Abstract
Purpose
The purpose was to evaluate the impact of intra-operative administration of tranexamic acid (TXA) and pre-operative discontinuation of prophylactic chemoprophylaxis in patients undergoing internal fixation of pelvic or acetabular fractures on the need for subsequent blood transfusion. Operative time and the incidence of deep vein thrombosis (DVT) and pulmonary embolism (PE) were also assessed.
Methods
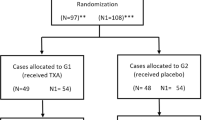
Data from a single level one trauma centre was retrospectively reviewed from January 2014 to December 2017 to identify pelvic ring or acetabular fractures managed operatively. Patients who did not receive their scheduled dose of chemoprophylaxis prior to surgery but who did receive intra-operative TXA were identified as the treatment group. Due to the interaction of VTE prophylaxis and TXA, the variables were analyzed using an interaction effect to account for administration of both individually and concomitantly.
Results
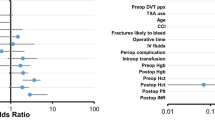
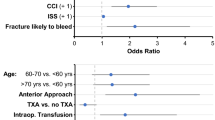
One hundred fifty-nine patients were included. The treatment group experienced a 20.7% reduction in blood product transfusion (regression coefficient (RC): − 0.207, p = 0.047, 95%CI: − 0.412 to − 0.003) and an average of 36 minutes (RC): − 36.90, p = 0.045, 95%CI: − 72.943 to − 0.841) reduction in surgical time as compared to controls. The treatment group did not experience differential rates of PE or DVT (RC: 1.302, p = 0.749, 95%CI: 0.259–6.546) or PE (RC: 1.024, p = 0.983, 95%CI: 0.114–9.208).
Conclusions
In the study population, the combination of holding pre-operative chemoprophylaxis and administering intra-operative TXA is a safe and effective combination in reducing operative time and blood product transfusions.
Similar content being viewed by others
References
Sharma OP, Oswanski MF, Joseph RJ, Tonui P, Westrick L, Raj SS, Tatchell T, Waite PJ, Gandaio A (2007) Venous thromboembolism in trauma patients. Am Surg 73:1173–1180
Kim JW, Oh CW, Oh JK, Baek SG, Lee BJ, Hong HP, Min WK (2014) The incidence and the risk factors of venous thromboembolism in Korean patients with pelvic or acetabular fractures. J Orthop Sci 19:471–477. https://doi.org/10.1007/s00776-014-0553-z
Godoy Monzon D, Iserson KV, Cid A, Vazquez JA (2012) Oral thromboprophylaxis in pelvic trauma: a standardized protocol. J Emerg Med 43:612–617. https://doi.org/10.1016/j.jemermed.2011.09.006
Dwyer EP, Moed BR (2019) Venous thromboembolism after hospital discharge in pelvic and acetabular fracture patients treated operatively. J Orthop Surg (Hong Kong) 27:2309499019832815. https://doi.org/10.1177/2309499019832815
Wang P, Kandemir U, Zhang B, Wang B, Li J, Zhuang Y, Wang H, Zhang H, Liu P, Zhang K (2019) Incidence and risk factors of deep vein thrombosis in patients with pelvic and acetabular fractures. Clin Appl Thromb Hemost 25:1076029619845066. https://doi.org/10.1177/1076029619845066
Cohen-Levy WB, Liu J, Sen M, Teperman SH, Stone ME Jr (2019) Prophylactic inferior vena cava filters for operative pelvic fractures: a twelve year experience. Int Orthop 43:2831–2838. https://doi.org/10.1007/s00264-019-04384-0
Moed BR, Miller JR, Tabaie SA (2012) Sequential duplex ultrasound screening for proximal deep venous thrombosis in asymptomatic patients with acetabular and pelvic fractures treated operatively. J tRauma Acute Care Surg 72:443–447. https://doi.org/10.1097/TA.0b013e318241090d
Montgomery KD, Geerts WH, Potter HG, Helfet DL (1996) Thromboembolic complications in patients with pelvic trauma. Clin Orthopaedics Relat Res:68–87. https://doi.org/10.1097/00003086-199608000-00010
Knudson MM, Morabito D, Paiement GD, Shackleford S (1996) Use of low molecular weight heparin in preventing thromboembolism in trauma patients. J Trauma 41:446–459
Roberts KC, Brox WT (2015) AAOS clinical practice guideline: management of hip fractures in the elderly. The Journal of the American Academy of Orthopaedic Surgeons 23:138–140. https://doi.org/10.5435/JAAOS-D-14-00433
Mont MA, Jacobs JJ (2011) AAOS clinical practice guideline: preventing venous thromboembolic disease in patients undergoing elective hip and knee arthroplasty. The Journal of the American Academy of Orthopaedic Surgeons 19:777–778
Falck-Ytter Y, Francis CW, Johanson NA, Curley C, Dahl OE, Schulman S, Ortel TL, Pauker SG, Colwell CW, Jr. (2012) Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141:e278S-e325S. https://doi.org/10.1378/chest.11-2404
Perka C (2011) Preoperative versus postoperative initiation of thromboprophylaxis following major orthopedic surgery: safety and efficacy of postoperative administration supported by recent trials of new oral anticoagulants. Thromb J 9:17. https://doi.org/10.1186/1477-9560-9-17
Randelli F, Biggi F, Della Rocca G, Grossi P, Imberti D, Landolfi R, Palareti G, Prisco D (2011) Italian intersociety consensus statement on antithrombotic prophylaxis in hip and knee replacement and in femoral neck fracture surgery. J Orthop Traumatol 12:69–76. https://doi.org/10.1007/s10195-010-0125-8
Raskob GE, Hirsh J (2003) Controversies in timing of the first dose of anticoagulant prophylaxis against venous thromboembolism after major orthopedic surgery. Chest 124:379S–385S
Hull RD, Pineo GF (1999) Extended prophylaxis against venous thromboembolism following total hip and knee replacement. Haemostasis 29(Suppl S1):23–31. https://doi.org/10.1159/000054109
Hull RD, Pineo GF, Francis C, Bergqvist D, Fellenius C, Soderberg K, Holmqvist A, Mant M, Dear R, Baylis B, Mah A, Brant R (2000) Low-molecular-weight heparin prophylaxis using dalteparin extended out-of-hospital vs in-hospital warfarin/out-of-hospital placebo in hip arthroplasty patients: a double-blind, randomized comparison. North American Fragmin Trial Investigators. Arch Intern Med 160:2208–2215
Hull RD, Pineo GF, Stein PD, Mah AF, MacIsaac SM, Dahl OE, Butcher M, Brant RF, Ghali WA, Bergqvist D, Raskob GE (2001) Extended out-of-hospital low-molecular-weight heparin prophylaxis against deep venous thrombosis in patients after elective hip arthroplasty: a systematic review. Ann Intern Med 135:858–869
Hull RD, Pineo GF, Stein PD, Mah AF, MacIsaac SM, Dahl OE, Ghali WA, Butcher MS, Brant RF, Bergqvist D, Hamulyak K, Francis CW, Marder VJ, Raskob GE (2001) Timing of initial administration of low-molecular-weight heparin prophylaxis against deep vein thrombosis in patients following elective hip arthroplasty: a systematic review. Arch Intern Med 161:1952–1960
Ktistakis I, Giannoudis V, Giannoudis PV (2016) Anticoagulation therapy and proximal femoral fracture treatment: an update. EFORT Open Rev 1:310–315. https://doi.org/10.1302/2058-5241.1.160034
Borgen PO, Dahl OE, Reikeras O (2012) Blood loss in cemented THA is not reduced with postoperative versus preoperative start of thromboprophylaxis. Clin Orthop Relat Res 470:2591–2598. https://doi.org/10.1007/s11999-012-2320-9
McCormack PL (2012) Tranexamic acid: a review of its use in the treatment of hyperfibrinolysis. Drugs 72:585–617. https://doi.org/10.2165/11209070-000000000-00000
Poeran J, Rasul R, Suzuki S, Danninger T, Mazumdar M, Opperer M, Boettner F, Memtsoudis SG (2014) Tranexamic acid use and postoperative outcomes in patients undergoing total hip or knee arthroplasty in the United States: retrospective analysis of effectiveness and safety. BMJ 349:g4829. https://doi.org/10.1136/bmj.g4829
Ho KM, Ismail H (2003) Use of intravenous tranexamic acid to reduce allogeneic blood transfusion in total hip and knee arthroplasty: a meta-analysis. Anaesth Intensive Care 31:529–537
Li JF, Li H, Zhao H, Wang J, Liu S, Song Y, Wu HF (2017) Combined use of intravenous and topical versus intravenous tranexamic acid in primary total knee and hip arthroplasty: a meta-analysis of randomised controlled trials. J Orthop Surg Res 12:22. https://doi.org/10.1186/s13018-017-0520-4
Peng Zhang MM, Jifeng Li MM, Xiao Wang MM (2017) Combined versus single application of tranexamic acid in total knee and hip arthroplasty: a meta-analysis of randomized controlled trials. Int J Surg 43:171–180. https://doi.org/10.1016/j.ijsu.2017.05.065
Jennings JD, Solarz MK, Haydel C (2016) Application of tranexamic acid in trauma and orthopedic surgery. Orthopedic Clinics North Am 47:137–143. https://doi.org/10.1016/j.ocl.2015.08.014
Luo W, Sun RX, Jiang H, Ma XL (2018) The efficacy and safety of topical administration of tranexamic acid in spine surgery: a meta-analysis. J Orthop Surg Res 13:96. https://doi.org/10.1186/s13018-018-0815-0
Yuan QM, Zhao ZH, Xu BS (2017) Efficacy and safety of tranexamic acid in reducing blood loss in scoliosis surgery: a systematic review and meta-analysis. Eur Spine J 26:131–139. https://doi.org/10.1007/s00586-016-4899-0
Amer KM, Rehman S, Amer K, Haydel C (2017) Efficacy and safety of tranexamic acid in orthopaedic fracture surgery: a meta-analysis and systematic literature review. J Orthop Trauma 31:520–525. https://doi.org/10.1097/BOT.0000000000000919
Gausden EB, Qudsi R, Boone MD, O'Gara B, Ruzbarsky JJ, Lorich DG (2017) Tranexamic acid in orthopaedic trauma surgery: a meta-analysis. J Orthop Trauma 31:513–519. https://doi.org/10.1097/BOT.0000000000000913
Lack WD, Crist BD, Seymour RB, Harvin W, Karunakar MA, Group TXAS (2017) Effect of tranexamic acid on transfusion: a randomized clinical trial in acetabular fracture surgery. J Orthop Trauma 31:526–530. https://doi.org/10.1097/BOT.0000000000000968
Colman M, Wright A, Gruen G, Siska P, Pape HC, Tarkin I (2013) Prolonged operative time increases infection rate in tibial plateau fractures. Injury 44:249–252. https://doi.org/10.1016/j.injury.2012.10.032
Viberg B, Gundtoft PH, Schonnemann J, Pedersen L, Andersen LR, Titlestad K, Madsen CF, Lauritsen J, Overgaard S (2018) Introduction of national guidelines for restrictive blood transfusion threshold for hip fracture patients--a consecutive cohort study based on complete follow-up in national databases. J Orthop Surg Res 13:116. https://doi.org/10.1186/s13018-018-0828-8
Sward-Nordmo M, Paulsen BS, Wold JK, Wehler T, Jansson PE (1991) Further structural studies of the carbohydrate moiety of the allergen Ag-54 (Cla h II) from the mould Cladosporium herbarum. Carbohydr Res 214:267–279
Dzik S, Blajchman MA, Blumberg N, Kirkley SA, Heal JM, Wood K (1996) Current research on the immunomodulatory effect of allogeneic blood transfusion. Vox Sang 70:187–194
Innerhofer P, Luz G, Spotl L, Hobisch-Hagen P, Schobersberger W, Fischer M, Nussbaumer W, Lochs A, Irschick E (1999) Immunologic changes after transfusion of autologous or allogeneic buffy coat-poor versus white cell-reduced blood to patients undergoing arthroplasty. I Proliferative T-cell responses and the balance of helper and suppressor T cells. Transfusion (Paris) 39:1089–1096
Dunne JR, Riddle MS, Danko J, Hayden R, Petersen K (2006) Blood transfusion is associated with infection and increased resource utilization in combat casualties. Am Surg 72:619–625 discussion 625-616
Bochicchio GV, Napolitano L, Joshi M, Bochicchio K, Meyer W, Scalea TM (2008) Outcome analysis of blood product transfusion in trauma patients: a prospective, risk-adjusted study. World J Surg 32:2185–2189. https://doi.org/10.1007/s00268-008-9655-0
Carson JL, Altman DG, Duff A, Noveck H, Weinstein MP, Sonnenberg FA, Hudson JI, Provenzano G (1999) Risk of bacterial infection associated with allogeneic blood transfusion among patients undergoing hip fracture repair. Transfusion 39:694–700
Fisahn C, Jeyamohan S, Norvell DC, Tubbs RS, Moisi M, Chapman JR, Page J, Oskouian RJ (2017) Association between allogeneic blood transfusion and postoperative infection in major spine surgery. Clin Spine Surg 30:E988–E992. https://doi.org/10.1097/BSD.0000000000000539
Everhart JS, Sojka JH, Mayerson JL, Glassman AH, Scharschmidt TJ (2018) Perioperative allogeneic red blood-cell transfusion associated with surgical site infection after total hip and knee arthroplasty. J Bone Joint Surg Am 100:288–294. https://doi.org/10.2106/JBJS.17.00237
Koyanagi I, Iwasaki Y, Isu T, Akino M, Abe H (1989) Significance of spinal cord swelling in the prognosis of acute cervical spinal cord injury. Paraplegia 27:190–197. https://doi.org/10.1038/sc.1989.28
Malone DL, Dunne J, Tracy JK, Putnam AT, Scalea TM, Napolitano LM (2003) Blood transfusion, independent of shock severity, is associated with worse outcome in trauma. J Trauma 54:898–905; discussion 905-897. https://doi.org/10.1097/01.TA.0000060261.10597.5C
Llewelyn CA, Taylor RS, Todd AA, Stevens W, Murphy MF, Williamson LM, Leucodepletion Study G (2004) The effect of universal leukoreduction on postoperative infections and length of hospital stay in elective orthopedic and cardiac surgery. Transfusion (Paris) 44:489–500. https://doi.org/10.1111/j.1537-2995.2004.03325.x
Frietsch T, Karger R, Scholer M, Huber D, Bruckner T, Kretschmer V, Schmidt S, Leidinger W, Weiler-Lorentz A (2008) Leukodepletion of autologous whole blood has no impact on perioperative infection rate and length of hospital stay. Transfusion (Paris) 48:2133–2142. https://doi.org/10.1111/j.1537-2995.2008.01804.x
Kim DG, Ha JK, Hwang CJ, Lee DH, Lee CS, Cho JH (2016) Is one-stage posterior corpectomy more favorable compared to decompression with fusion to control thoracic cord compression by metastasis? Clin Spine Surg. https://doi.org/10.1097/BSD.0000000000000267
Suzuki T, Morgan SJ, Smith WR, Stahel PF, Gillani SA, Hak DJ (2010) Postoperative surgical site infection following acetabular fracture fixation. Injury 41:396–399. https://doi.org/10.1016/j.injury.2009.11.005
Li Q, Liu P, Wang G, Yang Y, Dong J, Wang Y, Zhou D (2015) Risk factors of surgical site infection after acetabular fracture surgery. Surg Infect 16:577–582. https://doi.org/10.1089/sur.2014.134
Roberts I, Shakur H, Coats T, Hunt B, Balogun E, Barnetson L, Cook L, Kawahara T, Perel P, Prieto-Merino D, Ramos M, Cairns J, Guerriero C (2013) The CRASH-2 trial: a randomised controlled trial and economic evaluation of the effects of tranexamic acid on death, vascular occlusive events and transfusion requirement in bleeding trauma patients. Health Technol Assess 17:1–79. https://doi.org/10.3310/hta17100
Farrow LS, Smith TO, Ashcroft GP, Myint PK (2016) A systematic review of tranexamic acid in hip fracture surgery. Br J Clin Pharmacol 82:1458–1470. https://doi.org/10.1111/bcp.13079
Zufferey PJ, Miquet M, Quenet S, Martin P, Adam P, Albaladejo P, Mismetti P, Molliex S, tranexamic acid in hip-fracture surgery s (2010) Tranexamic acid in hip fracture surgery: a randomized controlled trial. Br J Anaesth 104:23–30. https://doi.org/10.1093/bja/aep314
Abdel MP, Chalmers BP, Taunton MJ, Pagnano MW, Trousdale RT, Sierra RJ, Lee YY, Boettner F, Su EP, Haas SB, Figgie MP, Mayman DJ (2018) Intravenous versus topical tranexamic acid in total knee arthroplasty: both effective in a randomized clinical trial of 640 patients. J Bone Joint Surg Am 100:1023–1029. https://doi.org/10.2106/JBJS.17.00908
Guo P, He Z, Wang Y, Gao F, Sun W, Guo W, Li Z, Cheng L (2018) Efficacy and safety of oral tranexamic acid in total knee arthroplasty: a systematic review and meta-analysis. Medicine 97:e0587. https://doi.org/10.1097/MD.0000000000010587
Wang S, Gao X, An Y (2017) Topical versus intravenous tranexamic acid in total knee arthroplasty: a meta-analysis of randomized controlled trials. Int Orthop 41:739–748. https://doi.org/10.1007/s00264-016-3296-y
White CC, Eichinger JK, Friedman RJ (2018) Minimizing blood loss and transfusions in total knee arthroplasty. J Knee Surg 31:594–599. https://doi.org/10.1055/s-0038-1648223
Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, Colwell CW (2008) Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 133:381S–453S. https://doi.org/10.1378/chest.08-0656
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Investigation Performed at Jackson Memorial Hospital, Miami, FL
The University of Miami Institutional Review Board approved this study. This research was previously presented at the American Academy of Orthopaedic Surgeons Annual Meeting, Mar 12–16, 2019.
Conflict of interest
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(XLSX 106 kb)
Rights and permissions
About this article
Cite this article
Cohen-Levy, W.B., Rush, A.J., Goldstein, J.P. et al. Tranexamic acid with a pre-operative suspension of anticoagulation decreases operative time and blood transfusion in the treatment of pelvic and acetabulum fractures. International Orthopaedics (SICOT) 44, 1815–1822 (2020). https://doi.org/10.1007/s00264-020-04595-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04595-w