Abstract
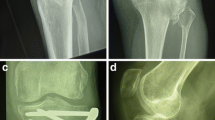
Eighteen patients with proximal tibial shaft non-union and shortening were treated. In each patient, the non-union area was débrided, realigned and stabilised with an Ilizarov lengthening frame. The tibia was gradually lengthened by 1–1.5 mm per day. After achieving the desired length, external fixation was converted to an angled blade plate and packed with cancellous bone graft. Follow-up of 16 patients for a median of 2.4 (1.2–4.5) years revealed satisfactory outcomes in all. No wound infections were noted. The described technique has a high success rate, a short treatment course and reduces patient discomfort. This method may be considered preferential treatment for all patients with the specified indications.
Résumé
18 patients présentant une pseudarthrose de la diaphyse tibiale, avec raccourcissement ont été traités. Pour chaque patient, la pseudarthrose a été mise à plat avec correction d’axe et stabilisation avec un appareil d’Ilizarov. Le tibia a été allongé progressivement de 1 à 1.5 mm par jour. Après correction de l’inégalité de longueur, la fixation externe a été remplacée par une lame plaque associée à une greffe. 16 patients ont été traités ainsi avec un suivi moyen de 2.4 ans (1.2 à 4.5). Il n’y a pas eu d’infections profondes. Cette technique entraîne un taux de succès important avec un traitement plus rapide et une amélioration du confort des patients. Cette méthode peut être considérée comme adaptée à tous les patients.

Similar content being viewed by others
References
Albright JA, Johnson TR, Saha S (1978) Principles of internal fixation. In: Ghista DN, Roaf R (eds) Orthopedic mechanics: procedures and devices. Academic, London, pp 123–229
Carpenter CA, Jupiter JB (1996) Blade plate reconstruction of metaphyseal nonunion of the tibia. Clin Orthop 332:23–28
Cierny G III, Zorn KE (1994) Segmental tibial defects: comparing conventional and Ilizarov methodologies. Clin Orthop 301:118–123
Coleman SS, Stevens PM (1976) Tibial lengthening. Clin Orthop 136:92–104
Dahl MT, Gulli B, Berg T (1994) Complications of limb lengthening: a learning curve. Clin Orthop 301:10–18
Faber FWM, Keessen W, van Roermund PM (1991) Complications of leg lengthening: 46 procedures in 28 patients. Acta Orthop Scand 62:327–332
Green SA (1994) Skeletal defects: a comparison of bone grafting and bone transport for segmental skeletal defects. Clin Orthop 301:111–117
Gustilo RB, Anderson JTT (1976) Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analysis. J Bone Joint Surg Am 58:453–458
Hang YS, Shih JS (1977) Tibial lengthening: a preliminary report. Clin Orthop 125:94–99
Ilizarov GA (1989) The tension-stress effect on the genesis and growth of tissues: part II. The influence of the rate and frequency of distraction. Clin Orthop 239:263–285
Karlstrom G, Olerud S (1974) Fractures of the tibial shaft: a critical evaluation of treatment alternatives. Clin Orthop 105:82–111
LaVelle DG (2003) Delayed union and nonunion of fractures. In: Canale ST (ed) Campbell’s operative orthopedics. Mosby, St. Louis, pp 3125–3165
Paley D (1990) Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop 250:81–104
Song HR, Cho SH, Koo KH, Jeong ST, Park YJ, Ko JH (1998) Tibial bone defects treated by internal bone transport using the Ilizarov method. Int Orthop 22:293–297
Weber BG, Brunner C (1981) The treatment of non-union without electrical stimulation. Clin Orthop 161:24–32
Wu CC (2006) Salvage of proximal tibial malunion or nonunion with the use of angled blade plate. Arch Orthop Trauma Surg 126:82–87
Wu CC, Chen WJ (2003) Tibial lengthening: technique for speedy lengthening by external fixation and secondary internal fixation. J Trauma 54:1159–1165
Wu CC, Chen WJ, Shih CH (2000) Tibial shaft malunion treated with reamed intramedullary nailing: a revised technique. Arch Orthop Trauma Surg 120:152–156
Wu CC, Shih CH (1993) Complicated open fractures of the distal tibia treated by secondary interlocking nailing. J Trauma 34:792–796
Wu CC, Shih CH, Chen WJ, Tai CL (1999) High success rate with exchange nailing to treat a tibial shaft aseptic nonunion. J Orthop Trauma 13:33–38
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, CC., Lee, ZL., Wu, CC. et al. Speeded gradual lengthening and secondary angled blade plate stabilisation for proximal tibial shaft non-union with shortening. International Orthopaedics (SICO 32, 693–696 (2008). https://doi.org/10.1007/s00264-007-0370-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-007-0370-5