Abstract
Purpose
To verify changes in the health-related quality of life (HRQOL) of patients with musculoskeletal disorders after the coronavirus disease 2019 (COVID-19) pandemic and to assess the relationship between the patients’ change in several activities of daily living and in the HRQOL to discover factors related to the deterioration in HRQOL.
Methods
A multi-centre cross-sectional questionnaire survey was administered between November 1, 2020, and December 31, 2020, in Japan. The participants included those who visited the orthopaedics clinic within the survey period and had experienced the first and second waves of COVID-19 in Japan and the first stay-at-home order issued by the government. Patients’ HRQOL at the two different time points (pre-outbreak and post-second wave of COVID-19) was assessed with the EuroQoL-5 dimensions 5-level (EQ-5D).
Results
The survey was completed by 1254 patients (average age: 52.5 ± 21.9 years; 644 women). Among them, 431 patients (34.3%) reported a decrease in the EQ-5D index after the pandemic. The largest decrease was in the pain domain followed by the mobility domain. Multivariate logistic regression analysis revealed that the patients with decreased regular exercise habits were significantly related to deterioration in HRQOL compared with those with stable regular exercise (adjusted odds ratio = 1.76, p < 0.001) independently from age, sex, and change of symptoms.
Conclusions
Up to 35% of patients with musculoskeletal disorders reported deterioration of HRQOL after the COVID-19 pandemic. Pain and mobility rather than anxiety were the two leading factors of the HRQOL decrease. The decrease in regular exercise was related to the HRQOL decrease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has had many effects on the lives and health of persons worldwide [1]. To prevent the spread of COVID-19 and to enable health care systems to manage the increase in seriously ill persons, severe restrictions on daily life have been implemented, including home confinement or lockdown. Although such emergent countermeasures were effective to some extent in preventing the spread of COVID-19 in the community, a prolonged situation where these countermeasures persist could also negatively affect several aspects of peoples’ lives, including decrease in regular exercise and deterioration in the mental health and quality of life (QOL) [2]. Furthermore, patients with musculoskeletal disorders could experience delays in timely access to the hospital owing to fear of exposure to the infection, or could hesitate before visiting the hospital in order to prevent spreading the infection. [3]
Hence, we aimed to determine whether the current situation in which fundamental daily activity is limited owing to the COVID-19 pandemic could negatively affect the health-related QOL (HRQOL), especially the mental health, of patients with musculoskeletal disorders. We, therefore, sought (1) to assess the changes in the HRQOL of patients with musculoskeletal disorders after the first and second waves of the pandemic, and (2) to assess the relationship between the patient’s reported changes in several daily life activities and in the HRQOL, to discover factors to prevent and/or improve HRQOL deterioration.
Patients and methods
Ethical approval
All study participants provided written informed consent. The study protocol was approved by the Institutional Review Board of the representative institution (approval No: 2020–242). All information has been handled in accordance with the standards for privacy of individually identifiable health information of health insurance portability and accountability act.
Survey time points
A multi-centre cross-sectional questionnaire survey was administered between November 1, 2020, and December 31, 2020, in Osaka, Japan. In Japan, the third wave of the COVID-19 pandemic occurred during this study’s severance period. The second state of emergency with a stay-at-home order was issued by the government on January 7, 2021 (Fig. 1). Hence, our survey’s results included data from patients who had experienced the first and second waves of the COVID-19 pandemic and the first stay-at-home order issued by the government.
Study design
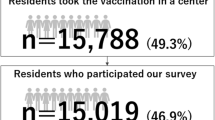
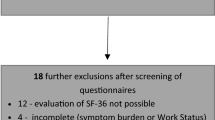
All patients who visited four private orthopaedic clinics for any symptoms in the aforementioned period were requested to participate in the current survey, and those who provided informed consent were enrolled; they were allowed to withdraw freely if they wished, during and after completing the questionnaire. All four clinics accepted patients into the study, regardless of whether they had clinician appointment, were visiting the clinic for the first time, or were on a follow-up visit. All participants completed the questionnaire at the clinic without receiving any instructions. In several questionnaires, the participants were asked to answer the questions at two time points, i.e., pre-pandemic and post-second wave (current). The patients who could not understand the questionnaires were excluded from the analysis to provide accurate data.
Questionnaire
General information
The questions included the date of birth, sex, first or return visit, patients’ complaints (spine, shoulder/hand, hip/knee joint or other), and whether they were hesitant to visit the hospital (if they had hesitated or not hesitated to visit the hospital).
Changes after the second wave of the COVID-19 pandemic
The questions included the changes in their symptoms (deteriorated, stable, stable and newly occurred after the pandemic) and the changes in their exercise habits (stable, increased, decreased, no exercise habit).
Activities of daily living (ADLs)
Criteria for determining the participant’s independence level in performing ADLs were based on the definition provided by the Japanese Ministry of Health, Labour, and Welfare [4]. The survey requested participants to answer questions regarding ADL before and after the second wave of the pandemic. The criteria include Grade J, which include those with a disability, but who were almost independent in performing ADLs and could leave home independently. Grade A included those who were almost independent in terms of performing indoor ADLs, but who required assistance when they leave home. Grade B included those who required assistance for performing indoor ADLs and remained in bed most of the time, but who could maintain a sitting position. Grade C included those who remained in bed and required assistance for toileting, eating, and changing clothes. When a patient’s answers indicated a similar ADL grade for pre- and post-second wave or a higher-grade post-pandemic compared with that pre-pandemic, he or she was considered to have stable activities. When a patient’s answers indicated a decrease in ADL after the pandemic compared to before the pandemic, he or she was considered to have decreased activity.
HRQOL index
In this cross-sectional survey, each patient’s HRQOL was assessed at two time points (pre-pandemic and post-second wave) using the EuroQoL-5 dimensions 5-level (EQ-5D) [5]. The EQ-5D measures HRQOL on a 1-to-5 scale in five dimensions, including mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. The domain scores were subsequently converted into a summarised index based on the published values proposed in a previous report [6, 7].
Statistical analysis
All patients were placed into two groups according to the change in the EQ-5D summarised index. The decreased group included those with a lower EQ-5D summarised index for the post-second wave compared with that for the pre-pandemic time point. The non-decreased group included those with a similar or higher EQ-5D index for the post-second wave compared with that for the pre-pandemic time point. The changes in the total and each domain index from pre- to post-second wave were compared between the decreased and non-decreased groups using 2-way repeated measurement analysis of variance. Subsequently, during the univariate analysis, the age, sex, complaints, along with the change in symptoms, exercise habits, and ADL were compared between the two groups using the Mann–Whitney U test for continuous values and the chi-squared test for categorical variables. The residual analysis result was described as p < 0.05 when all variables were |r|> 1.96, according to the Haberman method [8]. Finally, variables with a significance level of p < 0.05 in the univariate analysis were included in the multivariable binary logistic regression model as explanatory variables. In this analysis, the decreased group was set as an objective variable. The adjusted odds ratio (aOR) and 95% confidence intervals of the dependent variables were calculated. All analyses were performed using SPSS software (version 23.0; SPSS, Chicago, IL, USA). A p-value of < 0.05 was considered statistically significant.
Results
Overall, 1254 patients provided complete answers to all questions and were included in the analysis. The patients’ average age was 52.5 ± 21.9 years; the study included 644 women and 610 men.
Grouping based on the HRQOL changes
Among the 1254 patients, 431 (34.3%) reported a decrease in EQ-5D summarised index after the second wave and were classified into the decreased group, whereas 823 (65.7%) reported a stable or increased index after the second wave and were classified into the non-decreased group. There were significant differences in the total index changes between the decreased and non-decreased groups (p < 0.001, Fig. 2). The largest decrease was in the pain domain followed by the mobility domain (Table 1).
Univariate comparisons between the HRQOL decreased and non-decreased groups
Univariate analysis between the decreased and non-decreased groups revealed significant differences in age (p = 0.009), sex ratio (p = 0.012), hesitating to visit the hospital (p = 0.012), change in symptoms (p < 0.001), change in regular exercise (p < 0.001), and change in ADL (p < 0.001) (Table 2). Residual analysis demonstrated that the patients in the HRQOL decreased group reported higher rates of symptom deterioration and newly occurred symptoms than the HRQOL non-decreased group (p < 0.05 respectively). The patients in the HRQOL decreased group reported a significantly higher rate of decrease in their exercise habits (p < 0.05) and a lower rate of maintaining their usual exercise habits after the COVID-19 pandemic.
Multivariate comparisons: objective variable, patients who reported HRQOL decrease
Age, sex, and hesitating to visit the hospital were not significant factors in the multivariable binary logistic regression (Table 3). The changes in symptoms, regular exercise, and ADL were significant factors relating to the HRQOL decrease, and were independent of age, sex, and each other. Furthermore, patients who reported a deterioration in their symptoms or newly acquired symptoms after the second wave had a more significant deterioration in HRQOL compared to those with stable symptoms (aOR = 4.54 and 3.38, p < 0.001, respectively). Patients with decreased regular exercise habits had a more significant deterioration in HRQOL compared with those with stable regular exercise habits (aOR = 1.76, p < 0.001). An ADL decrease was significantly related to deterioration in HRQOL than stable ADL (aOR = 2.84, p < 0.001).
Discussion
In this study, nearly 35% of the patients with musculoskeletal disorders reported a HRQOL deterioration after the second wave of the COVID-19 pandemic. Contrary to our expectation, the reported decreases were in the pain and mobility subdomains, and these two, rather than the anxiety subdomain, were the leading causes of the HRQOL decrease. Additionally, the reported decrease in regular exercise habits and symptom deterioration after the pandemic’s second wave were significantly correlated with the HRQOL deterioration and these were independent of age, sex, and each other.
The minimal important difference or minimal clinically important difference (MCID) is the smallest amount of benefit that the patient can recognise and value [9]. This concept bridges the patient perspective with evidence-based medicine, especially in the evaluation of patient-reported HRQOL measures [10]. From this perspective, our study should also have used this model as the threshold to categorise the participants in the two groups. However, a disadvantage of the MCID is that it is intervention-specific and/or disease-specific. Additionally, there are numerous computational methods for calculating the MCID, leading to values with wide differences [11]. For example, a review has revealed that the EQ-5D MCID for patients with musculoskeletal disorders differs widely, ranging from 0.08 to 0.52 [12]. Considering these findings, we adopted the simple differences between the values evaluated at pre- and post-second wave of the COVID-19 outbreak as our threshold for grouping.
It is not surprising that the participants’ QOL had decreased after the second wave of the COVID-19 outbreak. Many factors, including inaccurate information about virus transmission, limited social support, financial uneasiness, and an unstable situation can increase anxiety, resulting in significant decreases in the psychological QOL [13,14,15]. Hence, we initially considered that the anxiety subdomain would be the most affected among the five EQ-5D subdomains. However, contrary to our expectation, our results demonstrated that the two major negative changes in patients with decreased HRQOL were in the mobility and pain subdomains, rather than in the anxiety subdomain. However, considering that all participants were patients who visited the orthopaedic clinic, their characteristics may differ from those of the general healthy population.
Our results demonstrated an independent relationship between symptom deterioration and decrease in HRQOL. Although some patients can be expected to experience deterioration in their musculoskeletal symptoms regardless of COVID-19, Clauw et al. reported that psychological stressors caused by the COVID-19 pandemic could trigger chronic pain exacerbation [16]. They suggested that reduced access or closure of routine clinics could result in prolonged waiting times, delays in timely access to medications due to fear of exposure to infection, and financial insecurity [16, 17]. Similarly, our survey revealed that 34% of all patients who visited the hospital during the survey period had hesitated before visiting the clinic. These patients may have potentially missed the optimal timing to receive adequate therapy. Although our study lacks a control group to validate the relationship between pain deterioration and COVID-19, physicians should pay attention to the symptoms and pain deterioration that can result in decreases in HRQOL in patients with musculoskeletal disorders after the COVID-19 pandemic.
Regular exercise is a vital management strategy for addressing chronic pain [18], mental health [19], several chronic diseases [20], life satisfaction [21], mortality, [22], and QOL [23, 24]. Additionally, regular exercise is important for improving the symptoms of patients with musculoskeletal disorders [25]. The importance of maintaining one’s physical activity during times of social restrictions and lockdowns was highlighted as an important strategy at the beginning of the pandemic [26, 27]. However, a wearable activity tracking software company collected physical activity data from 30 million users in one week in March 2020 and found a reduction in the average step counts of up to 40% in most countries compared with that in the same period the preceding year [28]. Comparably, our study revealed that 35% of the participants reported a decrease in regular exercise after the second wave of pandemic. Further, the decrease in regular exercise was related to the decrease in HRQOL of patients with musculoskeletal disease, which was independent of symptom deterioration. This evidence supports the importance of maintaining regular exercise during the COVID-19 pandemic.
In the post-COVID-19 era, our lives should not revert back to those of the pre-COVID-19 era [29]. In the post-COVID-19 era, some patients with musculoskeletal disorders may miss the optimal time to visit the hospital and/or hesitate to perform regular exercise, which can lead to a vicious circle resulting in HRQOL deterioration. Physicians, healthcare providers, and decision makers in the governmental and nongovernmental health systems should create guidelines to prepare the population for the post-COVID-19 era.
There are several limitations to our cross-sectional questionnaire survey. The major limitation is recall bias. Since we did not collect data before pandemic, the alternative would have been to ask for retrospective reports from before the pandemic. Further, negative emotions, including fear or anger related to COVID-19, could have affected the results. The second limitation is generalisability bias. All participants were those who had visited the orthopaedic clinic in the survey period during the COVID-19 pandemic. Those people may not be representative of all patients with musculoskeletal disorders, and this may potentially under-estimate some results, such as hesitation to visit the hospital. In addition, in the current study, the comorbid dementia and/or mental disorders were not assessed. Finally, this cross-sectional study could not evaluate the HRQOL changes after the patients resumed their regular exercise regimens. Therefore, a longitudinal questionnaire survey that includes a comprehensive sample of patients with musculoskeletal disorders, which had begun before the pandemic, would be helpful. However, our survey provides scientific evidence, even though it is not an editorial, letter to the editor, or an expert opinion, regarding the relationship between regular exercise and HRQOL after the COVID-19 pandemic [30]. Additionally, this study’s strengths could be the relatively large sample size that allowed assessment of the patient-reported HRQOL and the change in daily life in detail after the second wave of the pandemic.
In conclusion, nearly 35% of patients with musculoskeletal disorders reported deterioration in their HRQOL after the second wave of the COVID-19 pandemic. The leading reasons for the HRQOL decrease were pain and mobility rather than anxiety. Additionally, a decrease in regular exercise and symptom deterioration post-pandemic’s second wave were significantly correlated with HRQOL deterioration, and these were independent of age, sex, and each other. We believe our study calls the attention of physicians, healthcare providers, and decision makers in the governmental and nongovernmental health systems to create guidelines and to prepare for the post-COVID-19 era.
Availability of data and material
The data that support the findings of this study are available on request from the corresponding author, Koji Tamai. The data are not publicly available because the data contains the information that could compromise the privacy of research participants.
Code availability
Not applicable.
Change history
19 January 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00264-021-05297-7
References
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W, China Novel Coronavirus I, Research T (2020) A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382:727–733. https://doi.org/10.1056/NEJMoa2001017
Yamada M, Kimura Y, Ishiyama D, Otobe Y, Suzuki M, Koyama S, Kikuchi T, Kusumi H, Arai H (2020) Effect of the COVID-19 epidemic on physical activity in community-dwelling older adults in Japan: a cross-sectional online survey. J Nutr Health Aging 24:948–950. https://doi.org/10.1007/s12603-020-1424-2
Kulkarni K, Shah R, Armaou M, Leighton P, Mangwani J, Dias J (2021) What can we learn from the experiences and expectations of patients on growing waiting lists for planned care in the COVID-19 pandemic? Bone Jt Open 2:573–583. https://doi.org/10.1302/2633-1462.28.BJO-2021-0056.R1
Japanese Ministry of Health LaW Criteria for determination of the daily life independence level. www.mhlw.go.jp›english›database›db-hss›siel-2010-04
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, Bonsel G, Badia X (2011) Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 20:1727–1736. https://doi.org/10.1007/s11136-011-9903-x
Shiroiwa T, Fukuda T, Ikeda S, Igarashi A, Noto S, Saito S, Shimozuma K (2016) Japanese population norms for preference-based measures: EQ-5D-3L, EQ-5D-5L, and SF-6D. Qual Life Res 25:707–719. https://doi.org/10.1007/s11136-015-1108-2
Shiroiwa T, Ikeda S, Noto S, Igarashi A, Fukuda T, Saito S, Shimozuma K (2016) Comparison of value set based on DCE and/or TTO data: scoring for EQ-5D-5L Health States in Japan. Value Health 19:648–654. https://doi.org/10.1016/j.jval.2016.03.1834
Haberman SJ (1973) The analysis of residuals in cross-classified tables. Biometrics 29:205–220
Jaeschke R, Singer J, Guyatt GH (1989) Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials 10:407–415. https://doi.org/10.1016/0197-2456(89)90005-6
Barrett B, Brown D, Mundt M, Brown R (2005) Sufficiently important difference: expanding the framework of clinical significance. Med Decis Making 25:250–261. https://doi.org/10.1177/0272989X05276863
Wyrwich KW, Nienaber NA, Tierney WM, Wolinsky FD (1999) Linking clinical relevance and statistical significance in evaluating intra-individual changes in health-related quality of life. Med Care 37:469–478. https://doi.org/10.1097/00005650-199905000-00006
Coretti S, Ruggeri M, McNamee P (2014) The minimum clinically important difference for EQ-5D index: a critical review. Expert Rev Pharmacoecon Outcomes Res 14:221–233. https://doi.org/10.1586/14737167.2014.894462
Ikeda T, Igarashi A, Odani S, Murakami M, Tabuchi T (2021) Health-related quality of life during COVID-19 pandemic: assessing impacts of job loss and financial support programs in Japan. Appl Res Qual Life:1–17. https://doi.org/10.1007/s11482-021-09918-6
Gunduz N, Usen A, Aydin Atar E (2019) The impact of perceived social support on anxiety, depression and severity of pain and burnout among Turkish females with fibromyalgia. Arch Rheumatol 34:186–195. https://doi.org/10.5606/ArchRheumatol.2019.7018
Lardone A, Sorrentino P, Giancamilli F, Palombi T, Simper T, Mandolesi L, Lucidi F, Chirico A, Galli F (2020) Psychosocial variables and quality of life during the COVID-19 lockdown: a correlational study on a convenience sample of young Italians. PeerJ 8:e10611. https://doi.org/10.7717/peerj.10611
Clauw DJ, Hauser W, Cohen SP, Fitzcharles MA (2020) Considering the potential for an increase in chronic pain after the COVID-19 pandemic. Pain 161:1694–1697. https://doi.org/10.1097/j.pain.0000000000001950
Licciardone JC, Pandya V (2020) Feasibility trial of an eHealth intervention for health-related quality of life: implications for managing patients with chronic pain during the COVID-19 pandemic. Healthcare (Basel) 8. https://doi.org/10.3390/healthcare8040381
Macfarlane GJ, Kronisch C, Dean LE, Atzeni F, Hauser W, Fluss E, Choy E, Kosek E, Amris K, Branco J, Dincer F, Leino-Arjas P, Longley K, McCarthy GM, Makri S, Perrot S, Sarzi-Puttini P, Taylor A, Jones GT (2017) EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis 76:318–328. https://doi.org/10.1136/annrheumdis-2016-209724
De Moor MH, Beem AL, Stubbe JH, Boomsma DI, De Geus EJ (2006) Regular exercise, anxiety, depression and personality: a population-based study. Prev Med 42:273–279. https://doi.org/10.1016/j.ypmed.2005.12.002
Warburton DE, Bredin SS (2016) Reflections on physical activity and health: what should we recommend? Can J Cardiol 32:495–504. https://doi.org/10.1016/j.cjca.2016.01.024
Eek F, Larsson C, Wisen A, Ekvall Hansson E (2021) Self-perceived changes in physical activity and the relation to life satisfaction and rated physical capacity in Swedish adults during the COVID-19 pandemic-a cross sectional study. Int J Environ Res Public Health 18. DOI https://doi.org/10.3390/ijerph18020671
Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT, Lancet Physical Activity Series Working G (2012) Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 380:219–229. https://doi.org/10.1016/S0140-6736(12)61031-9
Rafferty MR, Schmidt PN, Luo ST, Li K, Marras C, Davis TL, Guttman M, Cubillos F, Simuni T, all NPFQIII (2017) Regular exercise, quality of life, and mobility in Parkinson’s disease: a longitudinal analysis of National Parkinson Foundation Quality Improvement Initiative Data. J Parkinsons Dis 7:193–202. https://doi.org/10.3233/JPD-160912
Chen X, Zheng Y, Zheng W, Gu K, Chen Z, Lu W, Shu XO (2009) The effect of regular exercise on quality of life among breast cancer survivors. Am J Epidemiol 170:854–862. https://doi.org/10.1093/aje/kwp209
Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, Ferreira PH, Fritz JM, Koes BW, Peul W, Turner JA, Maher CG, Working LLBPS, G, (2018) Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet 391:2368–2383. https://doi.org/10.1016/S0140-6736(18)30489-6
Chen P, Mao L, Nassis GP, Harmer P, Ainsworth BE, Li F (2020) Coronavirus disease (COVID-19): The need to maintain regular physical activity while taking precautions. J Sport Health Sci 9:103–104. https://doi.org/10.1016/j.jshs.2020.02.001
Dwyer MJ, Pasini M, De Dominicis S, Righi E (2020) Physical activity: benefits and challenges during the COVID-19 pandemic. Scand J Med Sci Sports 30:1291–1294. https://doi.org/10.1111/sms.13710
Fitbit I (2020) The impact of coronavirus on global activity. Available online: https://blog.fitbit.com/covid-19-global-activity/
Galea S, Vaughan R (2021) Preparing the public health workforce for the post-COVID-19 era. Am J Public Health 111:350–352. https://doi.org/10.2105/AJPH.2020.306110
D'Ambrosi R (2020) Orthopedics and COVID-19: Scientific Publications Rush. Indian J Orthop:1–7. https://doi.org/10.1007/s43465-020-00141-3
Acknowledgements
We thank the medical staff who were involved with the current survey in Shimada Hospital, Ishikiri Hospital, Shiraniwa Hospital, and Nishinomiya-Watanabe Hospital.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Koji Tamai, Shinji Takahashi, Masayoshi Iwamae, Shoichiro Ohyama, and Akito Yabu. The first draft of the manuscript was written by Hidetomi Terai and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki. The study protocol was approved by the Institutional Review Board of the representative institution (Osaka City University: No. 2020–242). All study participants provided written informed consent.
Consent for publication
This manuscript does not contain any data which can identify the participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of evidence: Level IV
The original version of this article was revised. The correct copyright should be "The Author(s) under exclusive licence to SICOT aisbl."
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Terai, H., Tamai, K., Takahashi, S. et al. The health-related quality of life of patients with musculoskeletal disorders after the COVID-19 pandemic. International Orthopaedics (SICOT) 46, 189–195 (2022). https://doi.org/10.1007/s00264-021-05256-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-05256-2