is a retrospective review of a limited series of one surgeon’s experience, prospective comparative studies with large number of patients are suitable to define the advantages and indications of the procedure herein described.





Similar content being viewed by others
Availability of data and materials
The manuscript has no associated data.
References
Piriou P, Martin J-N, Garreau de Loubresse C, Judet T (2005) Traitement des pseudarthroses de jambe après enclouage centromédullaire: intérêt de la décortication ostéopériostée avec ostéosynthèse par plaque médiale. Rev Chir Orthop 91:222–231. https://doi.org/10.1016/S0035-1040(05)84308-9
Judet R, Judet J, Orlandini J, Patel A (1967) La décortication ostéo-musculaire. Rev Chir Orthop 53:43–63
Judet PR, Patel A (1972) Muscle pedicle bone grafting of long bones by osteoperiosteal decortication. Clin Orthop Relat Res 87:74–80
Judet T, Richard L, Arnault O, De Thomasson E, Boury G (1992) Traitement des pseudarthroses du tibia par décortication ostéopériostée de Robert Judet. Acta Orthop Belg 58(suppl 1):182–186
Marino JT, Ziran BH (2010) Use of solid and cancellous autologous bone graft for fractures and nonunions. Orthop Clin N Am 41:15–26. https://doi.org/10.1016/j.ocl.2009.08.003
Heppenstall RB (1980) Fracture Treatment and Healing. WB Saunders, Philadelphia, p 1980
La C, Morshed S, Bhandari M, Miclau T (2008) Variability in the assessment of fracture healing in orthopaedic trauma studies. J Bone Joint Surg (Am) 90–A:1862–1868. https://doi.org/10.2106/JBJS.G.01580
Chamseddine AH, Abdallah A, Zein H, Taha A (2017) Transfracture medial transposition of the radial nerve associated with plate fixation of the humerus. Int Orthop 41:1463–1470. https://doi.org/10.1007/s00264-016-3397-7
Chamseddine AH, Zein HK, Alasiry AA, Mansour NA, Bazzal AM (2013) Trans-fracture transposition of the radial nerve during the open approach of humeral shaft fractures. Eur J Orthop Surg Traumatol 23:725–730. https://doi.org/10.1007/s00590-012-1065-1
Perumal V, Roberts CS (2007) Factors contributing to non-union of fractures. Curr Orthop 21:258–261. https://doi.org/10.1016/j.cuor.2007.06.004
Wiss D, Stetson W (1996) Tibial nonunion: treatment alternatives. J Am Acad Orthop Surg 4:249–257. https://doi.org/10.5435/00124635-199609000-00003
Santolini E, West RM, Giannoudis PV (2020) Leeds-Genoa Non-Union Index: a clinical tool for assessing the need for early intervention after long bone fracture fixation. Int Orthop 44:161–172. https://doi.org/10.1007/s00264-019-04376-0
Weber B (1976) Cech O (1976) Pseudarthrosis, pathology, biomechanics, therapy, results. Hans Huber, Bern
Giannoudis PV, Einhorn TA, Marsh D (2007) Fracture healing: the diamond concept. Injury 38(Suppl 4):S3–S6. https://doi.org/10.1016/s0020-1383(08)70003-2
Andrzejowski P, Giannoudis PV (2019) The “diamond concept” for long bone non-union management. J Orthop Traumatol 20:21. https://doi.org/10.1186/s10195-019-0528-0
Masquelet AC, Bégué T (2010) The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am 41:27–37. https://doi.org/10.1016/j.ocl.2009.07.011
Roukoz S, El Khoury G, Saghbini E, Saliba I, Khazzaka A, Rizkallah M (2020) Does the induced membrane have antibacterial properties? An experimental rat model of a chronic infected nonunion. Int Orthop 44:391–398. https://doi.org/10.1007/s00264-019-04453-4
Rousset M, Walle M, Cambou L, Mansour M, Samba A, Pereira B, Ghanem I, Canavese F (2018) Chronic infection and infected non-union of the long bones in paediatric patients: preliminary results of bone versus beta-tricalcium phosphate grafting after induced membrane formation. Int Orthop 42:385–393. https://doi.org/10.1007/s00264-017-3693-x
Hosny GA, Ahmed AA, Hussein MA (2018) Clinical outcomes with the corticotomy-first technique associated with the Ilizarov method for the management of the septic long bones non-union. Int Orthop 42:2933–2939. https://doi.org/10.1007/s00264-018-3924-9
Hernigou P, Dubory A, Homma Y, Flouzat Lachaniette CH, Chevallier N, Rouard H (2018) Single-stage treatment of infected tibial non-unions and osteomyelitis with bone marrow granulocytes precursors protecting bone graft. Int Orthop 42:2443–2450. https://doi.org/10.1007/s00264-017-3687-8
Liyan L, Aoyu L, Yunhe C, Tao X (2019) Letter to the editor: Single-stage treatment of infected tibial non-unions and osteomyelitis with bone marrow granulocytes precursors protecting bone graft. Int Orthop 43:1547. https://doi.org/10.1007/s00264-019-04304-2
Sen MK, Miclau T (2007) Autologous iliac crest bone graft: should it still be the gold standard for treating nonunions? Injury 38(Suppl 1):S75–S80. https://doi.org/10.1016/j.injury.2007.02.012
Mahendra A, Maclean AD (2007) Available biological treatments for complex non-unions. Injury 38(Suppl 4):S7–S12. https://doi.org/10.1016/s0020-1383(08)70004-4
Rodringo J (2001) Chapman MW (2001) Bone grafting, bone graft substitutes, and growth factors. In: Chapman MW, Szabo RM, Marder RA et al (eds) Chapman’s orthopedic surgery, 3rd edn. Lippincott Williams & Wilkins, Philadelphia, pp 181–211
Giannoudis PV, Kontakis G (2009) Treatment of long bone aseptic non-unions: monotherapy or polytherapy? Injury 40:1021–1022. https://doi.org/10.1016/j.injury.2009.07.064
Calori GM, Mazza E, Colombo M, Ripamonti C (2011) The use of bone-graft substitutes in large bone defects: any specific needs? Injury 42:S56–S63. https://doi.org/10.1016/j.injury.2011.06.011
Guyver P, Wakeling C, Naik K, Norton M (2012) Judet osteoperiosteal decortication for treatment of non-union: the Cornwall experience. Injury 43:1187–1192. https://doi.org/10.1016/j.injury.2012.03.035
Calori GM, Giannoudis PV (2011) Enhancement of fracture healing with the diamond concept: the role of the biological chamber. Injury 42:1191–1193. https://doi.org/10.1016/j.injury.2011.04.016
Perren SM (2002) Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg (Br) 84–B:1093–1110. https://doi.org/10.1302/0301-620x.84b8.13752
Koso RE, Terhoeve C, Steen RG, Zura R (2018) Healing, nonunion, and re-operation after internal fixation of diaphyseal and distal femoral fractures: a systematic review and meta-analysis. Int Orthop 42:2675–2683. https://doi.org/10.1007/s00264-018-3864-4
Rupp M, Biehl C, Budak M, Thormann U, Heiss C, Alt V (2018) Diaphyseal long bone nonunions - types, aetiology, economics, and treatment recommendations. Int Orthop 42:247–258. https://doi.org/10.1007/s00264-017-3734-5
Stewart SK (2019) Fracture non-union: a review of clinical challenges and future research needs. Malays Orthop J 13:1–10. https://doi.org/10.5704/MOJ.1907.001
Ollivier M, Gay AM, Cerlier A, Lunebourg A, Argenson JN, Parratte S (2015) Can we achieve bone healing using the diamond concept without bone grafting for recalcitrant tibial nonunions? Injury 46:1383–1388. https://doi.org/10.1016/j.injury.2015.03.036
Gaillard J, Masquelet AC, Boutroux P, Cambon-Binder A (2020) Induced-membrane treatment of refractory humeral non-union with or without bone defect. Orthop Traumatol Surg Res 106:803–811. https://doi.org/10.1016/j.otsr.2020.02.015
Dawson J, Kiner D, Gardner W II, Swafford R, Nowotarski PJ (2014) The reamer-irrigator-aspirator as a device for harvesting bone graft compared with iliac crest bone graft: union rates and complications. J Orthop Trauma 28:584–590. https://doi.org/10.1097/BOT.0000000000000086
Nauth A, Lee M, Gardner MJ, Brinker MR, Warner SJ, Tornetta P III, Leucht P (2018) Principles of nonunion management: state of the art. J Orthop Trauma 32(Suppl 3):S52–S57. https://doi.org/10.1097/BOT.0000000000001122
Kuehlfluck P, Moghaddam A, Helbig L, Child C, Wildemann B, Schmidmaier G, HTRG-Heidelber Trauma Research Group (2015) RIA fractions contain mesenchymal stroma cells with high osteogenic potency. Injury 46(suppl 8):S23–S32. https://doi.org/10.1016/S0020-1383(15)30051-6
Ahlmann E, Patzakis M, Roidis N, Shepherd L, Holtom P (2002) Comparison of anterior and posterior iliac crest bone grafts in terms of harvest-site morbidity and functional outcomes. J Bone Joint Surg (Am) 84–A:716–720. https://doi.org/10.2106/00004623-200205000-00003
PollonT RN, Delclaux S, Bonnevialle P, Mansat P, Bonnevialle N (2017) Persistent non-union of the humeral shaft treated by plating and autologous bone grafting. Int Orthop 41:367–373. https://doi.org/10.1007/s00264-016-3267-3
Moghaddam A, Thaler B, Bruckner T, Tanner M, Schmidmaier G (2017) Treatment of atrophic femoral non-unions according to the diamond concept: results of one- and two-step surgical procedure. J Orthop 14:123–133. https://doi.org/10.1016/j.jor.2016.10.003
Allende C, Paz A, Altube G, Boccolini H, Malvarez A, Allende B (2014) Revision with plates of humeral nonunions secondary to failed intramedullary nailing. Int Orthop 38:899–903. https://doi.org/10.1007/s00264-013-2180-2
Ballmer FT, Lambert SM, Hertel R (1998) Decortication and plate osteosynthesis for nonunion of the clavicle. J Shoulder Elbow Surg 7:581–585. https://doi.org/10.1016/s1058-2746(98)90004-0
Judet T, Richard L, de Thomasson E, Arnault O (1990) Current role of decortication in problems of bone healing. Chirurgie 116:442–447
Ramoutar DN, Rodrigues J, Quah C, Boulton C, Moran CG (2011) Judet decortication and compression plate fixation of long bone non-union: is bone graft necessary? Injury 42:1430–1434. https://doi.org/10.1016/j.injury.2011.03.045
Lai PJ, Hsu YH, Chou YC, Yeh WL, Ueng SWN, Yu YH (2019) Augmentative antirotational plating provided a significantly higher union rate than exchanging reamed nailing in treatment for femoral shaft aseptic atrophic nonunion - retrospective cohort study. BMC Musculoskelet Disord 20:127. https://doi.org/10.1186/s12891-019-2514-3
Allende C, Vanoli F, Gentile L, Gutierrez N (2018) Minimally invasive plate osteosynthesis in humerus nonunion after intramedullary nailing. Int Orthop 42:2685–2689. https://doi.org/10.1007/s00264-018-3911-1
Author information
Authors and Affiliations
Contributions
Conceptualization, Methodology and Supervision: Ali Hassan Chamseddine.
Writing and Editing the final version of the Manuscript: Ali Hassan Chamseddine Participation in Writing the Manuscript: Mark E. Mouchantaf, Kinan F. Freiha, Ali H. Asfour.
Data Collection: Mark E. Mouchantaf, Kinan F. Freiha, Ali H. Asfour.
Data Analysis: Ali Hassan Chamseddine, Abbas A. Dib, Hassan M. Wardani, Ali M. Bazzal, Georgio E. Nahed.
Literature Review and Analysis: Ali Hassan Chamseddine, Abbas A. Dib, Hassan M. Wardani, Ali M. Bazzal, Georgio E. Nahed.
Revision and Approval of the submitted final version of the Manuscript: All Authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The authors declare that the current study was approved by the Ethical Committee of their institution. The authors declare that an informed consent was obtained from all patients to participate in the current study and that the data will be subject for publication.
Consent for publication
The authors agree and consent to publish the current manuscript in “International Orthopaedics”.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chamseddine, A.H., Mouchantaf, M.E., Freiha, K.F. et al. Bridge plating with decortication, autologous bone graft, and tight closure: a “stepwise surgical diamond concept” for treatment of nonunion in a series of fifty five patients. International Orthopaedics (SICOT) 46, 1241–1251 (2022). https://doi.org/10.1007/s00264-022-05379-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05379-0