Abstract
Introduction
Tranexamic acid is an inhibitor of fibrinolysis and thereby decreases blood loss in patients undergoing surgery.
Materials and methods
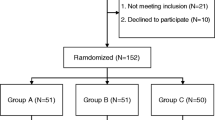
Fifty patients were randomized to Tranexamic acid (15 mg/kg) given as a bolus intravenous injection or placebo (normal saline) given intravenously, 15 min before the incision. The intraoperative and postoperative blood loss and the number of blood transfusions required were recorded. The patients were screened for deep venous thrombosis with bilateral compression ultrasonography on the 10th postoperative day. The hemoglobin level was measured preoperatively and on the 3rd postoperative day. The D-dimer levels were measured preoperatively and 24-h postoperatively.
Results
Patients receiving Tranexamic acid had a mean intraoperative blood loss of 410 ml (range, 300–510 ml) vs. 615 ml (range, 515–750 ml) (P value < 0.05) in patients receiving placebo, a postoperative blood loss of 210 ml (range, 150–325 ml) vs. 490 ml (range, 370–540 ml) (P value < 0.05), and a total need for 8 blood transfusions versus 30. 6/25 patients in first group and 18/25 patients in the placebo group required transfusion. In placebo group, the mean fall in hemoglobin was 2.9 g/dl (range, 2.5–3.2) when compared to 1.6 g/dl (1.3–2) (P < 0.05) in the Tranexamic group. At 24-h postoperatively, mean plasma D-dimer concentration in the Tranexamic group was half of that in the control group. No patient in either group had any evidence of deep vein thrombosis.
Conclusion
Tranexamic acid given as a single preoperative bolus dose reduces intraoperative and postoperative and total blood loss and transfusion requirements in primary cementless total hip replacement surgery without any increased risk of thrombus formation.


Similar content being viewed by others
References
Yamasaki S, Masuhara K, Fuji T (2004) Tranexamic acid reduces blood loss after cementless total hip arthroplasty—prospective randomized study in 40 cases. Int Orthop 28:69–73
Garneti N, Field J (2004) Bone bleeding during total hip arthroplasty after administration of tranexamic acid. J Arthroplasty 4:19
Ido K, Neo M, Asada Y, Kondo K, Morita T, Sakamoto T, Hayashi R, Kuriyama S (2000) Reduction of blood loss using tranexamic acid in total knee and hip arthroplasties. Arch Orthop Trauma Surg 120:518–520
Benoni G, Fredin H, Knebel R, Nilsson P (2001) Blood conservation with Tranexamic acid in total hip arthroplasty: a randomized, double-blind study in 40 primary operations. Acta Orthop Scand 72:442–448
Yamasaki S, Masuhara K, Fuji T (2005) Tranexamic acid reduces postoperative blood loss in cementless total hip arthroplasty. J Bone Joint Surg Am 87:766–770
Benoni G, Lethagen S, Nilsson P, Fredin H (2000) Tranexamic acid, given at the end of the operation, does not reduce postoperative blood loss in hip arthroplasty. Acta Orthop Scand 71:250–254
Ekbäck G, Axelsson K, Ryttberg L, Edlund B, Kjellberg J, Weckström J, Carlsson O, Schött U (2000) Tranexamic acid reduces blood loss in total hip replacement surgery. Anesth Analg 91:1124–1130
Clarke AM, Dorman T, Bell MJ (1992) Blood loss and transfusion requirements in total joint arthroplasty. Ann R Coll Surg Engl 74:360–363
Nilsson IM (1980) Clinical pharmacology of aminocaproic and tranexamic acids. J Clin Pathol (R Coll Pathol) Suppl 14: 41–7
Benoni G, Fredin H, Knebel R et al (2001) Blood conservation with tranexamic acid in total hip arthroplasty: a randomized, double-blind study in 40 primary operations. Acta Orthop Scand 72:5
Gill BJ, Rosenstein A (2006) The use of antifibrinolytic agents in total hip arthroplasty: a meta-analysis. J Arthroplasty 6:869–873
Sano M, Hakusui H, Kojima C, Akimoto T (1976) Absorption and excretion of Tranexamic following intravenous intramuscular and oral administrations in healthy volunteers. Clin Pharmacol Ther 7:375–382
Lindoff C, Rybo G, Astedt B (1993) Treatment with tranexamic acid during pregnancy, and the risk of thrombo-embolic complications. Thromb Haemost 70:238–240
Tanaka N, Sakahashi H, Sato E, Hirose K, Ishima T, Ishii S (2001) Timing of the administration of tranexamic acid for maximum reduction in blood loss in arthroplasty of the knee. J Bone Joint Surg Br 5:702–705
Ho KM, Ismail H (2003) Use of intravenous tranexamic acid to reduce allogeneic blood transfusion in total hip and knee arthroplasty: a meta-analysis. Anaesth Intensive Care 31:529–537
Acknowledgments
No funds were received in support of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Malhotra, R., Kumar, V. & Garg, B. The use of tranexamic acid to reduce blood loss in primary cementless total hip arthroplasty. Eur J Orthop Surg Traumatol 21, 101–104 (2011). https://doi.org/10.1007/s00590-010-0671-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-010-0671-z