Abstract
Purposes
To explore the efficacy and safety of multiple-dose oral tranexamic acid (TXA) on blood loss following primary total hip arthroplasty (THA).
Methods
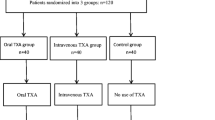
A total of 152 patients were randomized into three groups to receive 2 g of oral TXA two hours pre-operatively (group A), or another bolus of 2 g of oral TXA four hours post-operatively (group B), or another three boluses of 2 g of oral TXA four, ten, and 16 hours post-operatively (group C). The primary outcomes were total blood loss (TBL), hidden blood loss (HBL), and transfusion rate. The secondary outcomes were haemoglobin (Hb) and haematocrit (Hct) drop, the level of fibrinolysis parameters (fibrin degradation products, D-dimer), and complications (thrombotic diseases, stroke, cardiac infarction, and infection).
Results
The mean TBL and HBL in group C were lower than those in group A (p < 0.001 and p < 0.001) and group B (p = 0.012 and p = 0.029). The Hb drop on post-operative day one (POD1) and POD3 in group C was lower than those in group A (p < 0.001 and p = 0.029) and group B (p < 0.001 and p = 0.004). The difference was similar regarding Hct drop on POD3 (p < 0.001 and p = 0.014). Moreover, fibrin degradation products and D-dimer in group C were lower than in groups A and B on POD1 and POD3 (p < 0.001 and p < 0.001). The incidence of complications such as venous thromboembolism did not differ significantly among the three groups (p > 0.05).
Conclusions
Multiple boluses of oral TXA could further reduce blood loss, Hb and Hct drop, and restrain post-operative fibrinolysis in primary THA without increasing the risk of complications.
Level of Evidence I
Therapeutic study.



Similar content being viewed by others
References
Hogan CA, Golightly LK, Phong S, Dayton MR, Lyda C, Barber GR (2016) Perioperative blood loss in total hip and knee arthroplasty: outcomes associated with intravenous tranexamic acid use in an academic medical center. SAGE Open Med 4:205031211663702. https://doi.org/10.1177/2050312116637024
Loftus TJ, Spratling L, Stone BA, Xiao L, Jacofsky DJ (2016) A patient blood management program in prosthetic joint arthroplasty decreases blood use and improves outcomes. J Arthroplast 31(1):11–14. https://doi.org/10.1016/j.arth.2015.07.040
Rajesparan K, Biant LC, Ahmad M, Field RE (2009) The effect of an intravenous bolus of tranexamic acid on blood loss in total hip replacement. J Bone Joint Surg Br Vol 91(6):776–783. https://doi.org/10.1302/0301-620x.91b6.22393
Xie J, Hu Q, Ma J, Huang Q, Pei F (2017) Multiple boluses of intravenous tranexamic acid to reduce hidden blood loss and the inflammatory response following enhanced-recovery primary total hip arthroplasty: a randomised clinical trial. Bone Joint J 99-b(11):1442–1449. https://doi.org/10.1302/0301-620x.99b11.bjj-2017-0488.r1
Hao LQ, Wang QW, Chen WQ, Zhang ZY (2017) Comparison of oral and intravenous tranexamic acid in total knee and hip arthroplasty: a systematic review and meta-analysis. Int J Surg 47:52–53. https://doi.org/10.1016/j.ijsu.2017.09.009
Imai N, Dohmae Y, Suda K, Miyasaka D, Ito T, Endo N (2012) Tranexamic acid for reduction of blood loss during total hip arthroplasty. J Arthroplast 27(10):1838–1843. https://doi.org/10.1016/j.arth.2012.04.024
Lee QJ, Chang WY, Wong YC (2017) Blood-sparing efficacy of oral tranexamic acid in primary total hip arthroplasty. J Arthroplast 32(1):139–142. https://doi.org/10.1016/j.arth.2016.06.058
Malhotra R, Kumar V, Garg B (2011) The use of tranexamic acid to reduce blood loss in primary cementless total hip arthroplasty. Eur J Orthop Surg Traumatol 21(2):101–104. https://doi.org/10.1007/s00590-010-0671-z
Yue C, Kang P, Yang P, Xie J, Pei F (2014) Topical application of tranexamic acid in primary total hip arthroplasty: a randomized double-blind controlled trial. J Arthroplast 29(12):2452–2456. https://doi.org/10.1016/j.arth.2014.03.032
Kayupov E, Fillingham YA, Okroj K, Plummer DR, Moric M, Gerlinger TL, Della Valle CJ (2017) Oral and intravenous tranexamic acid are equivalent at reducing blood loss following total hip arthroplasty: a randomized controlled trial. J Bone Joint Surg Am Vol 99(5):373–378. https://doi.org/10.2106/jbjs.16.00188
Luo ZY, Wang HY, Wang D, Zhou K, Pei FX, Zhou ZK (2017) Oral vs intravenous vs topical tranexamic acid in primary hip arthroplasty: a prospective, randomized, double-blind, controlled study. J Arthroplast. https://doi.org/10.1016/j.arth.2017.09.062
Blanie A, Bellamy L, Rhayem Y, Flaujac C, Samama CM, Fontenay M, Rosencher N (2013) Duration of postoperative fibrinolysis after total hip or knee replacement: a laboratory follow-up study. Thromb Res 131(1):e6–e11. https://doi.org/10.1016/j.thromres.2012.11.006
Sharrock N, Go G, Harpel PC, Ranawat CS, Sculco TP, Salvati E (1995) Thrombogenesis during total hip-arthroplasty. Clin Orthop Relat Res (319):16–27
Iwai T, Tsuji S, Tomita T, Sugamoto K, Hideki Y, Hamada M (2013) Repeat-dose intravenous tranexamic acid further decreases blood loss in total knee arthroplasty. Int Orthop 37(3):441–445. https://doi.org/10.1007/s00264-013-1787-7
Lei Y, Xie J, Xu B, Xie X, Huang Q, Pei F (2017) The efficacy and safety of multiple-dose intravenous tranexamic acid on blood loss following total knee arthroplasty: a randomized controlled trial. Int Orthop 41(10):2053–2059. https://doi.org/10.1007/s00264-017-3519-x
Xie J, Ma J, Yao H, Yue C, Pei F (2016) Multiple boluses of intravenous tranexamic acid to reduce hidden blood loss after primary total knee arthroplasty without tourniquet: a randomized clinical trial. J Arthroplast 31(11):2458–2464. https://doi.org/10.1016/j.arth.2016.04.034
Liu X, Zhang X, Chen Y, Wang Q, Jiang Y, Zeng B (2011) Hidden blood loss after total hip arthroplasty. J Arthroplast 26(7):1100–1105.e1101. https://doi.org/10.1016/j.arth.2010.11.013
Bedard NA, Pugely AJ, Lux NR, Liu SS, Gao Y, Callaghan JJ (2017) Recent trends in blood utilization after primary hip and knee arthroplasty. J Arthroplast 32(3):724–727. https://doi.org/10.1016/j.arth.2016.09.026
Holt JB, Miller BJ, Callaghan JJ, Clark CR, Willenborg MD, Noiseux NO (2016) Minimizing blood transfusion in total hip and knee arthroplasty through a multimodal approach. J Arthroplast 31(2):378–382. https://doi.org/10.1016/j.arth.2015.08.025
Irwin A, Khan SK, Jameson SS, Tate RC, Copeland C, Reed MR (2013) Oral versus intravenous tranexamic acid in enhanced-recovery primary total hip and knee replacement: results of 3000 procedures. Bone Joint J 95-b(11):1556–1561. https://doi.org/10.1302/0301-620x.95b11.31055
Pilbrant A, Schannong M, Vessman J (1981) Pharmacokinetics and bioavailability of tranexamic acid. Eur J Clin Pharmacol 20(1):65–72
Ralley FE, Berta D, Binns V, Howard J, Naudie DD (2010) One intraoperative dose of tranexamic acid for patients having primary hip or knee arthroplasty. Clin Orthop Relat Res 468(7):1905–1911. https://doi.org/10.1007/s11999-009-1217-8
Perreault RE, Fournier CA, Mattingly DA, Junghans RP, Talmo CT (2017) Oral tranexamic acid reduces transfusions in total knee arthroplasty. J Arthroplast 32(10):2990–2994. https://doi.org/10.1016/j.arth.2017.03.063
Charoencholvanich K, Siriwattanasakul P (2011) Tranexamic acid reduces blood loss and blood transfusion after TKA: a prospective randomized controlled trial. Clin Orthop Relat Res 469(10):2874–2880. https://doi.org/10.1007/s11999-011-1874-2
Xie J, Ma J, Kang P, Zhou Z, Shen B, Yang J, Pei F (2015) Does tranexamic acid alter the risk of thromboembolism following primary total knee arthroplasty with sequential earlier anticoagulation? A large, single center, prospective cohort study of consecutive cases. Thromb Res 136(2):234–238. https://doi.org/10.1016/j.thromres.2015.05.014
Funding
This study was funded by the National Health and Family Planning Commission of the People’s Republic of China (CN) program (201302007).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
The trial was approved by the institutional review board and registered at the International Clinical Trial Registry (ChiCTR-IPR-17012266).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Cao, G., Huang, Q., Huang, Z. et al. The efficacy and safety of multiple-dose oral tranexamic acid on blood loss following total hip arthroplasty: a randomized controlled trial. International Orthopaedics (SICOT) 43, 299–305 (2019). https://doi.org/10.1007/s00264-018-3925-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-3925-8