Abstract
Purpose
There is a significantly higher incidence of delayed unions, non-unions, and increased healing time in diabetic patients compared with non-diabetic patients. Studies suggest that diabetics suffer from deficiencies of pancreatic stem/progenitor cells, and a clinically relevant question arises concerning the availability and functionality of progenitor cells obtained from bone marrow of diabetics for applications in bone repair.
Methods
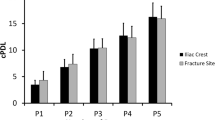
We have evaluated the cellularity and frequency of osteogenic mesenchymal stem cells (MSCs) in bone marrow from 54 diabetic patients (12 with type 1 and 42 with type 2) with tibial non-unions. These patients were treated with bone marrow MSCs (BM-MSCs) delivered in an autologous bone marrow concentrate (BMC). Clinical outcomes and marrow cellularity were compared to 54 non-diabetic, matched patients with tibial non-unions also treated with BMC.
Results
After adjusting for age and sex, no differences were identified with respect to bone marrow cellularity and MSC number among the diabetic and non-diabetic groups and both groups received approximately the same number of MSCs on average. BMC treatment promoted non-union healing in 41 diabetic patients (76 %) and 49 non-diabetic patients (91 %), but the non-diabetic patients healed more quickly and produced a larger volume of callus.
Conclusion
We recommend that diabetic patients be treated with an increased number of progenitor cells by increasing the bone marrow aspiration volume. We also anticipate a need to extend the time of casting and non-weight bearing for diabetic patients as compared with non-diabetic patients.
Similar content being viewed by others
References
Bhansali A, Upreti V, Khandelwal N et al (2009) Efficacy of autologous bone marrow-derived stem cell transplantation in patients with type 2 diabetes mellitus. Stem Cells Dev 18:1407–1415
Dumic-Cule I, Pecina M, Jelic M, Jankolija M, Popek I, Grgurevic L, Vukicevic S (2015) Biological aspect of segmental bone defects. Int Orthop 39:1005–1011
Follak N, Kl¨oting L, Wolf E, Merk H (2004) Delayed remodeling in the early period of fracture healing in spontaneously diabetic BB/OK rats depending on the diabetic metabolic state. Histol Histopathol 19:473–486
Gandhi A, Beam HA, O’Connor JP, Parsons JR, Lin SS (2005) The effects of local insulin delivery on diabetic fracture healing. Bone 37:482–490
Ganesh SP, Pietrobon R, Cecilio WA, Pan D, Lightdale N, Nunley JA (2005) The impact of diabetes on patient outcomes after ankle fracture. J Bone Joint Surg Am 87:1712–1718
Hernigou P, Poignard A, Beaujean F, Rouard H (2005) Percutaneous autologous bone-marrow grafting for nonunions. Influence of the number and concentration of progenitor cells. J Bone Joint Surg Am 87:1430–1437
Hernigou P, Guissou I, Homma Y, Poignard A, Chevallier N, Rouard H, Flouzat Lachaniette CH (2015) Percutaneous injection of bone marrow mesenchymal stem cells for ankle non-unions decreases complications in patients with diabetes. Int Orthop 39:1639–1643
Kayal RA, Tsatsas D, Bauer MA, Allen B, Al-Sebaei MO, Kakar S, Leone CW, Morgan EF, Gerstenfeld LC, Einhorn TA, Graves DT (2007) Diminished bone formation during diabetic fracture healing is related to the premature resorption of cartilage associated with increased osteoclast activity. J Bone Miner Res 22:560–568
Le Nail LR, Stanovici J, Fournier J, Splingard M, Domenech J, Rosset P (2014) Percutaneous grafting with bone marrow autologous concentrate for open tibia fractures: analysis of forty three cases and literature review. Int Orthop 38:1845–1853
Loder RT (1988) The influence of diabetes mellitus on the healing of closed fractures. Clin Orthop Relat Res 232:210–216
Loomans CJ, de Koning EJ, Staal FJ, Rookmaaker MB, Verseyden C, de Boer HC, Verhaar MC, Braam B, Rabelink TJ, van Zonneveld AJ (2004) Endothelial progenitor cell dysfunction: a novel concept in the pathogenesis of vascular complications of type 1 diabetes. Diabetes 53:195–199
Lu H, Kraut D, Gerstenfeld LC, Graves DT (2003) Diabetes interferes with the bone formation by affecting the expression of transcription factors that regulate osteoblast differentiation. Endocrinology 144:346–352
Tölli H, Kujala S, Jämsä T, Reindeer JP (2011) bone extract can heal the critical-size rat femur defect. Int Orthop 35:615–622
Wang X, Wang Y, Gou W, Lu Q, Peng J, Lu S (2013) Role of mesenchymal stem cells in bone regeneration and fracture repair: a review. Int Orthop 37:2491–2498
Zhou B, Bi YY, Han ZB, Ren H, Fang ZH, Yu XF, Poon MC, Han ZC (2006) G-CSF-mobilized peripheral blood mononuclear cells from diabetic patients augment neovascularization in ischemic limbs but with impaired capability. J Thromb Haemost 4:993–1002
Acknowledgments
We thank Ted Sand and Richard Suzuki and the other members of Celling Biosciences for the review of the final manuscript, and their help in translation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Flouzat-Lachaniette, C.H., Heyberger, C., Bouthors, C. et al. Osteogenic progenitors in bone marrow aspirates have clinical potential for tibial non-unions healing in diabetic patients. International Orthopaedics (SICOT) 40, 1375–1379 (2016). https://doi.org/10.1007/s00264-015-3046-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-3046-6