Abstract
Transmembrane protein GARP binds latent TGF-β1 to form GARP:(latent)TGF-β1 complexes on the surface of several cell types including Tregs, B-cells, and platelets. Upon stimulation, these cells release active TGF-β1. Blocking TGF-β1 activation by Tregs with anti-GARP:TGF-β1 mAbs overcomes resistance to PD1/PD-L1 blockade and induces immune-mediated regressions of murine tumors, indicating that Treg-derived TGF-β1 inhibits anti-tumor immunity. TGF-β1 exerts a vast array of effects on immune responses. For example, it favors differentiation of TH17 cells and B-cell switch to IgA production, two important processes for mucosal immunity. Here, we sought to determine whether treatment with anti-GARP:TGF-β1 mAbs would perturb immune responses to intestinal bacterial infection. We observed no aggravation of intestinal disease, no systemic dissemination, and no alteration of innate or adaptative immune responses upon oral gavage of C. rodentium in highly susceptible Il22r−/− mice treated with anti-GARP:TGF-β1 mAbs. To examine the effects of GARP:TGF-β1 blockade on Ig production, we compared B cell- and TH cell- responses to OVA or CTB protein immunization in mice carrying deletions of Garp in Tregs, B cells, or platelets. No alteration of adaptive immune responses to protein immunization was observed in the absence of GARP on any of these cells. Altogether, we show that antibody-mediated blockade of GARP:TGF-β1 or genetic deletion of Garp in Tregs, B cells or platelets, do not alter innate or adaptive immune responses to intestinal bacterial infection or protein immunization in mice. Anti-GARP:TGF-β1 mAbs, currently tested for cancer immunotherapy, may thus restore anti-tumor immunity without severely impairing other immune defenses.
Précis
Immunotherapy with GARP:TGF-β1 mAbs may restore anti-tumor immunity without impairing immune or inflammatory responses required to maintain homeostasis or host defense against infection, notably at mucosal barriers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
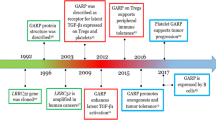
Transforming growth factor-β1 (TGF-β1) is a potent immunosuppressive cytokine that plays an important role in the maintenance of immune tolerance [1, 2]. Most cells, including immune cells, produce TGF-β1 in a latent, inactive form, in which the mature TGF-β1 dimer is non-covalently associated with the latency-associated peptide (LAP) [3, 4]. Only a few cell types are able to activate the cytokine, by releasing mature TGF-β1 from LAP and allowing its binding to the TGF-β receptor. Dendritic cells and epithelial cells can activate latent TGF-β1 deposited in the extracellular matrix via binding of integrins αVβ8 or αVβ6, respectively, to RGD motifs in LAP [5, 6]. We and others showed that Tregs, B cells, and platelets activate latent TGF-β1 presented on their surface by a transmembrane protein called GARP [7,8,9].
Activation of TGF-β1 from GARP:(latent)TGF-β1 complexes on Tregs requires integrin αVβ8 [10]. We recently developed monoclonal antibodies against GARP:TGF-β1 complexes that block TGF-β1 activation and immunosuppression by human and mouse Tregs [11, 12]. We showed that anti-GARP:TGF-β1 mAbs overcome resistance to PD1/PD-L1 blockade and induce immune-mediated regressions of tumors in mice. In addition to blocking Treg immunosuppression and restoring anti-tumor immunity, anti-GARP:TGF-β1 mAbs could exert unwanted side effects, owing on one hand to their ability to block TGF-β1 activation from non-Treg GARP-expressing cells, and on the other hand to the pleiotropic functions exerted by TGF-β1 in immunity, including adaptive immunity. Notably but non exclusively, TGF-β1 is known to induce switch to IgA production in B cells, and differentiation of naïve CD4+ T cells into TH17 effectors in presence of IL-6 or into peripheral Tregs (pTregs) in presence of IL-2 [13,14,15]. TH17, pTregs and IgA-producing B cells are adaptive immune effectors playing important roles in the establishment and maintenance of balanced immune responses at epithelial barriers. The use of blocking anti-GARP:TGF-β1 mAbs for the purpose of cancer immunotherapy could therefore perturb immunity against bacterial infections in the intestine.
Citrobacter rodentium is a natural murine bacterial pathogen causing intestinal infection, inflammation, and disease that closely resembles disease caused by enteropathogenic Escherichia coli and enterohemorrhagic E. coli in humans. Oral gavage of C. rodentium in WT mice causes infection and inflammation limited to colon and caecum, which are rapidly controlled by the immune system, preventing severe intestinal disease [16, 17]. Production of IL-22 is required to protect the host against development of severe colitis [18]. In the early phase of infection, IL-22 is produced by innate immune cells such as group 3 innate lymphoid cells. The cytokine is crucial to limit bacterial expansion, notably by inducing production of RegIIIβ and RegIIIγ antimicrobial peptides by epithelial cells [19, 20]. In later phases, IL-22 is also produced by CD4+ T cells, including TH17 cells. In addition to TH17 cells, adaptive immune responses against C. rodentium, which are required to clear the infection [21, 22], also imply TH1 cells and B cells producing pathogen-specific IgGs.
Here, we examined whether anti-GARP:TGF-β1 mAbs could perturb innate or adaptive immune responses at mucosal barriers, using oral gavage of C. rodentium in WT or highly susceptible Il22r−/− mice as a model of intestinal bacterial infection. We also examined whether the absence of GARP:TGF-β1 complexes would alter T cell- or B cell- responses against protein immunization in mice carrying Treg-, B cell- or platelet-specific deletions of the Garp gene.
Methods
Mice
All mice were bred at the SPF animal facility of the UCLouvain. Cell type-specific Garp KOs and WT littermates were obtained by crossing Lrrc32tm1.1Hfuj mice with B6.129 (Cg)-Foxp3tm4(YFP/icre)Ayr/J, or Tg(Pf4-icre)Q3Rsko, or Cd79atm1(cre)Reth/EhobJ mice. Il22ra1−/− (Il22r−/−) mice were generated at the de Duve Institute [23]. Mice were maintained in an SPF animal facility at temperatures between 20 and 24 °C, HR between 40 and 65%, and day–night cycles of 12 h–12 h. All animal studies were performed in accordance with national and institutional guidelines for animal care, under permit number 2017/UCL/MD/019 from the UCLouvain.
Antibodies
Clone 58A2 is a monoclonal mouse IgG2a antibody that binds mouse GARP:TGF-β1 complexes and blocks active TGF-β1 production by mouse cells in vitro [12]. Three to four biweekly intra-peritoneal (i.p.) injections of 250 µg of 58A2 mAb in combination with anti-PD1 were previously shown to exert anti-tumor effects in tumor-bearing mice [12]. Here, mice received two weekly i.p. injections of 400 µg of 58A2. Clone 1D11 is a monoclonal mouse IgG1 antibody that neutralizes active TGF-β [1, 2, and 3] (BioXcell).
C. rodentium infections
C. rodentium strain DBS100 (kindly provided by M. Chamaillard, Pasteur Institute, Lille, France) was cultured overnight in LB media at 37 °C. Concentration of bacteria in the cultures was assessed by measuring absorbance at 600 nm and converting into colony-forming units (CFU). Inoculation of C. rodentium (109 CFU in 200 µl of PBS) was performed by oral gavage in 3-month-old mice. One day before infection and 6 days after, 400 µg of anti-GARP:TGF-β1 (clone 58A2) or anti-TGF-β (clone 1D11) mAbs were injected i.p.. Mice were monitored daily for weight change, and sacrificed at the time point indicated in the figures, or if weight loss was > 20% by comparison today 0.
Protein immunization
To measure Ig responses, 3-month-old mice were injected i.p. with 100 μg ovalbumin (OVA, Sigma) or 30 μg Cholera Toxin B subtype (CTB, Enzo Life Science) emulsified in 100 μl of Imject® Alum solution (Thermofisher) on day 0, and 100 μg OVA or 30 μg CTB in PBS on day 9. Mice were bled on day 16 to measure OVA- or CTB- specific Igs in the serum. As indicated in the figures and their legends, some mice received 400 µg of anti-GARP:TGF-β1 i.p. on day -1 and 6. To measure TH cell responses, 3-month-old mice were injected sub-cutaneously (s.c.) with 100 μg OVA emulsified in 100 μl of Complete Freund’s Adjuvant (CFA, Thermofisher) on day 0, then sacrificed to collect spleens on day 14.
Tissue collection and Histology
Colons were collected after sacrifice. Five mm-long terminal fragments were used for RT-qPCR analyses. For histological analyses, colons were placed in a Swiss roll shape, soaked in 10% formalin for 24 h then embedded into paraffin. 7 µm-sections were stained with hematoxylin and eosin. Histopathological scoring was adapted from previous reports [24, 25], by measuring lymphocyte infiltration, goblet cell- and crypt- damage, and colonic hyperplasia to attribute a colitis score (0: no colitis; 1: scattered inflammatory cells in the lamina propria, less than 25% of Goblet cell depletion, less than 25% of crypt thickness increase; 2: increased numbers of inflammatory cells in the lamina propria, less than 50% of Goblet cell depletion, less than 50% of crypt thickness increase 3: confluence of inflammatory cells extending into the submucosa, less than 75% of Goblet cell depletion, less than 75% of crypt thickness increase; 4: transmural extension of the infiltrative inflammatory cell severe colitis, 100% of Goblet cell depletion, 100% of crypt thickness increase).
Bacteria and CFU counts
Fresh fecal samples were collected, weighed, and homogenized in cold sterile PBS (1 ml/100 mg of feces). Bacterial DNA was extracted using QIAamp DNA Stool Mini Kit (Qiagen). Copy numbers of the C. rodentium Espb gene were measured by qPCR with the following primer set: 5′- CGTCAGCAGCCTTTTCAGCTA -3′, and 5′- ATGCCGCAGATGAGACAGTTG -3′ and in 20 µl reaction volumes containing Takyon Master Mix (Eurogentec) using StepOnePlus device (Thermofisher) with standard Thermal cycling parameters (95 °C for 3′; 50 cycles of 95 °C for 10’’ and 60 °C for 60″).
Livers were collected, weighed and homogenized, and titrated in PBS. Series of liver homogenate dilutions were spread on LB semi-solid culture medium and incubated at 37 ℃ overnight. Bacterial colonies were counted to determine CFUs and normalized to the weight of the livers.
Mixed lymphocyte cultures
15 days after immunization with OVA in CFA, spleens were collected and CD4+ T cells were sorted by MACS (Miltenyi Biotech) with anti-mouse CD4+ beads. 2 × 105 CD4+ cells were seeded with irradiated syngeneic adherent cells pulsed with OVA. Adherent cells were obtained by coating 1 × 106 splenocytes in a 96-well flat-bottomed plate for 1.5 h, then removing non-adherent cells by washing with PBS, and pulsed with OVA (50 µg/ml) for 2 h, before irradiation (30 Gy from a 137Cs source). After 96 h of mixed lymphocyte culture, supernatants were collected to measure cytokines.
RNA extraction and RT-qPCR
Colonic tissues were disrupted with the Tissue Lyser (Qiagen), total RNA was isolated using Nucleospin Mini Columns (Macherey Nagel), and reverse transcribed into cDNA (Thermofisher). qPCR was performed in a StepOnePlus device (Applied Biosystems) in 20 µl reaction volumes containing Takyon Master Mix (Eurogentec), cDNA, and primers. Thermal cycling parameters were either fast conditions (95 °C for 3′; 50 cycles of 95 °C for 3’’and 60 °C for 30’’) or standard conditions (95 °C for 3′; 50 cycles of 95 °C for 10’’ and 60 °C for 60’’) depending on the amplicon size. The b-actin gene (primers obtained from Eurogentec; forward strand: 5′-ATTGCCGACAGGATGCAGAA-3′; reverse strand: 5′-GTCATACTCCTGCTTGCTGA-3′; Taqman probe: 5′-TCAAGATCATTGCTCCTCCTGAGC-3′) was used to normalize relative gene expression. Primers were obtained from Eurogentec or IDT. The target genes included Il17a (forward: 5′-GCTCCAGAAGGCCCTCAG-3′; reverse: 5′-CTTTCCCTCCGCATTGACA-3′; Taqman probe: 5′-ACCTCAACCGTTCCACGTCACCCTG-3′), Ifng (forward: 5′-TCAAGTGGCATAGATGTGGAAGAA-3′; reverse: 5′-TGGCTCT GCAGGATTTTCATG-3′; Taqman probe: 5′-TCACCATCCTTTTGCCAGTTCCTCCAG-3′), RegIIIb (forward: 5′-CTACTGCCTTAGACCGTGCTTTC-3′; reverse: 5′-GAGTCTTCACATTTTGTCCCTTGTC-3′; Taqman probe: 5′-GTGAAGTTGCCCTATGTCTGC-3′), RegIIIg (forward: 5′-GAGTGGAGCAATGCTGATGTGATG-3′; reverse: 5′-GGGATCTTGCTTGTGGCTAGG -), Il6 (forward: 5′-CAGAGTCCTTCAGAGAGATACAGAAA-3′; reverse: 5′-TCCAGCTTATCTGTTAGGAGAGCATT-3′), Il4 (forward: 5′-GAACGAGGTCACAGGAGAAGG-3′; reverse: 5′-GGACTCATTCATGGTGCAGCTTA-3′; Taqman probe: 5′-CCTCACAGCAACGAAGAACACCACAG-3′) and Il22 (forward: 5′-GCTGCCCGTCAACACCC-3′; reverse: 5′-CTGATCCTTAGCACTGACTCCTC-3′; Taqman probe: 5′- TGAGGTGTCCAACTTCCAGCAGCCA-3′).
ELISA
Total serum IgG, IgM, and IgA were measured according to manufacturer instructions using IgG, IgM, and IgA ELISAs kits (Thermo Scientific). To measure C. rodentium- specific serum Igs, bacteria were lysed by sonication in PBS, C. rodentium proteins were enriched with bacterial protein extraction reagent (Thermo Scientific), then coated overnight at 4 °C (10 µg/ml, 100 µl) prior to incubation with various dilutions of mouse sera as indicated in the figures. Similarly, to measure OVA- and CTB- specific Igs, OVA (15 µg/ml, 100 µl) or CTB (4 µg/ml, 100 µl) were coated overnight at 4 °C on microtiter plates. C. rodentium-, OVA- or CTB- specific IgGs, IgMs, and IgAs were measured using detection antibodies from the IgG, IgM, and IgA ELISA kits. Cytokines in culture supernatants were also measured by ELISA (murine IFNγ ELISA, R&D Systems; murine IL-17a ELISA, with antibodies described in [26]). Absorbance readings were made at 450 nm, using a 96-well plate spectrophotometer with GloMax Discover (Promega).
Flow cytometry
Splenocytes were stained with antibodies against surface markers (CD4, B220, CD41, and GARP) in the presence of a viability dye (eBioscience) and anti-CD16/32 to block FcγRs using a standard protocol. Tregs were stained with anti-Foxp3 using the eBioscience™ FOXP3/Transcription Factor Staining Kit (Invitrogen). Analyses were performed on a FACS LSR Fortessa flow cytometer (DIVA, BD Biosciences) and data were computed using the FlowJo software (Tree Star).
Statistical analyses
Statistical analysis was performed with Prism 5 (Graphpad Software) using non-parametric tests (Mann–Whitney), One-way ANOVA (Bonferroni multiple comparison post-tests), and Log-rank Test for survival curves. P-value is shown if it is lower than 0.5.
Results
Anti-GARP:TGF-β1 mAbs do not aggravate intestinal disease caused by C. rodentium infection
Infection of wild-type C57BL/6 (WT) mice by oral gavage of C. rodentium is efficiently controlled by innate and adaptive immune responses, which prevent severe intestinal disease and weight loss [16, 17]. To determine whether TGF-β1 blockade could alter this control, we administered anti-GARP:TGF-β1, anti-TGF-β, or PBS one day before and six days after the oral gavage (Fig. 1a). Whereas the anti-GARP:TGF-β1 mAb (clone 58A2) blocks activation of latent TGF-β1 at the surface of GARP expressing cells such as Tregs [12], anti-TGF-β mAb (clone 1D11) neutralizes active TGF-β1, β2, and β3, whichever their cellular source. No obvious symptom and no weight loss were observed, and all mice survived in all groups, indicating that TGF-β signals are not required to prevent severe intestinal disease in WT mice (Fig. 1b and supplementary Fig. 1a).
Antibody-mediated blockade of TGF-β1 produced from GARP:TGF-β1 complexes does not aggravate intestinal disease induced by C. rodentium infection. a Schematic representation of the experimental design. Three-month-old C57BL/6 wild-type (WT B6) or Il22r−/− mice received i.p. injections of PBS, anti-GARP:TGF-β1 or anti-TGF-β mAbs 1 day before, and 6 days after oral gavage with C. rodentium (C.r). b-c Mice were monitored daily for weight loss. Data pooled from 2 to 3 independent experiments. Data points represent mean weight change per group ± sem. n = number of mice per group. Statistical analysis was performed by ANOVA with a Bonferroni post-test. d C. rodentium numbers were evaluated by quantification of espB gene copy number in the feces by qPCR. Each line represents values measured in one mouse. e C. rodentium CFUs in the livers collected 9 days after oral gavage. Each data point represents the value measured in one mouse. Statistical analysis was performed with a Mann–Whitney unpaired t-test. No statistically significant difference was observed between infected mice treated with PBS or anti-GARP:TGF-β1 (P > 0,05)
IL-22 signaling is crucial in the early phase of host defense against intestinal infection. In contrast to WT mice, Il22−/− and Il22r−/− mice are highly susceptible to C. rodentium infection, which causes severe epithelial damage in the intestine, weight loss, systemic bacterial burden, and high mortality in these mice [19, 27]. We thus tested whether TGF-β1 blockade with anti-GARP:TGF-β1 mAbs would increase the severity of disease in these mice. Mice receiving control PBS injections started to lose weight 8 days after infection and had lost 17 ± 8% (mean ± sem) of their initial weight by the end of the experiment on day 15 (Fig. 1c). Only 30% of the mice survived until the end of the experiment (supplementary Fig. 1b). Injections of anti-GARP:TGF-β1 mAbs did not exacerbate weight loss, which was even slightly, although not significantly, less pronounced than in PBS-injected mice (11% ± 8%). In line with this, more than 65% of mice receiving anti-GARP:TGF-β1 mAbs survived until the end of the experiment (supplementary Fig. 1b). Histological analyses of colons collected 9 days after gavage confirmed epithelial damage and inflammation, which were not more severe in mice that had received anti-GARP:TGF-β1 mAbs (supplementary Fig. 1c). We used qPCR to measure C. rodentium numbers in the feces at multiple time points after oral gavage (Fig. 1d). After an initial drop on day 2, C. rodentium numbers per gram of feces started to increase on day 3, to reach a maximum of 108–1010 on day 9. No significant difference was observed in mice receiving anti-GARP:TGF-β1 mAbs (Fig. 1d). We also measured C. rodentium CFU in liver homogenates, to evaluate systemic bacterial burden on day 9. No significant difference was observed in Il22r−/− mice that had received anti-GARP:TGF-β1 by comparison to PBS (Fig. 1e).
Taken together, these results indicate that anti-GARP:TGF-β1 mAbs do not reduce control of bacterial proliferation nor does it aggravate the severity of disease induced by C. rodentium infection in WT mice or in highly susceptible Il22r−/− mice.
Anti-GARP:TGF-β1 mAbs do not modify innate and adaptive immune responses to intestinal C. rodentium infection
Control and clearance of C. rodentium infection require both innate and adaptive immune responses [16, 28]. We tested whether anti-GARP:TGF-β1 mAbs could alter these responses in the intestines of highly susceptible Il22r−/− mice. Mice received C. rodentium by oral gavage on day 0, and i.p. injections of anti-GARP:TGF-β1 or PBS on days -1 and + 6. Weights were measured daily (Fig. 2a), and sera and colons were collected 9 days after gavage.
Antibody-mediated blockade of TGF-β1 produced from GARP:TGF-β1 complexes do not impair innate or adaptive immune responses against intestinal C. rodentium infection. Three-month-old Il22r−/− mice received i.p. injections of PBS or anti-GARP:TGF-β1 mAbs 1 day before, and 6 days after oral gavage with C. rodentium. Mice were monitored daily for weight loss and sacrificed on day 9, to collect colons and sera. a Weight change in individual mice. Each line represents one mouse, with individual mouse ID numbers indicated next to the corresponding line. b-c Expression of the indicated genes, normalized to b-actin expression, as measured by RT-qPCR in colon samples. d C. rodentium-specific IgM, IgG, and IgA, as measured in 1/100 dilutions of serum samples by ELISA. Data points show mean value (technical duplicates) in each individual mouse (mouse ID number is indicated within each data point). Horizontal bars represent mean ± sem per group. Data is representative of three independent experiments. Statistical analysis was performed with a Mann–Whitney unpaired t-test. No statistically significant difference was observed between infected mice treated with PBS or anti-GARP:TGF-β1 (P > 0,05)
We first measured intestinal levels of mRNAs encoding molecules implicated in innate responses. High susceptibility to C. rodentium in absence of IL-22 signaling occurs mostly because IL-22 is required to induce expression of antimicrobial peptides RegIIIβ and RegIIIγ in colonic epithelial cells [19]. Accordingly, we observed that RegIIIb and RegIIIg mRNAs were induced in the intestines of infected Il22r−/− mice by comparison to non-infected mice, but to levels ± 10–100 times lower than in infected WT mice (Fig. 2b and supplementary Fig. 2). Nevertheless, anti-GARP:TGF-β1 mAbs did not reduce RegIIIb and RegIIIg expression in infected Il22r−/− or WT mice (Fig. 2b, supplementary Fig. 2 and data not shown). Similar results were observed for expression of Il6 and Il22 itself, taken here as representative of innate immune responses (Fig. 2b).
We next measured intestinal expression of mRNAs encoding CD3ε and cytokines produced by helper T (TH) cells. As expected, expression of Cd3e, Ifng, and Il17a was clearly induced by comparison to non-infected mice, whereas that of Il4 was not. Here again, anti-GARP:TGF-β1 mAbs did not significantly reduce expression of any of these T cell marker or TH cell-derived cytokines by comparison to control PBS injections (Fig. 2c). Finally, we measured C. rodentium-specific IgM, IgG and IgA in 1/100 dilutions of sera by ELISA. Most mice had induced high levels of C. rodentium-specific IgM, IgG, and IgA, whether or not they had received anti-GARP:TGF-β1 mAbs (Fig. 2d). Interestingly, two mice that had received anti-GARP:TGF-β1 (mice 5 and 6) did not develop strong IgM, IgG, and IgA responses against the bacteria. They correspond to mice that did not develop severe colitis and weight loss (Fig. 2a) and showed only very minor inductions of TH1 and TH17 cytokine genes in the colons (Fig. 2c). Thus, they appear to correspond to mice that did not develop significant infection and consequent immune responses upon oral gavage with C. rodentium.
Taken together, these results indicate that neither innate nor adaptive immune responses against C. rodentium in highly susceptible Il22r−/− mice are altered by anti-GARP:TGF-β1 mAbs. If anything, anti-GARP:TGF-β1 mAbs tend to protect Il22r−/− mice against severe intestinal disease and mortality induced by C. rodentium infection, although differences by comparison to PBS controls were not always statistically significant (Fig. 1c, supplementary Fig. 1b, and Fig. 2a).
Anti-GARP:TGF-β1 mAbs do not alter production of antigen-specific IgM, IgG, or IgA following protein immunization
Our group previously reported that blocking anti-GARP:TGF-β1 mAbs impaired switch to IgA production in human B cells stimulated in vitro [9]. We thus sought to determine whether TGF-β1 production from GARP:TGF-β1 complexes could regulate Ig production and isotype switching in non-infectious immunization models that induce strong Ig responses in mice. We primed WT B6 mice with ovalbumin (OVA) in alum and boosted them in PBS on day 9. Mice also received PBS or anti-GARP:TGF-β1 injections 1 day before and 6 days after priming (Fig. 3a). Immunization induced abundant anti-OVA IgM, IgG, and IgA, none of which were reduced by anti-GARP:TGF-β1 mAbs (Fig. 3b-c).
Antibody-mediated blockade of TGF-β1 produced from GARP:TGF-β1 complexes does not modify the amplitude of OVA-specific Ab responses upon immunization with OVA and alum. a Schematic representation of the experimental design. Three-month-old C57BL/6 mice were treated with mAbs 1 day before and 6 after i.p. OVA protein immunization with alum. After 9 days, OVA protein in PBS was injected i.p. as boost. Blood was collected on day 16 to measure OVA-specific Igs in sera by ELISA. b-c Data points represent values in individual mice. Horizontal lines indicate mean ± sem (n = 6 mice per group). Statistical analysis was performed with a Mann–Whitney unpaired t-test. No statistically significant difference was observed between OVA-immunized mice treated with PBS or anti-GARP:TGF-β1 (P > 0,05). Results shown are representative of two independent experiments
Genetic deletion of Garp in Tregs, B cells, or platelets does not modify production of antigen-specific IgM, IgG, or IgA following protein immunization
To exclude cell-type-restricted effects of GARP:TGF-β1 blockade, we performed protein immunizations in mice carrying a Treg-, B cell- or platelet-specific deletion of the Garp gene. Complete and specific Cre-mediated deletion of Garp in the expected cell type is observed in each of the three mouse strains, namely Foxp3Cre x Garpfl/fl, Mb1Cre x Garpfl/fl, and Pf4Cre x Garpfl/fl mice (supplementary Fig. 3a). All cell-type-specific knock-out (KO) mice have serum levels of various Ig isotypes that are similar to those found in the corresponding WT littermates (Supplementary Fig. 3b). Treg-specific Garp KOs and WT littermates were immunized with OVA in alum as above. Immunization induced similar levels of anti-OVA IgM, IgG, and IgA in WT and KOs (supplementary Fig. 4). We also used another antigen, cholera toxin B (CTB), to immunize Treg- and other cell type-specific Garp KOs and WT littermates (Fig. 4a). CTB in alum is also known to induce high levels of antigen-specific IgM, IgG, and IgA [29, 30]. We confirmed that the absence of GARP on Tregs did not modify levels of anti-CTB IgM, IgG, and IgA in serum (Fig. 4b-c). Mb1Cre x Garpfl/fl and Pf4Cre x Garpfl/fl mice and their WT littermates were also immunized with CTB in alum and levels of serum anti-CTB IgM, IgG and IgA 16 days after priming were similar in B cell- and platelet- Garp KOs by comparison to their corresponding WT littermates (Fig. 4b-c). A trend towards slightly reduced anti-CTB IgM was observed in B cell-Garp KOs, but this difference was not statistically significant (Fig. 4c).
Genetic deletion of Garp in Tregs, B cells, or platelets does not modify CTB-specific Ig responses upon CTB immunization. a Schematic representation of the experimental design. Genetically modified C57BL/6 mice (3-month-old) were injected i.p. with CTB in alum on day 0, and CTB in PBS on day 9. Blood was collected on day 16 to measure CTB specific-Igs in serum by ELISA. b-d Data points represent values in individual mice. Horizontal lines show mean ± sem (n = 5–6 mice per group). Statistical analysis was performed with a Mann–Whitney unpaired t-test (to compare groups of CTB-immunized mice treated with PBS or anti-GARP:TGF-β1) and p-value is shown if it is lower than 0.5
Genetic deletion of Garp in Tregs, B cells, or platelets does not impair OVA-specific TH responses following OVA immunization
We examined whether TH cell differentiation is altered in cell type-specific Garp KOs upon protein immunization. Garp KOs and their WT littermates were immunized with OVA in Complete Freund’s Adjuvant (CFA). CFA is known to favor potent TH response and notably TH17 responses [31], which could be impaired if TGF-β activation is reduced. Fourteen days after immunization, splenocytes were collected and re-stimulated in vitro with APCs pulsed with OVA to measure IL-4, IFNγ, and IL-17a production in the supernatants (Fig. 5a). Splenocytes from all mice immunized with OVA produced abundant IFNγ and IL-17a, but no IL-4. Importantly, no difference was observed between cell-type-specific Garp KOs and their corresponding WT littermates (Fig. 5b-d).
Genetic deletion of GARP in Tregs, B cells, or platelets does not modify OVA-specific TH responses upon immunization with OVA and CFA. a Schematic representation of the experimental design. Genetically modified C57BL/6 mice (3-month-old) were injected s.c. with OVA protein and CFA on day 0. B–c 14 days after OVA-CFA immunization, spleen cells were collected and CD4+ cells were purified by MACS before incubation with adherent stimulating cells pulsed with OVA. After 4 days of co-culture, IFNγ and IL-17a production were measured by ELISA. Data in all panels are means ± sem (n = 5–6 mice per group) and are representative of two to three independent experiments Statistical analysis was performed with Mann–Whitney unpaired t-test (to compare the groups of CTB-immunized mice treated with PBS or anti-GARP:TGF-β1) and p-value is shown if it is lower than 0.5
Altogether, our results indicate that TGF-β1 production from GARP:TGF-β1 complexes on Tregs, B cells, or platelets does not significantly impact antibody production and TH cell differentiation following immunization with protein in vivo.
Discussion
Our observations suggest that anti-GARP:TGF-β1 mAbs do not alter innate or adaptive immune responses against C. rodentium infection in mice. This may be considered reassuring with regards to the risk of increased susceptibility to intestinal infection and inflammation that could be associated with the use of anti-GARP:TGF-β1 mAbs for cancer immunotherapy. It also suggests that TGF-β1 derived from GARP-expressing cells does not play important role in regulating immune responses to bacterial infections at the level of mucosal barriers.
Zhang et al. reported that C. rodentium infection downregulates expression of TGF-β receptor chains I and II and of Smad2 in mouse colons [32]. They suggested that these downregulations promote inflammation and contribute to disease pathogenesis. Their observations could explain the absence of effect of anti-GARP:TGF-β1 mAbs observed here in mice infected with C rodentium if TGF-β1 signaling was already inhibited by the pathogen and did not participate in the immune responses.
Host defense against C. rodentium also involves adaptive TH17 responses [28]. TH17 differentiation depends on IL-23 and TGF-β1. IL-23-deficient (p19−/−) mice treated with anti-TGF-β1 mAbs developed severe colitis associated with a strong decrease of TH17 cells [33]. Backert et al. confirmed this observation with a TGF-β inhibitor in STAT3-deficient mice highly susceptible to C. rodentium infection [34]. Interestingly, we observed that anti-GARP:TGF-β1 mAbs did not alter Il17a mRNA expression in the colons of C. rodentium-infected Il22r−/− mice, suggesting that active TGF-β1 released from GARP:TGF-β1 complex does not contribute to TH17 differentiation in this setting.
B cells and production of C. rodentium-specific IgGs are also required for complete clearance of C. rodentium [22]. Following C. rodentium infection, Il22r−/− mice produced specific IgG, IgM, and IgA, and this production was not altered by administration of anti-GARP:TGF-β1 mAbs. This observation was unexpected. Indeed, we previously showed that blocking anti-GARP:TGF-β1 mAbs hampered isotype switching towards IgA by human B cells in vitro [9], suggesting that B cells could produce themselves the active TGF-β1 required for IgA secretion [15, 35]. However, our data here in mice showed that anti-GARP:TGF-β1 mAbs did not impede the anti-OVA IgA response in vivo. Moreover, anti-CTB IgA response was not impeded in any of the cell type-specific Garp KOs used, including B cell-specific Garp KO. Altogether, these results suggest that the active TGF-β1 required for IgA switching does not emanate from GARP-expressing cells, including B cells. This could be true when IgA switching occurs in vivo, upon immunization of mice with protein antigens. In our previous report using purified human B cells in vitro, IgA switching was observed after BCR stimulation with anti-IgM in the presence of CpG, anti-CD40L, and IL-21, but in the absence of any other cell types. In such experimental conditions in vitro, GARP-expressing human B cells may become a unique, predominant source of active TGF-β1 allowing IgA switching, even though they may not significantly contribute to switching in vivo.
Anti-GARP:TGF-β1 mAbs were shown to inhibit immunosuppression by human and mouse Tregs in vivo [11, 12]. Here, we observe no obvious impact of these mAbs in a model of bacterial intestinal infection in mice. We thus suggest that anti-GARP:TGF-β1 mAbs could be used to inhibit immunosuppression by Tregs in patients with cancer, without major risks of impairing immune responses to bacterial infection at mucosal barriers.
References
Shull MM, Ormsby I, Kier AB et al (1992) Targeted disruption of the mouse transforming growth factor-beta 1 gene results in multifocal inflammatory disease. Nature 359:693–699. https://doi.org/10.1038/359693a0
Kulkarni AB, Huh CG, Becker D et al (1993) Transforming growth factor beta 1 null mutation in mice causes excessive inflammatory response and early death. Proc Natl Acad Sci U S A 90:770–774. https://doi.org/10.1073/pnas.90.2.770
Shi M, Zhu J, Wang R, Chen X, Mi L, Walz T, Springer TA (2011) Latent TGF-beta structure and activation. Nature 474:343–349. https://doi.org/10.1038/nature10152
Lienart S, Merceron R, Vanderaa C et al (2018) Structural basis of latent TGF-beta1 presentation and activation by GARP on human regulatory T cells. Science 362:952–956. https://doi.org/10.1126/science.aau2909
Munger JS, Huang X, Kawakatsu H et al (1999) The integrin alpha v beta 6 binds and activates latent TGF beta 1: a mechanism for regulating pulmonary inflammation and fibrosis. Cell 96:319–328. https://doi.org/10.1016/s0092-8674(00)80545-0
Travis MA, Reizis B, Melton AC et al (2007) Loss of integrin alpha(v)beta8 on dendritic cells causes autoimmunity and colitis in mice. Nature 449:361–365. https://doi.org/10.1038/nature06110
Tran DQ, Andersson J, Wang R, Ramsey H, Unutmaz D, Shevach EM (2009) GARP (LRRC32) is essential for the surface expression of latent TGF-beta on platelets and activated FOXP3+ regulatory T cells. Proc Natl Acad Sci U S A 106:13445–13450. https://doi.org/10.1073/pnas.0901944106
Stockis J, Colau D, Coulie PG, Lucas S (2009) Membrane protein GARP is a receptor for latent TGF-beta on the surface of activated human Treg. Eur J Immunol 39:3315–3322. https://doi.org/10.1002/eji.200939684
Dedobbeleer O, Stockis J, van der Woning B, Coulie PG, Lucas S (2017) Cutting edge: active TGF-beta1 released from GARP/TGF-beta1 complexes on the surface of stimulated Human B Lymphocytes Increases class-switch recombination and production of IgA. J Immunol 199:391–396. https://doi.org/10.4049/jimmunol.1601882
Stockis J, Lienart S, Colau D, Collignon A, Nishimura SL, Sheppard D, Coulie PG, Lucas S (2017) Blocking immunosuppression by human Tregs in vivo with antibodies targeting integrin alphaVbeta8. Proc Natl Acad Sci U S A 114:E10161–E10168. https://doi.org/10.1073/pnas.1710680114
Cuende J, Lienart S, Dedobbeleer O et al. (2015) Monoclonal antibodies against GARP/TGF-beta1 complexes inhibit the immunosuppressive activity of human regulatory T cells in vivo. Sci Transl Med 7:284ra56. https://doi.org/10.1126/scitranslmed.aaa1983
de Streel G, Bertrand C, Chalon N et al (2020) Selective inhibition of TGF-beta1 produced by GARP-expressing Tregs overcomes resistance to PD-1/PD-L1 blockade in cancer. Nat Commun 11:4545. https://doi.org/10.1038/s41467-020-17811-3
Li MO, Wan YY, Flavell RA (2007) T cell-produced transforming growth factor-beta1 controls T cell tolerance and regulates Th1- and Th17-cell differentiation. Immunity 26:579–591. https://doi.org/10.1016/j.immuni.2007.03.014
Edwards JP, Fujii H, Zhou AX, Creemers J, Unutmaz D, Shevach EM (2013) Regulation of the expression of GARP/latent TGF-beta1 complexes on mouse T cells and their role in regulatory T cell and Th17 differentiation. J Immunol 190:5506–5515. https://doi.org/10.4049/jimmunol.1300199
Cazac BB, Roes J (2000) TGF-beta receptor controls B cell responsiveness and induction of IgA in vivo. Immunity 13:443–451. https://doi.org/10.1016/s1074-7613(00)00044-3
Silberger DJ, Zindl CL, Weaver CT (2017) Citrobacter rodentium: a model enteropathogen for understanding the interplay of innate and adaptive components of type 3 immunity. Mucosal Immunol 10:1108–1117. https://doi.org/10.1038/mi.2017.47
Mundy R, MacDonald TT, Dougan G, Frankel G, Wiles S (2005) Citrobacter rodentium of mice and man. Cell Microbiol 7:1697–1706. https://doi.org/10.1111/j.1462-5822.2005.00625.x
Basu R, O’Quinn DB, Silberger DJ, Schoeb TR, Fouser L, Ouyang W, Hatton RD, Weaver CT (2012) Th22 cells are an important source of IL-22 for host protection against enteropathogenic bacteria. Immunity 37:1061–1075. https://doi.org/10.1016/j.immuni.2012.08.024
Zheng Y, Valdez PA, Danilenko DM et al (2008) Interleukin-22 mediates early host defense against attaching and effacing bacterial pathogens. Nat Med 14:282–289. https://doi.org/10.1038/nm1720
Satoh-Takayama N, Vosshenrich CA, Lesjean-Pottier S et al (2008) Microbial flora drives interleukin 22 production in intestinal NKp46+ cells that provide innate mucosal immune defense. Immunity 29:958–970. https://doi.org/10.1016/j.immuni.2008.11.001
Bry L, Brenner MB (2004) Critical role of T cell-dependent serum antibody, but not the gut-associated lymphoid tissue, for surviving acute mucosal infection with Citrobacter rodentium, an attaching and effacing pathogen. J Immunol 172:433–441. https://doi.org/10.4049/jimmunol.172.1.433
Maaser C, Housley MP, Iimura M et al (2004) Clearance of Citrobacter rodentium requires B cells but not secretory immunoglobulin A (IgA) or IgM antibodies. Infect Immun 72:3315–3324. https://doi.org/10.1128/IAI.72.6.3315-3324.2004
Van Belle AB, Cochez PM, de Heusch M et al (2019) IL-24 contributes to skin inflammation in Para-Phenylenediamine-induced contact hypersensitivity. Sci Rep 9:1852. https://doi.org/10.1038/s41598-018-38156-4
Cevallos SA, Lee JY, Tiffany CR, Byndloss AJ, Johnston L, Byndloss MX, Baumler AJ (2019) Increased Epithelial Oxygenation Links Colitis to an Expansion of Tumorigenic Bacteria. mBio. 10. https://doi.org/10.1128/mBio.02244-19
Chen CC, Louie S, McCormick B, Walker WA, Shi HN (2005) Concurrent infection with an intestinal helminth parasite impairs host resistance to enteric Citrobacter rodentium and enhances Citrobacter-induced colitis in mice. Infect Immun 73:5468–5481. https://doi.org/10.1128/IAI.73.9.5468-5481.2005
Uyttenhove C, Van Snick J (2006) Development of an anti-IL-17A auto-vaccine that prevents experimental auto-immune encephalomyelitis. Eur J Immunol 36:2868–2874. https://doi.org/10.1002/eji.200636662
Michiels C, Puigdevall L, Cochez P, Achouri Y, Cheou P, Hendrickx E, Dauguet N, Blanchetot C, Dumoutier L (2021) A targetable, noncanonical signal transducer and activator of transcription 3 activation induced by the Y-Less region of IL-22 receptor orchestrates imiquimod-induced psoriasis-like dermatitis in mice. J Invest Dermatol. https://doi.org/10.1016/j.jid.2021.04.016
Collins JW, Keeney KM, Crepin VF, Rathinam VA, Fitzgerald KA, Finlay BB, Frankel G (2014) Citrobacter rodentium: infection, inflammation and the microbiota. Nat Rev Microbiol 12:612–623. https://doi.org/10.1038/nrmicro3315
Marinaro M, Staats HF, Hiroi T et al (1995) Mucosal adjuvant effect of cholera toxin in mice results from induction of T helper 2 (Th2) cells and IL-4. J Immunol 155:4621–4629
Lycke N (1997) The mechanism of cholera toxin adjuvanticity. Res Immunol 148:504–520. https://doi.org/10.1016/s0923-2494(98)80144-2
Brunner R, Jensen-Jarolim E, Pali-Scholl I (2010) The ABC of clinical and experimental adjuvants–a brief overview. Immunol Lett 128:29–35. https://doi.org/10.1016/j.imlet.2009.10.005
Zhang YG, Singhal M, Lin Z et al (2018) Infection with enteric pathogens Salmonella typhimurium and Citrobacter rodentium modulate TGF-beta/Smad signaling pathways in the intestine. Gut Microbes 9:326–337. https://doi.org/10.1080/19490976.2018.1429878
Mangan PR, Harrington LE, O’Quinn DB et al (2006) Transforming growth factor-beta induces development of the T(H)17 lineage. Nature 441:231–234. https://doi.org/10.1038/nature04754
Backert I, Koralov SB, Wirtz S et al (2014) STAT3 activation in Th17 and Th22 cells controls IL-22-mediated epithelial host defense during infectious colitis. J Immunol 193:3779–3791. https://doi.org/10.4049/jimmunol.1303076
Klein J, Ju W, Heyer J et al (2006) B cell-specific deficiency for Smad2 in vivo leads to defects in TGF-beta-directed IgA switching and changes in B cell fate. J Immunol 176:2389–2396. https://doi.org/10.4049/jimmunol.176.4.2389
Acknowledgments
We thank E. Hemelrike for editorial assistance.
Funding
This work was supported by grants from the Fondation contre le Cancer (Grant F/2016/837), from the European Research Council (ERC) under the European Union's Horizon 2020 research and innovation programme (Grant TARG-SUP 682818), from the Actions de Recherche Concertées (Grant 14/19-056), from the Fonds National de la Recherche Scientifique (PDR Number T.0089.16) and from Région Wallonne (program WALinnov, project IMMUCAN, convention number 1610119). Xuhao Zhang was supported by a grant from the China Scholarship Council. This work was supported by grants from Walloon Excellence in Life Sciences and Biotechnology (WELBIO), Wavre, Belgium (CR-2019A-02.).
Author information
Authors and Affiliations
Contributions
Sophie Lucas conceived the study. Mélanie Gaignage, Xuhao Zhang, Julie Stockis, Olivier Dedobbeleer, Camille Michiels, Perrine Cochez, Laure Dumoutier and Sophie Lucas analyzed the data. Sophie Lucas, Pierre G. Coulie and Mélanie Gaignage wrote the manuscript. Mélanie Gaignage, Xuhao Zhang, Julie Stockis, and Camille Michiels performed experiments.
Corresponding author
Ethics declarations
Conflict of interest
Patents pertaining to blocking antibodies against human GARP:TGF-b1 have been filed under the Patent Cooperation Treaty (International application Number PCT/IB2019/053753), with Sophie Lucas, Pierre G. Coulie, and Laure Dumoutier as inventors and UCLouvain as applicant. The anti-mouse GARP:TGF-b1 antibody (clone 58A2) used herein is a surrogate for these antibodies. All other authors declare no competing interests.
Ethics approval
All mice were bred at the SPF animal facility of the UCLouvain. C. rodentium infection and immunization studies were performed in accordance with national and institutional guidelines for animal care, under permit number 2017/UCL/MD/019 from the UCLouvain.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gaignage, M., Zhang, X., Stockis, J. et al. Blocking GARP-mediated activation of TGF-β1 did not alter innate or adaptive immune responses to bacterial infection or protein immunization in mice. Cancer Immunol Immunother 71, 1851–1862 (2022). https://doi.org/10.1007/s00262-021-03119-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-021-03119-8








