Abstract
Background
Anti-programmed cell death-1 (ligand-1) antibody [PD-(L)1-Ab] can cause destructive thyroiditis and/or hypothyroidism. In addition, tyrosine kinase inhibitors (TKIs) frequently induce hypothyroidism. The aim of this prospective study is to examine the incidence and clinical characteristics of thyroid dysfunction induced by combination therapy of a PD-(L)1-Ab and TKI [PD-(L)1-Ab/TKI].
Methods
A total of 757 patients treated with PD-(L)1-Ab or PD-(L)1-Ab/TKI were evaluated for anti-thyroid antibodies (ATAs) at baseline and for thyroid function for 48 weeks after treatment initiation and then observed until the last visit.
Results
The cumulative incidences of destructive thyroiditis [4/23 (17.4%) vs. 45/734 (6.1%) patients, p < 0.001], isolated hypothyroidism [10/23 (43.5%) vs. 29/734 (4.0%) patients, p < 0.001], and all thyroid dysfunction [14/23 (60.9%) vs. 74/734 (10.1%) patients, p < 0.001] were significantly higher in the PD-(L)1-Ab/TKI group than PD-(L)1-Ab group, respectively. All patients positive for ATAs at baseline developed thyroid dysfunction after PD-(L)1-Ab/TKI treatment, a significantly higher incidence than that in those negative for ATAs at baseline [4/4 (100%) vs. 10/19 (52.6%) patients, p = 0.026].
Conclusions
The addition of TKIs increased the risk of thyroid dysfunction induced by PD-(L)1-Ab, with the risk being higher in patients positive for baseline ATAs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immune checkpoint inhibitors (ICIs), which block the immune checkpoints allowing T cells to fight cancer cells, have been developed and used for treatment of advanced malignancies. On the other hand, ICIs can lead to adverse events, termed immune-related adverse events (irAEs), in the lung, skin, gastrointestinal tract, liver, and endocrine glands [1]. Among the endocrine irAEs, thyroid dysfunction is one of the most frequently observed [2,3,4,5,6].
Although thyroid dysfunction can be induced by any class of ICIs, they occur more often following anti-programmed cell death-1 antibody (PD-1-Ab) or anti-programmed cell death-1 ligand-1 antibody (PD-L1-Ab) therapy compared with cytotoxic T-lymphocyte antigen-4 antibody monotherapy [7, 8]. Previously, we reported that thyroid dysfunction was observed in 9.9% (41/416) of patients treated with PD-1-Ab [9] and 10.1% (15/148) of patients treated with PD-L1-Ab [10]. Thyroid dysfunction is classified as thyrotoxicosis and hypothyroidism, and most cases of thyrotoxicosis are destructive thyroiditis (DT). In our previous prospective studies, the incidences of DT and hypothyroidism were 6.7 and 3.1% during PD-1-Ab therapy [9] and 5.4 and 4.7% during PD-L1-Ab therapy [10], respectively.
Tyrosine kinase inhibitors (TKIs), which target vascular endothelial growth factor (VEGF) receptors 1–3, fibroblast growth factor receptors 1–4, platelet-derived growth factor receptor α, the transmembrane tyrosine kinase rearranged during transfection, and a region of stem cell factor receptor [11, 12], are also reported to frequently induce thyroid dysfunction, mainly hypothyroidism [13]. The incidence of TKI-induced hypothyroidism varies among TKIs: 16.4–52.0% for lenvatinib [14,15,16], 14.6–23.0% for cabozantinib [17, 18], and 19.2–48.4% for axitinib [19,20,21], respectively. On the other hand, the incidence of DT in TKI treatments has been rarely reported in previous clinical trials.
Recently, PD-1-Abs or PD-L1-Abs [PD-(L)1-Abs] have been used in combination therapies with TKIs for several types of cancer. Combination therapy of a PD-(L)1-Ab plus a TKI [PD-(L)1-Ab/TKI] increased the frequency of thyroid dysfunction compared with TKI monotherapy in several clinical trials. In a phase 3 trial, hypothyroidism and thyrotoxicosis were observed in 47.2% (166/352) and 8.0% (28/352) of patients with advanced renal cell carcinoma (RCC) treated with lenvatinib plus pembrolizumab, respectively [22]. In another phase 3 trial, hypothyroidism and thyrotoxicosis were observed in 34.1% (109/320) and 10.0% (32/320) of patients with advanced RCC treated with cabozantinib plus nivolumab, respectively [23]. However, no real-world prospective studies have measured thyroid hormones at regular intervals to determine the incidence of thyroid dysfunction, as a primary outcome, after PD-(L)1-Ab/TKI compared with PD-(L)1-Ab treatment. It is also unknown whether the presence of anti-thyroid antibodies (ATAs) [anti-thyroglobulin antibody (TgAb) and/or anti-thyroid peroxidase antibody (TPOAb)] at baseline, which is a risk factor for thyroid dysfunction induced by PD-1-Ab [9, 10, 24, 25], could affect thyroid dysfunction induced by PD-(L)1-Ab/TKI as well.
The aim of the present study was to clarify the incidence of thyroid dysfunction induced by PD-(L)1-Ab/TKI treatment in patients positive or negative for ATAs at baseline in a prospective study.
Materials and methods
Patients
Since November 2, 2015, we conducted a prospective study analyzing irAEs in patients treated with ICIs to identify the clinical features of endocrine irAEs (UMIN000019024). The schema of this study is shown in Fig. 1. All patients who started nivolumab, pembrolizumab, or avelumab treatment between November 2, 2015 and July 12, 2023 at Nagoya University Hospital were included in this study since the above PD-(L)1-Abs can be used as combination therapy with TKIs. The TKIs were administered concurrently with PD-(L)1-Abs as combination therapy. Patients treated with PD-(L)1-Ab in combination with chemotherapeutic drugs other than TKIs (e.g., carboplatin, pemetrexed, cisplatin, 5-fluorouracil) were included in the PD-(L)1-Ab group since these cytotoxic chemotherapeutic agents rarely affect thyroid function. The patients were observed until the time of death, referral to another hospital, or a change in treatment from the initial PD-(L)1-Ab therapy. Patients who did not provide informed consent (n = 3) at enrollment, those with a history of ICI treatment (n = 67), those with a history of thyroid disease (n = 84) including Graves’ disease, hypothyroidism with levothyroxine replacement therapy, and thyroid tumors treated with thyroidectomy, and those with histories of both ICI treatment and thyroid disease (n = 2) were excluded (Fig. 1). All patients provided written informed consent. PD-(L)1-Ab treatment was continued until disease progression, death, or development of unacceptable severe adverse events, or if the patient withdrew consent for treatment. This study was approved by the Ethics Committee of Nagoya University Hospital (UMIN000019024).
Assessments
Thyroid function including serum levels of free T3 (FT3), free T4 (FT4), and thyroid stimulating hormone (TSH) were assessed at baseline and every 6 weeks for 24 weeks after the first administration of PD-(L)1-Ab. After the initial 24 weeks, thyroid function was evaluated at week 36, at week 48, and if clinically needed until the visits stopped. TgAb and TPOAb levels were assessed at baseline and at the onset of thyroid dysfunction. In patients who developed thyrotoxicosis, the TSH receptor antibody (TRAb) level was also measured. Serum levels of FT3, FT4, TSH, TPOAb, TgAb, and TRAb were measured as described previously [24]. Ultrasonography of the thyroid gland was performed in patients who had positive TgAb and/or TPOAb at baseline, as well as those who developed thyroid dysfunction after the initiation of PD-(L)1-Ab treatment. Thyroid dysfunction was defined according to the clinical guidelines of the Japan Endocrine Society [4]. Thyroid function is classified as thyrotoxicosis and hypothyroidism, and thyrotoxicosis is further divided into DT and hyperthyroidism (Graves’ disease). DT was defined as a decreased TSH level, elevated FT3 and/or FT4 levels, and TRAb negativity based on the diagnostic criteria for painless thyroiditis established by the Japan Thyroid Association [26]. Hyperthyroidism was defined as a decreased TSH level, elevated FT3 and/or FT4 levels, increased thyroid uptake of 99mTc pertechnetate on scintigraphy when available, and TRAb positivity based on the diagnostic criteria for Graves’ disease established by the Japan Thyroid Association [26]. Hypothyroidism was defined as an increased TSH level and decreased FT4 level. Isolated hypothyroidism was defined as hypothyroidism without preceding thyrotoxicosis. Subclinical thyroid dysfunction was defined as a TSH level beyond the normal reference range but normal parameters otherwise [27]. The cumulative incidence of thyroid dysfunction was analyzed during the initial year after the first PD-(L)1-Ab administration, since most cases of thyroid dysfunction developed during the initial 6 months, at the latest by 1 year, in our previous studies [9, 10, 24, 25].
Statistical analysis
Categorical variables are expressed as numbers and percentages and continuous variables as medians (interquartile range). The significance of differences between nominal variables was analyzed using Fisher’s exact test. The significance of differences between continuous variables was tested using the two-sample t test for normally distributed variables or the Mann–Whitney U test for nonnormally distributed variables. Kaplan–Meier curves were used to evaluate the cumulative incidence of thyroid dysfunction, differences in which were determined by log-rank test. Since the PD-(L)1-Ab/TKI group comprised both RCC and gynecologic cancer patients, a subgroup analysis of the incidence of thyroid dysfunction was performed in the RCC patients and gynecologic cancer patients. A multivariate Cox regression model (adjusted for age, sex, ICI type, ATAs at baseline, and TKI usage) was used to identify potential risk factors for the development of thyroid dysfunction. Overall survival (OS), which was determined until death from any cause, was analyzed using the Kaplan–Meier method and compared using a log-rank test; OS is expressed as the median survival time. All statistical tests were two-sided, and significance was defined as a p value < 0.05. Statistical analyses were performed using IBM SPSS Statistics 29 (IBM, Armonk, NY).
Results
Patient characteristics
A total of 757 patients with malignancies treated with a PD-(L)1-Ab (nivolumab, pembrolizumab, or avelumab, n = 734) or PD-(L)1-Ab/TKI (n = 23) were enrolled in this study (Fig. 1). The clinical characteristics of the patients treated with PD-(L)1-Ab and PD-(L)1-Ab/TKI are presented in Table 1. There was a significant difference in the tumor type between the PD-(L)1-Ab and PD-(L)1-Ab/TKI groups (Table 1). There was no significant difference in sex, age, or the prevalence of ATA (TgAb and/or TPOAb), TgAb, or TPOAb positivity at baseline between the two groups (Table 1). The PD-(L)1-Abs and TKIs used are shown in Table 1.
The risk of thyroid dysfunction was higher in the PD-(L)1-Ab/TKI group than PD-(L)1-Ab group
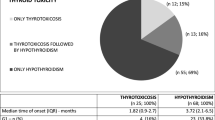
During the observation period, 74 (10.1%) and 14 (60.9%) patients developed thyroid dysfunction, and 162 (22.1%) and 4 (17.4%) patients developed subclinical thyroid dysfunction after the initiation of PD-(L)1-Ab and PD-(L)1-Ab/TKI treatment, respectively (Table 1). The cumulative incidence of thyroid dysfunction was significantly higher in the PD-(L)1-Ab/TKI group than PD-(L)1-Ab group (log-rank test, p < 0.001) (Fig. 2). The clinical characteristics of the thyroid dysfunction between the PD-(L)1-Ab and PD-(L)1-Ab/TKI groups are presented in Table 2. There was a significant difference in tumor type between the PD-(L)1-Ab and PD-(L)1-Ab/TKI groups. Regarding the type of thyroid dysfunction, the incidence of isolated hypothyroidism was significantly higher in the PD-(L)1-Ab/TKI group than PD-(L)1-Ab group [10/14 (71.4%) vs. 29/74 (39.2%) patients, p < 0.05]. There was no significant difference in age, sex, incidence of levothyroxine treatment, or the median number of days from the first administration to the diagnosis of thyroid dysfunction between the two groups, respectively (Table 2). In the multivariate Cox regression analysis, ATAs at baseline [odds ratio (OR) 6.970, 95% confidence interval (CI) 4.500–10.796, p < 0.001] and TKI usage (OR 7.578, 95% CI 4.048–14.187, p < 0.001) were significantly associated with the development of thyroid dysfunction (Supplementary Table 1).
High incidences of DT and isolated hypothyroidism induced by PD-1-Ab/TKI treatment
During the observation period, 45 (6.1%) and 4 (17.4%) patients developed thyrotoxicosis after initiation of the PD-(L)1-Ab and PD-(L)1-Ab/TKI treatments, respectively, all of whom were diagnosed with DT based on TRAb negativity (Table 2). The cumulative incidence of DT was significantly higher in the PD-(L)1-Ab/TKI group than PD-(L)1-Ab group (log-rank test, p < 0.001, Fig. 3A). There was no significant difference in the median number of days from the first administration to the diagnosis of DT between the two groups (Table 2). Furthermore, 29 (4.0%) and 10 (43.5%) patients developed isolated hypothyroidism after initiation of the PD-(L)1-Ab and PD-(L)1-Ab/TKI treatments, respectively. The cumulative incidence of isolated hypothyroidism was significantly higher in the PD-(L)1-Ab/TKI group than PD-(L)1-Ab group (log-rank test, p < 0.001, Fig. 3B). There was no significant difference in the median number of days from the first administration to the diagnosis of isolated hypothyroidism between the two groups (Table 2). In a subgroup analysis among patients with RCC and patients with gynecologic cancer, the cumulative incidences of thyroid dysfunction [14/23 (60.9%) vs. 10/56 (17.9%) patients, p < 0.001] and isolated hypothyroidism [10/23 (43.5%) vs. 3/56 (5.4%) patients, p < 0.001] were significantly higher in the PD-(L)1-Ab/TKI group than the PD-(L)1-Ab group, respectively (Supplementary Fig. 1A, C). Although a similar tendency in the incidence of DT was observed, there was no significant difference between the two groups [4/23 (17.4%) vs. 7/56 (12.5%) patients, p = 0.105] (Supplementary Fig. 1B).
Cumulative incidences of DT and isolated hypothyroidism in patients treated with PD-(L)1-Ab/TKI or PD-(L)1-Ab. Kaplan–Meier curves showing patients who developed DT (A) and patients who developed isolated hypothyroidism (B) after PD-(L)1-Ab/TKI (red line) or PD-(L)1-Ab (blue line) treatment, respectively. PD-(L)1-Ab, anti-programmed cell death-1 (ligand-1) antibody; TKI, tyrosine kinase inhibitor
Association of ATA positivity at baseline with the incidence of thyroid dysfunction
At baseline, of the patients treated with PD-(L)1-Ab or PD-(L)1-Ab/TKI, ATA (TgAb and/or TPOAb) positivity was observed in 123 (16.8%) [PD-(L)1-Ab-(+) group] and 4 (17.4%) [PD-(L)1/TKI-Ab-(+) group] patients, respectively (Table 1); the remaining 611 and 19 ATA-negative patients were designated as the PD-(L)1-Ab-(−) and PD-(L)1/TKI-Ab-(−) groups, respectively. During the observation period after ICI initiation, the cumulative incidence of thyroid dysfunction was significantly different among the four groups (log-rank test, p < 0.001, Fig. 4). In particular, the incidence was higher in the PD-(L)1-Ab-(+) group than PD-(L)1-Ab-(−) group [41/123 (33.3%) vs. 33/611 (5.4%) patients, log-rank test, p < 0.001] and in the PD-(L)1/TKI-Ab-(+) group than PD-(L)1/TKI-Ab-(-) group [4/4 (100%) vs. 10/19 (52.6%) patients, log-rank test, p = 0.026] (Fig. 4). Among the patients positive for ATAs at baseline, the cumulative incidence of thyroid dysfunction was significantly higher in the PD-(L)1/TKI-Ab-(+) group than PD-(L)1-Ab-(+) group (100% vs. 33.3% of patients, log-rank test, p = 0.002) (Fig. 4). Notably, among the patients negative for ATAs at baseline, the cumulative incidence of thyroid dysfunction was significantly higher in the PD-(L)1/TKI-Ab-(−) group than PD-(L)1-Ab-(−) group (52.6% vs. 5.4% of patients, log-rank test, p < 0.001) (Fig. 4). The risk of thyroid dysfunction was not significantly different between the PD-(L)1/TKI-Ab-(−) and PD-(L)1-Ab-(+) groups (p = 0.244).
Cumulative incidence of thyroid dysfunction in patients treated with PD-(L)1-Ab/TKI and PD-(L)1-Ab. Kaplan–Meier curves showing patients treated with PD-(L)1-Ab/TKI (red line) or PD-(L)1-Ab (blue line). Dashed and solid lines indicate the patients positive and negative for anti-thyroid antibodies at baseline, respectively. PD-(L)1-Ab, anti-programmed cell death-1 (ligand-1) antibody; TKI, tyrosine kinase inhibitor; Ab, anti-thyroid antibody
OS was not different between the PD-(L)1-Ab and PD-(L)1-Ab/TKI groups among the RCC or gynecologic cancer patients.
Next, we compared OS between patients in the PD-(L)1-Ab and PD-(L)1-Ab/TKI groups. Since the PD-(L)1-Ab/TKI group comprised both RCC and gynecologic cancer patients, OS was analyzed in these patients. There was no significant difference in OS between the PD-(L)1-Ab and PD-(L)1-Ab/TKI groups among the patients with RCC (median: 1237 days vs. not reached, p = 0.099) or those with gynecologic cancer (median: not reached vs. 650 days, p = 0.883), respectively.
Discussion
This prospective study, in which thyroid hormone levels were measured at regular intervals, demonstrated that combined use of a TKI increased the incidence of thyroid dysfunction induced by PD-(L)1-Ab treatment, and that ATA positivity at baseline was associated with an increased risk of developing thyroid dysfunction after PD-(L)1-Ab/TKI treatment. The association between TKI usage and the development of thyroid dysfunction was confirmed by multivariate Cox regression analysis. Furthermore, the increased risk of thyroid dysfunction after PD-(L)1-Ab/TKI treatment was not due to the extended observation period resulting from longer survival times.
The thyroid dysfunction induced by TKIs reported so far has been primarily hypothyroidism [28], which could explain the higher prevalence of isolated hypothyroidism induced by PD-(L)1-Ab/TKI in this study (Table 2). On the other hand, while the incidence of DT has been rarely evaluated in clinical trials of TKI treatment, a prospective study including 69 patients with RCC showed that transient thyrotoxicosis preceded TKI-induced hypothyroidism in 23.9% [29] of patients, suggesting that development of TKI-induced DT, which generally was not evaluated as a primary outcome, might have been overlooked in most previous clinical trials. Our prospective study showing that the DT incidence was higher after PD-(L)1-Ab/TKI than PD-(L)1-Ab treatment further supports this possibility. Since the subgroup analysis showed no significant difference in the incidence of DT among the RCC or gynecologic cancer patients, further analysis using a larger sample size is required.
Several studies have shown that CD4 + and CD8 + T cells infiltrate the thyroid gland in patients who develop PD-1-Ab-induced DT, suggesting that PD-1-Abs activate autoreactive T cells against the thyroid glands [30,31,32]. In a mouse model, we also reported that PD-1-Ab injections induced activation of cytotoxic CD4 + memory T cells, directly damaging thyroid cells [33]. On the other hand, TKIs can also increase autoimmunity via mechanisms such as enhancing T cell function and decreasing the number of immunosuppressive cells including regulatory T cells [34, 35]. Thus, the combined use of a PD-(L)1-Ab and TKI might cooperatively enhance the activation of T cells targeting the thyroid gland. In addition, there are reports of TKIs reducing thyroid vascular density and fenestrations via blockade of VEGF receptor signaling [13, 36, 37], inhibiting iodine uptake [38] as well as TPO activity [39], and enhancing type 3 deiodinase activity, all of which could have contributed to thyroidal dysfunction induced by PD-(L)1-Ab/TKI. Therefore, thyroid dysfunction may be more severe with PD-(L)1-Ab/TKI treatment than with PD-(L)1-Ab treatment. This hypothesis was supported by the higher incidence of overt thyroid dysfunction in the PD-(L)1-Ab/TKI group than the PD-(L)1-Ab group.
We previously reported that ATA positivity at baseline is a risk factor for thyroid dysfunction induced by PD-(L)1-Ab treatment [9, 10, 24, 25, 40,41,42,43], which was also confirmed by multivariate Cox regression analysis in this study. The present study also showed that ATA positivity at baseline is associated with the increased incidence of PD-(L)1-Ab/TKI-induced thyroid dysfunction; all four cases positive for ATAs at baseline developed thyroid dysfunction. It is also of note that the incidence of thyroid dysfunction was high even among the patients negative for ATAs at baseline in the PD-(L)1-Ab/TKI group, which was almost equivalent to that among patients positive for ATAs at baseline in the PD-(L)1-Ab group.
This study has several limitations. First, the sample size of the PD-(L)1-Ab/TKI group was relatively small because only a limited number of malignancies could be treated with PD-(L)1-Ab/TKI during the study period. Second, since the TKIs (lenvatinib, cabozantinib, and axitinib) were analyzed together as a single group, it was not possible to detect differences in the incidence of thyroid dysfunction among the three TKIs employed. Further investigation using a larger sample size for each treatment is needed. Third, there was a significant difference in the tumor types between the PD-(L)1-Ab and PD-(L)1-Ab/TKI groups. Further studies with larger sample sizes are needed to clarify the difference, if any, among the drugs and cancer types. Fourth, a comparison of the clinical characteristics of thyroid dysfunction in patients treated with PD-(L)1-Ab/TKI versus TKI monotherapy was not possible because our prospective study included only patients treated with ICIs.
In conclusion, TKIs increased the incidence of thyroid dysfunction induced by PD-(L)1-Ab, the risk of which is even higher in patients positive than in those negative for ATAs at baseline.
Data availability
No datasets were generated or analyzed during the current study.
References
Brahmer JR, Lacchetti C, Schneider BJ, Atkins MB, Brassil KJ et al (2018) Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American society of clinical oncology clinical practice guideline. J Clin Oncol 36:1714–1768
Zhai Y, Ye X, Hu F, Xu J, Guo X et al (2019) Endocrine toxicity of immune checkpoint inhibitors: a real-world study leveraging US Food and Drug Administration adverse events reporting system. J Immunother Cancer 7:286
Iwama S, Kobayashi T, Arima H (2021) Clinical characteristics, management, and potential biomarkers of endocrine dysfunction induced by immune checkpoint inhibitors. Endocrinol Metab (Seoul) 36:312–321
Arima H, Iwama S, Inaba H, Ariyasu H, Makita N et al (2019) Management of immune-related adverse events in endocrine organs induced by immune checkpoint inhibitors: clinical guidelines of the Japan Endocrine Society. Endocri J 66:581–586
Kobayashi T, Iwama S, Arima H (2024) Clinical characteristics and potential biomarkers of thyroid and pituitary immune-related adverse events. Endocr J 71:23–29
Iwama S, Kobayashi T, Yasuda Y, Arima H (2022) Immune checkpoint inhibitor-related thyroid dysfunction. Best Pract Res Clin Endocrinol Metab 36:101660
Yoo WS, Ku EJ, Lee EK, Ahn HY (2023) Incidence of endocrine-related dysfunction in patients treated with new immune checkpoint inhibitors: a meta-analysis and comprehensive review. Endocrinol Metab (Seoul) 38:750–759
Barroso-Sousa R, Barry WT, Garrido-Castro AC, Hodi FS, Min L et al (2018) Incidence of endocrine dysfunction following the use of different immune checkpoint inhibitor regimens: a systematic review and meta-analysis. JAMA Oncol 4:173–182
Iwama S, Kobayashi T, Yasuda Y, Okuji T, Ito M et al (2022) Increased risk of thyroid dysfunction by PD-1 and CTLA-4 blockade in patients without thyroid autoantibodies at baseline. J Clin Endocrinol Metab 107:e1620–e1630
Kobayashi T, Iwama S, Yamagami A, Yasuda Y, Okuji T et al (2022) Elevated TSH level, TgAb, and prior use of ramucirumab or tkis as risk factors for thyroid dysfunction in PD-L1 blockade. J Clin Endocrinol Metab 107:e4115–e4123
Yamamoto Y, Matsui J, Matsushima T, Obaishi H, Miyazaki K et al (2014) Lenvatinib, an angiogenesis inhibitor targeting VEGFR/FGFR, shows broad antitumor activity in human tumor xenograft models associated with microvessel density and pericyte coverage. Vasc Cell 6:18
Tohyama O, Matsui J, Kodama K, Hata-Sugi N, Kimura T et al (2014) Antitumor activity of lenvatinib (e7080): an angiogenesis inhibitor that targets multiple receptor tyrosine kinases in preclinical human thyroid cancer models. J Thyroid Res 2014:638747
Bhattacharya S, Goyal A, Kaur P, Singh R, Kalra S (2020) Anticancer drug-induced thyroid dysfunction. Eur Endocrinol 16:32–39
Kudo M, Finn RS, Qin S, Han KH, Ikeda K et al (2018) Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet 391:1163–1173
Yamashita T, Kudo M, Ikeda K, Izumi N, Tateishi R et al (2020) REFLECT-a phase 3 trial comparing efficacy and safety of lenvatinib to sorafenib for the treatment of unresectable hepatocellular carcinoma: an analysis of Japanese subset. J Gastroenterol 55:113–122
Koizumi Y, Hirooka M, Hiraoka A, Ochi H, Tanaka T et al (2019) Lenvatinib-induced thyroid abnormalities in unresectable hepatocellular carcinoma. Endocr J 66:787–792
Choueiri TK, Escudier B, Powles T, Tannir NM, Mainwaring PN et al (2016) Cabozantinib versus everolimus in advanced renal cell carcinoma (METEOR): final results from a randomised, open-label, phase 3 trial. Lancet Oncol 17:917–927
Smith DC, Smith MR, Sweeney C, Elfiky AA, Logothetis C et al (2013) Cabozantinib in patients with advanced prostate cancer: results of a phase II randomized discontinuation trial. J Clin Oncol 31:412–419
Rini BI, Escudier B, Tomczak P, Kaprin A, Szczylik C et al (2011) Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (AXIS): a randomised phase 3 trial. Lancet 378:1931–1939
Motzer RJ, Escudier B, Tomczak P, Hutson TE, Michaelson MD et al (2013) Axitinib versus sorafenib as second-line treatment for advanced renal cell carcinoma: overall survival analysis and updated results from a randomised phase 3 trial. Lancet Oncol 14:552–562
Tomita Y, Uemura H, Fujimoto H, Kanayama HO, Shinohara N et al (2011) Key predictive factors of axitinib (AG-013736)-induced proteinuria and efficacy: a phase II study in Japanese patients with cytokine-refractory metastatic renal cell Carcinoma. Eur J Cancer 47:2592–2602
Motzer R, Alekseev B, Rha SY, Porta C, Eto M et al (2021) Lenvatinib plus pembrolizumab or everolimus for advanced renal cell carcinoma. N Engl J Med 384:1289–1300
Choueiri TK, Powles T, Burotto M, Escudier B, Bourlon MT et al (2021) Nivolumab plus cabozantinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med 384:829–841
Kobayashi T, Iwama S, Yasuda Y, Okada N, Tsunekawa T et al (2018) Patients with antithyroid antibodies are prone to develop destructive thyroiditis by nivolumab: a prospective study. J Endocr Soc 2:241–251
Okada N, Iwama S, Okuji T, Kobayashi T, Yasuda Y et al (2020) Anti-thyroid antibodies and thyroid echo pattern at baseline as risk factors for thyroid dysfunction induced by anti-programmed cell death-1 antibodies: a prospective study. Br J Cancer 122:771–777
Japan Thyroid Association (2022) Guidelines. |https://www.japanthyroid.jp/en/guidelines.html. Accessed 5 Apr 2024
Kim HI, Kim M, Lee SH, Park SY, Kim YN et al (2017) Development of thyroid dysfunction is associated with clinical response to PD-1 blockade treatment in patients with advanced non-small cell lung cancer. Oncoimmunology 7:e1375642
Ahmadieh H, Salti I (2013) Tyrosine kinase inhibitors induced thyroid dysfunction: a review of its incidence, pathophysiology, clinical relevance, and treatment. Biomed Res Int 2013:725410
Miyake H, Kurahashi T, Yamanaka K, Kondo Y, Muramaki M et al (2010) Abnormalities of thyroid function in Japanese patients with metastatic renal cell carcinoma treated with sorafenib: a prospective evaluation. Urol Oncol 28:515–519
Neppl C, Kaderli RM, Trepp R, Schmitt AM, Berger MD et al (2018) Histology of nivolumab-induced thyroiditis. Thyroid 28:1727–1728
Zaborowski M, Sywak M, Nylen C, Gill AJ, Chou A (2020) Unique and distinctive histological features of immunotherapy-related thyroiditis. Pathology 52:271–273
Jabkowski J, Loidl A, Auinger B, Kehrer H, Sepp N et al (2021) Pembrolizumab-induced thyroiditis shows PD-L1 expressing histiocytes and infiltrating T cells in thyroid tissue—a case report. Front Immunol 12:606056
Yasuda Y, Iwama S, Sugiyama D, Okuji T, Kobayashi T et al (2021) CD4(+) T cells are essential for the development of destructive thyroiditis induced by anti-PD-1 antibody in thyroglobulin-immunized mice. Sci Transl Med 13:eabb7495
Yang J, Yan J, Liu B (2018) Targeting VEGF/VEGFR to modulate antitumor immunity. Front Immunol 9:978
Ozao-Choy J, Ma G, Kao J, Wang GX, Meseck M et al (2009) The novel role of tyrosine kinase inhibitor in the reversal of immune suppression and modulation of tumor microenvironment for immune-based cancer therapies. Cancer Res 69:2514–2522
Cao Y (2014) VEGF-targeted cancer therapeutics-paradoxical effects in endocrine organs. Nat Rev Endocrinol 10:530–539
Makita N, Miyakawa M, Fujita T, Iiri T (2010) Sunitinib induces hypothyroidism with a markedly reduced vascularity. Thyroid 20:323–326
Mannavola D, Coco P, Vannucchi G, Bertuelli R, Carletto M et al (2007) A novel tyrosine-kinase selective inhibitor, sunitinib, induces transient hypothyroidism by blocking iodine uptake. J Clin Endocrinol Metab 92:3531–3534
Wong E, Rosen LS, Mulay M, Vanvugt A, Dinolfo M et al (2007) Sunitinib induces hypothyroidism in advanced cancer patients and may inhibit thyroid peroxidase activity. Thyroid 17:351–355
Kimbara S, Fujiwara Y, Iwama S, Ohashi K, Kuchiba A et al (2018) Association of anti-thyroglobulin antibodies with the development of thyroid dysfunction induced by nivolumab. Cancer Sci 109(11):3583–3590
Zhou X, Iwama S, Kobayashi T, Ando M, Arima H (2023) Risk of thyroid dysfunction in PD-1 blockade is stratified by the pattern of TgAb and TPOAb positivity at baseline. J Clin Endocrinol Metab 108:e1056–e1062
Kobayashi T, Iwama S, Sugiyama D, Yasuda Y, Okuji T et al (2021) Anti-pituitary antibodies and susceptible human leukocyte antigen alleles as predictive biomarkers for pituitary dysfunction induced by immune checkpoint inhibitors. J Immunother Cancer 9:e002493
Iwama S, De Remigis A, Callahan MK, Slovin SF, Wolchok JD et al (2014) Pituitary expression of CTLA-4 mediates hypophysitis secondary to administration of CTLA-4 blocking antibody. Sci Transl Med 6:230–245
Acknowledgements
None.
Funding
Open Access funding provided by Nagoya University.
Author information
Authors and Affiliations
Contributions
S.I. and H.A. designed the study. T.K., S.I., and H.A. performed the clinical study. T.K., S.I., M.A., and H.A. analyzed all the data. T.K., S.I., A.Y., T.I., K.S., K.O., Y.Y., T.O., T.M., M.Sugi., D.H., H.S. and H.A. treated the enrolled patients and collected and discussed the clinical data. T.K., S.I., and H.A. wrote the manuscript. All authors were involved in the revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
S.I. received personal fees from Ono Pharmaceutical Co. Ltd., Bristol-Myers Squibb, Chugai Pharmaceutical Co., Ltd. and MSD K.K. outside of this study. T.H. received personal fees from AstraZeneca K.K., Takeda Pharmaceutical Co., Ltd., Chugai Pharmaceutical Co. Ltd., Ono Pharmaceutical Co. Ltd., Bristol-Myers Squibb Co. Ltd., Taiho Pharmaceutical Co. Ltd., MSD K.K., Merck Biopharma Co. Ltd., Pfizer Inc., and Eli Lilly Japan K.K., and grants from Novartis Pharma K.K., AstraZeneca K.K., BeiGene Inc., AbbVie Inc., Amgen Co. Ltd., and Chugai Pharmaceutical Co. Ltd., outside of this study. S.M. received grants from MSD K.K., BristolΓÇôMyers Squibb and Takara Bio Inc. outside of this study. S.A. received lecture fees from Takeda Pharmaceutical Co., Ltd. outside of this study. Y.A. received personal fees from Ono Pharmaceutical Co. Ltd., and MSD K.K. outside of this study. M.Aki. received lecture fees from Sanofi K.K., lecture fees and grant donations from Maruho Co., Ltd., clinical research funding from Novartis Pharma K.K. and Boehringer Ingelheim outside of this study. M.I. received research funding from Nippon Boehringer Ingelheim Co., Ltd, and lecture fees from Shionogi & Co., Ltd. and AstraZeneca K.K. outside of this study. H.A. received grants from Ono Pharmaceutical Co., Ltd., MSD K.K., and Chugai Pharmaceutical Co., Ltd., and personal fees from Ono Pharmaceutical Co., Ltd., BristolΓÇôMyers Squibb and MSD K.K. outside of this study. The remaining authors have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kobayashi, T., Iwama, S., Yamagami, A. et al. Combined use of tyrosine kinase inhibitors with PD-(L)1 blockade increased the risk of thyroid dysfunction in PD-(L)1 blockade: a prospective study. Cancer Immunol Immunother 73, 146 (2024). https://doi.org/10.1007/s00262-024-03733-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00262-024-03733-2