Abstract
Objective
To analyze the effectiveness of combining immune checkpoint inhibitors (ICIs) with first-line therapy in patients with advanced biliary tract cancer (BTC) and explore the biomarkers affecting the prognosis of immunotherapy, to construct a nomogram for the prediction of survival.
Methods
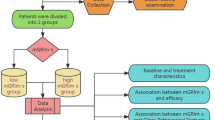
A retrospective study was conducted to include a total of 209 patients with advanced BTC treated in the first line from 2018 to 2022, divided into a combination therapy group (n = 129) and a chemotherapy-only group (n = 80) according to whether ICIs were applied in combination. Univariate and multifactorial COX regression analyses were performed on variables that may affect prognosis to identify independent influences on patient prognosis, and this was used to create nomograms, which were then prospectively validated and calibrated.
Results
The median progression-free survival (mPFS) and median overall survival (mOS) of patients in the combination therapy group were higher than those in the chemotherapy alone group [hazard ratio (HR) = 1.152, 95% confidence interval (CI): 0.7848–1.692, p = 0.0004, and HR = 1.067, 95% CI: 0.7474–1.524, p = 0.0016]. The objective response rate (ORR) of patients in the combination therapy and chemotherapy alone groups was 39.5% (51/129) vs. 27.5% (22/80), and the disease control rate (DCR) between the two groups was 89.9% (116/129) vs. 83.8% (67/80). Univariate analysis revealed the gender, presence of long-term tobacco and alcohol, degree of histological differentiation, serum albumin level, presence of liver metastases, presence of multi-visceral metastases, response, neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), monocyte-to-lymphocyte ratio (MLR), glycoprotein antigen 19-9 (CA19-9), systemic inflammatory index (SII), and controlling nutritional status (CONUT) scores were statistically significant with patient prognosis (all P values < 0.05). Multi-factor COX regression analysis was continued for the above variables, and the results showed that NLR, MLR, PLR, SII, and CONUT scores were independent influences on patients’ OS (all p values < 0.05). A nomogram (C-index 0.77, 95% CI: 0.71–0.84) was created based on these independent influences and later validated using a validation cohort (C-index 0.75, 95% CI: 0.68–0.81). The time-dependent receiver operator characteristic curve (ROC) showed that the area under curve (AUC) of the training cohort patients at 12, 18, and 24 months was 0.72 (95% CI: 0.63–0.81), 0.75 (95% CI: 0.67–0.85), and 0.77 (95% CI: 0.66–0.87) and the AUC of the validation cohort was 0.69 (95% CI: 0.58–0.79), 0.74 (95% CI: 0.65–0.87), and 0.71 (95% CI: 0.64–0.89), respectively. Finally, calibration was performed using calibration curves, and the results showed that nomograms based on inflammatory metrics and CONUT scores could be used to assess survival (12, 18, and 24 months) in patients with advanced BTC treated with ICIs in the first line.
Conclusion
Patients with advanced BTC benefit more from first-line treatment with standard chemotherapy in combination with ICIs than with chemotherapy alone. In addition, nomograms based on inflammatory metrics and CONUT scores can be used to predict survival at 12, 18, and 24 months in patients with advanced BTC treated with ICIs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Biliary tract cancer (BTC) is a malignant tumor originating from biliary tract epithelial cells, accounting for about 3% of GI malignancies, which can be divided into cholangiocarcinoma (CCA) and gallbladder carcinoma (GCA) according to the site of development, and the CCA can be further divided into intrahepatic cholangiocarcinoma (ICCA), hilar cholangiocarcinoma (HCC), and distal cholangiocarcinoma (DCCA) [1, 2]. BTC has an aggressive biological behavior, and most patients are diagnosed at an advanced stage; therefore, the prognosis is often poor, with a 5-year survival rate of less than 10% and a median survival of less than 1 year. [3,4,5]. The current treatment of advanced BTC is based on chemotherapy with Gemcitabine as the cornerstone, supplemented by targeted therapy, hepatic artery embolization chemotherapy, radiotherapy, and other therapeutic measures. Although immunotherapy based on ICIs has achieved better results in several solid tumor species, the evidence for its application in BTC is not yet sufficient [6, 7]. In the KEYNOTE-028 and KEYNOTE-224 clinical trials, single-agent pembrolizumab showed some benefits; in addition, in the KEYNOTE-158 clinical trial, patients with advanced BTC with positive PD-L1 expression achieved an ORR of 40.9% with pembrolizumab, and even 17% of patients achieved PR, but most studies mainly recommended single-agent pembrolizumab for second-line or even later treatment in BTC patients who failed first-line therapy [4, 8, 9]. Regarding the efficacy and safety of immune combination therapy in the first-line treatment of patients with advanced BTC, several phase III clinical trials have been conducted, of which only the phase III clinical trial of TOPAZ-1 met the study endpoint, and the results of this study showed that durvalumab in combination with standard chemotherapy was beneficial in terms of both overall survival (OS) and progression-free survival (PFS) in patients with advanced BTC and showed good safety and tolerability [10]. Other phases III clinical studies have not yet met their endpoints, so the evidence for the use of ICIs for the first-line treatment of patients with advanced BTC is still insufficient, so we conducted this retrospective study.
Recently, it has been found that changes in inflammation-related indicators are crucial for tumorigenesis and progression, such as NLR, PLR, MLR, SII, and other indicators be of significant value in the prognosis of esophageal, cervical, pancreatic, and hepatocellular carcinomas [11,12,13,14]. The CONUT score is also a recently developed biomarker of inflammation and nutritional status based on serum albumin, total cholesterol, and peripheral blood lymphocyte count, has been used in the prognostic assessment of gastric, esophageal, colorectal, and lung cancers, and has shown some feasibility [15,16,17,18]. However, less is known about the application of CONUT scores and inflammatory indicators in predicting and assessing long-term survival in patients with advanced BTC, especially in advanced patients receiving first-line immunotherapy; therefore, we conducted this retrospective study to construct nomograms to predict patient survival while analyzing the efficacy assessment of immune combination chemotherapy for first-line treatment of advanced BTC.
Materials and methods
Inclusion and exclusion criteria
A total of 309 patients with advanced BTC treated at the Harbin Medical University Cancer Hospital from 2018 to 2022 were included in the study. A total of 209 patients achieved PFS or OS (129 in combination with immunotherapy and 80 in the chemotherapy alone), and a total of 100 patients received immunotherapy in combination but did not achieve PFS or OS. The main inclusion criteria were: (1) pathological diagnosis of BTC (including cholangiocarcinoma and gallbladder cancer), (2) presence of local progression or distant metastasis, (3) presence of measurable target lesions, (4) no combination of other primary tumors, and (5) complete clinical record data. The exclusion criteria: (1) non-advanced BTC patients, (2) no measurable target lesions, (3) combination of other active tumors, and (4) incomplete medical records.
General information
The following variables were collected and analyzed: gender, age, height, weight, history of smoking and alcohol consumption, site of primary focus, histological classification, Eastern Cooperative Oncology Group (ECOG) score, whether ICIs were combined and the different types of ICIs, time of first definitive diagnosis, radical surgery, postoperative adjuvant chemotherapy, whether combined with radiotherapy, whether radiofrequency ablation or hepatic artery infusion chemotherapy was performed, distant metastases, hematological findings (white blood cell count, neutrophil count, platelet count, hemoglobin count, lymphocyte count, total cholesterol, serum albumin, tumor markers, etc.), imaging findings, the response of tumor, time of disease progression and reasons for progression, survival of patients at the last follow-up, time of death and the cause of death, etc. Preoperative CONUT scores were calculated from the serum albumin concentration, total lymphocyte count, and cholesterol concentration data and are shown in Table 1.
Follow-up was performed by reviewing inpatient case information, follow-up visits, and telephone contact, with the last follow-up up to September 2022. The time from the start of the first standard treatment until the patient progresses or dies is called PFS, and the time from the start of standard treatment until death (from any cause) is OS.
Efficacy evaluation standard
Both the combination therapy and chemotherapy alone groups were performed according to Response Evaluation Criteria In Solid Tumors (RECIST1.1); they can be classified as complete response (CR), partial response (PR), stable disease (SD), and progressive disease (PD). DCR is the proportion of cases other than PD after drug administration, and ORR is the percentage of patients with the best efficacy rating of CR and PR in the total number of effective cases during treatment.
Statistical methods
We used SPSS 26.0 software, R software version 4.2.1, and GraphPad prism 9.0 software for statistical analysis and plotting of the data. Continuous measures obeying normal distribution were expressed as mean ± standard (mean ± SD) deviation; one-way ANOVA was used for comparison between groups of measures obeying normal distribution with uniform variance, and LSD was used for two-way comparison; the Kruskal–Wallis test was used for those not obeying normal distribution with an uneven variance; Chi-square test was used for comparison between groups of count data, and utilization rate or composition ratio was expressed. The Pearson linear correlation was used for bivariate normal distribution, and the Spearman rank correlation was used for non-normal distribution; the Cox regression analysis was used for multi-factor analysis and made p < 0.05 as the difference was statistically significant. The 209 patients who had achieved OS were divided into a combination treatment group (n = 129) and a chemotherapy alone group (n = 90) according to the treatment regimen for effectiveness analysis, and the Kaplan–Meier method was used to plot survival curves and to compare survival by log-rank test. Univariate and multifactorial regression analyses were performed on 129 patients in the combined treatment group, and then, the training cohort was included for COX regression modeling based on the results of the multifactorial analyses, and the nomogram was plotted and the C-index was calculated using R software. The patients in the validation cohort were not from training cohort, further 100 immunotherapy patients were included as the validation cohort, and the constructed functional model was validated using ROC curves and AUC, calibration curves. All tests were bivariate, and the results with a P value < 0.05 were considered statistically significant.
Results
Basic characteristics of the combination therapy group and chemotherapy alone group
A total of 209 patients with advanced BTC treated first-line data were included in the study, including 129 patients in the combination therapy group, 81 patients (62.8%) with bile duct cancer and 25 patients (37.2%) with gallbladder cancer, and 80 patients in the chemotherapy alone group, 65 patients (81.3%) with bile duct cancer and 15 patients (18.7%) with gallbladder cancer, all with ECOG scores of 0–1. There was no statistical difference in age, gender, height, weight, primary tumor location, previous history of smoking and alcohol, total bilirubin, ALT, and AST between the patients in the combination treatment group and the chemotherapy alone group (p > 0.05). There were more men than women in both the combination therapy group and the chemotherapy alone group. Statistical differences existed between the two groups in terms of NLR, PLR, whether ICIs were used in combination, degree of tumor differentiation and the presence of multisite metastasis (p < 0.05) (Table 2).
Analysis of treatment effectiveness
A total of 10 patients (7.8%) in the combination treatment group had an efficacy evaluation of CR, 41 patients (31.8%) had an evaluation of PR, 65 patients (50.4%) had an evaluation of SD, and 13 patients (10.1%) had an evaluation of PD (Fig. 1). The ORR of patients in the combination treatment group was 39.5% (51/129) and the DCR was 89.9% (116/129). One patient (1.2%) in the chemotherapy alone group had a CR, 21 patients (26.3%) had an efficacy evaluation of PR, 45 patients (56.3%) had an efficacy evaluation of SD, and 13 (16.3%) had an efficacy evaluation of PD. The ORR of patients in the chemotherapy alone group was 27.5% (22/80) and the DCR was 83.8% (67/80).
The overall ORR and DCR of patients in the combination treatment group were higher than those in the chemotherapy alone group, 39.5% (51/129) vs. 27.5% (22/80) and 89.9% (116/129) vs. 83.8% (67/80), respectively, with statistically significant differences (p < 0.05). Patients in the chemotherapy combined with ICIs group had higher progression-free survival (PFS) and overall survival (OS) than those in the chemotherapy alone group [hazard ratio (HR) = 1.152, 95% confidence interval (CI): 0.7848–1.692, P = 0.0004 and HR = 1.067, 95% CI: 0.7474–1.524, p = 0.0016] (Fig. 2).
Basic characteristics of training cohort and validation cohort
We included 129 patients in the combination therapy group in the training cohort and randomly selected 100 patients currently receiving immune combination therapy as the validation cohort. A total of 229 patients included in the study were not statistically different in terms of gender, age, smoking and alcohol history, primary tumor site, degree of histological differentiation, NLR, PLR, MLR, SII, ECOG score, CA19-9, and CONUT score (p > 0.05). In both the training cohort and the validation cohort, there were more men than women, more patients with a history of smoking or drinking than without a history of smoking or drinking, significantly more bile duct cancer than gallbladder cancer, and the majority of patients in both groups were over 60 years of age (Table 3).
ICCA intrahepatic cholangiocarcinoma; HCCA hilar cholangiocarcinoma; DCCA distal cholangiocarcinoma; GCA gallbladder carcinoma; NLR neutrophil-to-lymphocyte ratio; PLR platelet-to-lymphocyte ratio; MLR monocyte-to-lymphocyte ratio; SII systemic inflammatory index (SII was calculated by multiplying the platelet count by the neutrophil count divided by the lymphocyte count); ALT alanine transaminase; AST aspartate transaminase; CA19-9 glycoprotein antigen 19-9; CONUT score controlling nutritional status score; other types of immune drugs included sintilimab and dovalizumab.
We performed a univariate regression analysis of the variables in the training cohort and found that patients' gender, previous history of smoking and alcohol, degree of tumor differentiation, presence of liver metastases, presence of multisite metastases, best response, NLR, PLR, MLR, CONUT score, SII, serum albumin level, and CA19-9 value were all correlated with patient prognosis (all p < 0.05). We proceeded to include the above factors in a multifactorial COX regression analysis, which showed that lower inflammatory indexes (NLR, PLR, MLR, SII) and CONUT scores (Fig. 3) were associated with better OS in patients (p < 0.05) and were independent influencers of OS (Supplementary Table).
Progression-free survival (PFS) and overall survival (OS) curves in advanced BTC patients of training cohort. A PFS according to the NLR; B PFS according to the PLR; C PFS according to the MLR; D PFS according to the SII value; E PFS according to the CONUT score; F OS according to the NLR; G OS according to the PLR; H OS according to the MLR; I OS according to the SII value; and J OS according to the CONUT score
Construction and validation of nomogram
A total of 229 patients included in the study were divided into two cohorts, 56.3% (n = 129) in the training cohort and 43.7% (n = 100) in the validation cohort, with no statistical differences between the two groups (all p > 0.05). Based on five independent prognostic factors affecting OS, a nomogram was generated in the training cohort to predict OS at 12, 18, and 24 months in patients with advanced BTC receiving first-line combination therapy with ICIs (Fig. 4).
Nomogram to predict the probability of 12-, 18-, and 24-month overall survival (OS) including the NLR (0: NLR < 3.0, 1:NLR ≥ 3.0), PLR (0:PLR < 160, 1:PLR ≥ 160), MLR(0:MLR < 2.3, 1:MLR ≥ 2.3), SII(0:SII < 830, 1:SII ≥ 830), and the CONUT score (0: CONUT score < 2, 1:CONUT score ≥ 2). The nomogram can be used to obtain the probability of 12-, 18, and 24-month OS by adding up the points identified on the point scale for each variable. Notes: CA19-9: carbohydrate antigen 19–9; COUNT: controlling nutritional status, NLR: neutrophil-to-lymphocyte ratio; PLR: platelet-to-lymphocyte ratio; MLR: monocyte-to-lymphocyte ratio; SII: systemic inflammatory index.
In the training cohort, the C-index of the nomogram was 0.771 (p = 0.0012, HR = 0.732, 95% CI: 0.693–0.797), and the C-index of the validation cohort was 0.715 (p = 0.0038, HR = 0.701, 95% CI: 0.663–0.747), which was in good agreement with the actual OS. In addition, the AUCs for the training cohort were 0.689 (95% CI:0.627–0.809), 0.741 (95% CI:0.663–0.846), and 0.712 (95% CI:0.661–0.781) at 12, 18, and 24 months, respectively (Fig. 5A). The AUCs at 12, 18, and 24 months for the validation cohort were 0.690 (95% CI:0.589–0.791), 0.727 (95% CI:0.649–0.867), and 0.770 (95% CI:0.635–0.843), respectively (Fig. 5B) (all p < 0.05). Calibration plots of OS probabilities at 12, 18, and 24 months for patients with advanced BTC showed a high degree of agreement between the actual survival predictions of the training and validation cohorts (Fig. 6).
Calibration curve of the nomogram both in the training and validation cohorts. A 2-month OS in the training cohort, B 18-month OS in the training cohort, C 24-month OS in the training cohort; D 12-month OS in the validation cohort, E 18-month OS in the validation cohort, F 24-month OS in the validation cohort
Discussion
We found in this retrospective study that patients with advanced BTC benefited more from the use of ICIs in combination with standard chemotherapy compared with chemotherapy alone at first-line treatment. In our study, the mPFS and mOS of patients in the combination therapy group were 6.37 months and 9.43 months, respectively, which were higher than those in the chemotherapy-only group; in addition, the ORR of 39.5% and DCR of 89.9% were also significantly higher in the combination therapy group compared with 27.5% and 83.8% of patients in the chemotherapy-only group. The results of this study showed full consistency with the TOPAZ-1 phase III trial and even better results than those obtained with TOPAZ-1, and in the subgroup analysis of TOPAZ-1, it was also indicated that Asian patients benefited more from treatment with durvalumab in combination with chemotherapy [19, 20]. In addition, we also found that in this retrospective study we conducted, the ORR of patients in the combination therapy group was also significantly improved compared to the KEYNOTE-028 and KEYNOTE-224 clinical trials of single-agent immunotherapy, showing that immune combination chemotherapy does benefit patients with advanced BTC more than single-agent immunotherapy [21, 22]. In a phase II clinical trial (NCT03875235), the difference in efficacy between one ICIs (GP plus durvalumab) in combination with first-line GP regimen chemotherapy and two ICIs (GP plus durvalumab plus tremelimumab) in patients with advanced BTC was investigated. As a result, they found that the ORR of dual immunotherapy combination was even 2% lower than that of single-agent immunotherapy combination; therefore, they concluded that chemotherapy combined with dual immunotherapy did not show significant advantages over single-agent immunotherapy in the first-line treatment of patients with advanced BTC, and even increased the financial cost for patients compared to single-agent immunotherapy. The study also found that the ORR of patients treated with second-line therapy in combination with immunotherapy was 20% lower than that of patients treated with first-line therapy, suggesting that patients benefit more from the combination of ICIs at first-line therapy in the treatment of patients with advanced BTC, This result is consistent with both our retrospective study and the results of the phase III clinical trial of TOPAZ-1 [7, 19, 23].
In a multifactorial regression analysis, we also found that inflammatory indicators such as NLR, PLR, MLR, SII, and CONUT score were independent influences on the prognosis of patients with advanced BTC (all p < 0.05), where lower inflammatory indicators and CONUT score were associated with better OS and PFS of patients. Ellegård et al. [24] have also found that the systemic inflammatory response is the most important biochemical indicator in malignant diseases. A large prospective cohort study of the association between systemic inflammatory markers and cancer risk was conducted by Therese Haugdahl Nøst et al. [25] who found that a variety of cancers were positively associated with the risk of SII, NLR, PLR, and MLR by analyzing the association between systemic inflammatory markers and cancer risk in 440,000 patients. Hyerim Ha1 et al. [26] found that patients with high levels of NLR, PLR, and SII had poorer OS by analyzing the hematological indicators of 158 patients with advanced BTC. Chan Su Park et al. [27] also found in a retrospective study that lower MLR was significantly associated with better OS in patients with advanced BTC treated with pembrolizumab in the second line. This result is consistent with the results in the retrospective study we conducted, in which we also found a significant correlation between lower NLR (p = 0.0083), PLR (p = 0.020), SII (p = 0.0161), and MLR (p < 0.001) and better OS of patients. Chiao-En Wu et al. [28] also found that patients with a response of CR or PR had significantly lower MLR values than those with a response of SD or PD and concluded that high MLR was an independent influencing factor for poor patient prognosis.
Sorayya Kheirouri et al [29] and Lejia Sun et al [15] both found in their studies that CONUT scores can be used to predict OS, cancer-specific survival (CSS), and (recurrence-free survival (RFS) in cancer patients, which are independent prognostic factors for OS and CSS in patients with multiple cancers, and that higher CONUT scores are associated with lower cancer survival, and the nomogram based on the CONUT score predicts OS in BTC patients and performs better than the American Joint Committee on Cancer (AJCC) staging system. The CONUT score includes total cholesterol concentration, serum albumin concentration, and peripheral blood lymphocyte count. Total serum cholesterol can reflect the body’s lipid metabolism ability, serum albumin can reflect the body’s protein synthesis ability, and peripheral blood lymphocyte count is similar to NLR, PLR, and other inflammation indicators, which can reflect the body’s immune function [30, 31]. However, many believe that the hyposerum albuminemia seen in patients with advanced cancer may be more related to the systemic inflammatory response, and therefore, it is more recommended to consider serum albumin as an indicator of inflammation rather than nutrition in the CONUT score [15, 32]. In addition, a higher CONUT score indicates not only a poor nutritional status but also a degree of impaired immune function, which may be associated with a poorer prognosis, as it has been found that the nutritional status of patients is closely related to the normal functioning of the immune system, and that poor nutritional status leads to immune system dysfunction, with varying degrees of dysfunction of immune cells such as lymphocytes, macrophages and neutrophils [33, 34]. The results of this retrospective study we conducted also showed a significant correlation between better OS and lower CONUT scores in patients with advanced BTC treated with the combination of ICIs (p = 0.0051).
Although there have been many studies confirming the prognostic role of inflammatory biomarkers in patients with BTC, there is a paucity of studies on the impact and predictive role of inflammatory indicators and the CONUT score in patients with advanced BTC who receive ICIs in combination with first-line therapy [14, 35]. As far as we know, this is the first study to assess the prognostic relevance of NLR, PLR, MLR, SII, and CONUT scores to patients with advanced BTC receiving first-line ICIs in combination with chemotherapy. We identified NLR, PLR, MLR, SII, and CONUT scores as independent influences on PFS and OS in patients with advanced BTC based on multifactorial regression analysis, which was considered and included in the final nomogram and validated. Both the training and validation cohorts were statistically significant (both p < 0.05), with a C-index of 0.77 (95% CI: 0.71–0.84) for the training cohort and 0.75 (95% CI: 0.68–0.81) for the validation cohort for the nomogram. In addition, the AUC values were greater than 0.65 at 12, 18 and 24 months for both the training and validation cohorts (all p < 0.05). Our nomograms were also well calibrated and ultimately found to have better clinical prognostic value than any single prognostic factor.
This retrospective study of ours was carried out based on clinical reality and analyzed the effectiveness of combined ICIs in patients with advanced BTC at the time of first-line treatment and produced positive results. The currently known clinical evidence on the use of ICIs for the first-line treatment of patients with advanced BTC is insufficient, as most phase II/III clinical trials are still ongoing, except for the phase III clinical trial of TOPAZ-1, which is already conclusive, so this study we conducted provides a meaningful reference on the feasibility of first-line application of ICIs for patients with advanced BTC. In addition, we developed a nomogram for predicting 12-, 18- and 24-month survival in patients with advanced BTC based on multifactorial analysis; according to us, this nomogram is the first model to predict the prognosis of patients with advanced BTC receiving first-line immune combination therapy, and the model was prospectively validated in the validation cohort and yielded results that were generally consistent with the training cohort. Our nomogram has been calibrated and tested and proven to be realistic and practical, allowing simple and intuitive prediction of patient OS at 12, 18, and 24 months. However, there are also some shortcomings in our study. Studies failed to analyze the adverse effects and safety between immune combination therapy and patients treated with chemotherapy alone; failed to sequence cancer-related genomes or exons to explore possible associations between immunotherapy effects and the genome of advanced BTC to more precisely guide the practical application of immunotherapy in the clinic and to aid the effective screening of target populations. Our nomogram has good predictive power for the entire cohort, but has insufficient risk stratification power for patients in different subgroups; moreover, the nomogram was generated based on clinical data from a single institution in China, without including data from other countries or regions and excluding a large number of data with poor medical records, which may lead to a certain degree of selection bias.
In conclusion, the combination of ICIs with first-line treatment in patients with advanced BTC can effectively prolong the survival of patients. In addition, nomograms based on independent prognostic factors such as CONUT score, NLR, PLR, MLR, and SII can be used to predict the long-term survival of patients with advanced BTC treated with ICIs in the first line, and their predictive ability is better than any single factor, which can more accurately assess the OS of patients with advanced BTC and provide more personalized guidance for patient treatment selection.
Data availability and materials
All data and materials are real and available.
References
Andersen JB, Spee B, Blechacz BR et al (2012) Genomic and genetic characterization of cholangiocarcinoma identifies therapeutic targets for tyrosine kinase inhibitors. Gastroenterology 142(4):1021–31.e15
Valle JW, Kelley RK, Nervi B et al (2021) Biliary tract cancer. Lancet 397(10272):428–444
Brindley PJ, Bachini M, Ilyas SI, Khan SA, Loukas A, Sirica AE, Teh BT, Wongkham S, Gores GJ (2021) Cholangiocarcinoma. Nat Rev Dis Primers 7(1):65
Guo X, Shen W (2020) Latest evidence on immunotherapy for cholangiocarcinoma. Oncol Lett 20(6):381
Song W, Zhu ZG, Wu Q et al (2018) A nomogram to predict overall survival for biliary tract cancer. Cancer Manag Res 10:1535–1541
Morizane C, Okusaka T, Mizusawa J et al (2019) Combination gemcitabine plus S-1 versus gemcitabine plus cisplatin for advanced/recurrent biliary tract cancer: the FUGA-BT (JCOG1113) randomized phase III clinical trial. Ann Oncol 30(12):1950–1958
Hindson J (2022) Gemcitabine and cisplatin plus immunotherapy in advanced biliary tract cancer: a phase II study. Nat rev gastro hepat 19(5):280
Piha-Paul SA, Oh DY, Ueno M et al (2020) Efficacy and safety of pembrolizumab for the treatment of advanced biliary cancer: results from the KEYNOTE-158 and KEYNOTE-028 studies. Int J Cancer 147(8):2190–2198
Chen X, Qin S, Gu S et al (2021) Camrelizumab plus oxaliplatin-based chemotherapy as first-line therapy for advanced biliary tract cancer: a multicenter, phase 2 trial. Int J Cancer 149(11):1944–1954
Yuan ZG, Zeng TM, Tao CJ (2022) Current and emerging immunotherapeutic approaches for biliary tract cancers. Hepatobil Pancreat Dis Int 21:440–449
Li C, Lin JW, Yeh HL et al (2021) Good prediction of treatment responses to neoadjuvant chemoradiotherapy for esophageal cancer based on preoperative inflammatory status and tumor glucose metabolism. Sci Rep 11(1):11626
Zheng J, Cai J, Li H et al (2017) Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio as prognostic predictors for hepatocellular carcinoma patients with various treatments: a meta-analysis and systematic review. Cell Physiol Biochem 44(3):967–981
Jomrich G, Paireder M, Kristo I et al (2021) High systemic immune-inflammation index is an adverse prognostic factor for patients with gastroesophageal adenocarcinoma. Ann Surg 273(3):532–541
Fang L, Yan FH, Liu C et al (2021) Systemic inflammatory biomarkers, especially fibrinogen to albumin ratio, predict prognosis in patients with pancreatic cancer. Cancer Res Treat 53(1):131–139
Sun L, Su S, Xiong J et al (2021) Controlling nutritional status score as a prognostic marker to predict overall survival in resected biliary tract cancers. Ann Transl Med 9(8):644
Qiu Y, You J, Wang K et al (2020) Effect of whole-course nutrition management on patients with esophageal cancer undergoing concurrent chemoradiotherapy: a randomized control trial. Nutrition 69:110558
Miyata T, Yamashita YI, Higashi T et al (2018) The prognostic impact of controlling nutritional status (CONUT) in intrahepatic cholangiocarcinoma following curative hepatectomy: a retrospective single institution study. World J Surg 42(4):1085–1091
Yang C, Wei C, Wang S et al (2019) Combined features based on preoperative controlling nutritional status score and circulating tumour cell status predict prognosis for colorectal cancer patients treated with curative resection. Int J Biol Sci 15(6):1325–1335
Oh DY, Lee KH, Lee DW et al (2022) Gemcitabine and cisplatin plus durvalumab with or without tremelimumab in chemotherapy-naive patients with advanced biliary tract cancer: an open-label, single-centre, phase 2 study. Lancet Gastroenterol Hepatol 7(6):522–532
Woods E, Le D, Jakka BK et al (2022) Changing landscape of systemic therapy in biliary tract cancer. Cancers 14(9):2137
Ott PA, Bang YJ, Piha-Paul SA et al (2019) T-cell-inflamed gene-expression profile, programmed death ligand 1 expression, and tumor mutational burden predict efficacy in patients treated with pembrolizumab across 20 cancers: KEYNOTE-028. J Clin Oncol 37(4):318–327
Kudo M, Finn RS, Edeline J et al (2022) Updated efficacy and safety of KEYNOTE-224: a phase II study of pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib. Eur J Cancer 167(1):1–12
Mirallas O, López-Valbuena D, García-Illescas D et al (2022) Advances in the systemic treatment of therapeutic approaches in biliary tract cancer. ESMO Open 7(3):100503
Ellegård LH, Bosaeus IG (2008) Biochemical indices to evaluate nutritional support for malignant disease. Clin Chim Acta 390(1–2):23–27
Nost TH, Alcala K, Urbarova I et al (2021) Systemic inflammation markers and cancer incidence in the UK Biobank. Eur J Epidemiol 36(8):841–848
Ha H, Nam AR, Bang JH et al (2016) Soluble programmed death-ligand 1 (sPDL1) and neutrophil-to-lymphocyte ratio (NLR) predicts survival in advanced biliary tract cancer patients treated with palliative chemotherapy. Oncotarget 7(47):76604–76612
Park CS, Sung MJ, Kim SJ et al (2022) Prognostic factors in patients treated with pembrolizumab as a second-line treatment for advanced biliary tract cancer. Cancers 14(17):4323
Wu CE, Chou WC, Hsieh CH et al (2020) Prognostic and predictive factors for Taiwanese patients with advanced biliary tract cancer undergoing frontline chemotherapy with gemcitabine and cisplatin: a real-world experience. BMC Cancer 20(1):422
Kheirouri S, Alizadeh M (2021) Prognostic potential of the preoperative controlling nutritional status (CONUT) score in predicting survival of patients with cancer: a systematic review. Adv nutr 12(1):234–250
Chang L, Cheng Q, Ma Y et al (2022) Prognostic effect of the controlling nutritional status score in patients with esophageal cancer treated with immune checkpoint inhibitor. J immunother 45(9):415
Tsunematsu M, Haruki K, Fujiwara Y et al (2021) Preoperative controlling nutritional status (CONUT) score predicts long-term outcomes in patients with non-B non-C hepatocellular carcinoma after curative hepatic resection. Langenbeck Arch Surg 406(1):99–107
Crumley AB, Stuart RC, Mckernan M et al (2010) Is hypoalbuminemia an independent prognostic factor in patients with gastric cancer? World J Surg 34(10):2393–2398
Conci S, Campagnaro T, Danese E et al (2021) Role of inflammatory and immune-nutritional prognostic markers in patients undergoing surgical resection for biliary tract cancers. Cancers 13(14):3594
Jayarajan S, Daly JM (2011) The relationships of nutrients, routes of delivery, and immunocompetence. Surg Clin N Am 91(4):737–753
Raucci MG, Fasolino I, Caporali M et al (2019) Exfoliated black phosphorus promotes in vitro bone regeneration and suppresses osteosarcoma progression through cancer-related inflammation inhibition. ACS Appl Mater Inter 11(9):9333–9342
Acknowledgements
Not applicable.
Funding
This study was funded by the Haiyan Scientific Research Fund of Harbin Medical University Cancer Hospital (JJZD2020-03) and Beijing Medical Award Foundation (YXJL-2022-0800-0015).
Author information
Authors and Affiliations
Contributions
All authors are involved in the creation of manuscripts by making specific contributions such as CRediT.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Consent for publication
All patients included in this study signed the Second Use Informed Consent for Historical Data/Biospecimens at Harbin Medical University-affiliated Oncology Hospital.
Ethics approval and consent to participate
This study was reviewed and approved by the Board of Directors of Harbin Medical University Cancer Hospital for inclusion in the review. Study participants provided written informed consent for the publication of any potentially identifiable image or data contained herein. The retrospective study was approved by the Ethics Committee of Harbin Medical University Cancer Hospital prior to being performed (Approval no. is: KY2022-14). The study follows the World Medical Association Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, Z., Wang, D., Zhang, J. et al. Comparison of the effectiveness of chemotherapy combined with immunotherapy and chemotherapy alone in advanced biliary tract cancer and construction of the nomogram for survival prediction based on the inflammatory index and controlling nutritional status score. Cancer Immunol Immunother 72, 3635–3649 (2023). https://doi.org/10.1007/s00262-023-03513-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-023-03513-4