Abstract
We report on the immunogenicity and clinical effects in a phase I/II dose escalation trial of a DNA fusion vaccine in patients with prostate cancer. The vaccine encodes a domain (DOM) from fragment C of tetanus toxin linked to an HLA-A2-binding epitope from prostate-specific membrane antigen (PSMA), PSMA27–35. We evaluated the effect of intramuscular vaccination without or with electroporation (EP) on vaccine potency. Thirty-two HLA-A2+ patients were vaccinated and monitored for immune and clinical responses for a follow-up period of 72 weeks. At week 24, cross-over to the immunologically more effective delivery modality was permitted; this was shown to be with EP based on early antibody data, and subsequently, 13/15 patients crossed to the +EP arm. Thirty-two HLA-A2− control patients were assessed for time to next treatment and overall survival. Vaccination was safe and well tolerated. The vaccine induced DOM-specific CD4+ and PSMA27-specific CD8+ T cells, which were detectable at significant levels above baseline at the end of the study (p = 0.0223 and p = 0.00248, respectively). Of 30 patients, 29 had a measurable CD4+ T-cell response and PSMA27-specific CD8+ T cells were detected in 16/30 patients, with or without EP. At week 24, before cross-over, both delivery methods led to increased CD4+ and CD8+ vaccine-specific T cells with a trend to a greater effect with EP. PSA doubling time increased significantly from 11.97 months pre-treatment to 16.82 months over the 72-week follow-up (p = 0.0417), with no clear differential effect of EP. The high frequency of immunological responses to DOM-PSMA27 vaccination and the clinical effects are sufficiently promising to warrant further, randomized testing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Activating immunity against cancer in patients has been a difficult goal [1] but randomized studies are now showing encouraging results in solid tumors [2, 3], including prostate cancer [4]. Prostate cancer immunotherapy is attractive at early biochemical detection of recurrence since rising prostate-specific antigen (PSA), even without radiologically measurable disease, identifies patients at risk who have very small volume disease [5]. Vaccine targets, like Muc-1 [6], PSA [7, 8], prostatic acid phosphatase (PAP) [9] or prostate-specific membrane antigen (PSMA) [10–12], have been identified as promising targets [13]. A randomized phase III trial showed that prostate-associated antigens can be effectively targeted by vaccination [4]. The improved median survival of 4.1 months in late-stage disease was not mirrored by PSA changes [4], an observation also made in other immunotherapy studies [14]. Although Sipuleucel-T sets a treatment paradigm, producing a new patient-specific vaccine is a technical, financial and logistical challenge. Overall benefit remains small, indicating an unmet clinical need for better, ideally non-toxic, treatments to improve outcomes [13].
Vaccination against cancer using exogenous peptide has been tested widely and may confer clinical effect in some settings [15–17]. However, CD8+ T-cell responses following vaccination using exogenous short peptides appear transient [18] possibly due to the lack of T-cell help. Viral vector–based vaccines may overcome this problem and have shown promise in metastatic disease [8, 19] with effects also on PSA doubling time (PSA-DT) at biochemical failure [6]. However, viral vectors will either face pre-existing immunity or induce it on repeat injections. DNA vaccines avoid this problem and offer a novel delivery vehicle for the induction of peptide-specific responses.
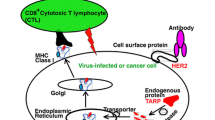
We have designed DNA fusion-gene vaccines able to deliver tumor-derived peptides, together with microbial genes, to generate high levels of T-cell help [20]. Our platform design includes a strongly immunogenic helper domain (DOM), derived from fragment C (FrC) of tetanus toxin, linked to a tumor-epitope sequence of choice [20]. In pre-clinical models, DOM-epitope vaccines induce durable tolerance-breaking epitope-specific CD8+ T-cell immunity, able to suppress a range of tumors [20].
In mice expressing the HLA-A0201* transgene, the DOM-epitope vaccine design incorporating an epitope from PSMA (PSMA27 VLAGGFFLL) [20, 21] induced high levels of specific CD8+ T cells able to kill tumor cells [22]. We have now vaccinated patients with biochemically recurrent prostate cancer and, to optimize human translation, also evaluated delivery with electroporation (EP). EP has been reported to increase the potency of DNA vaccines by increasing antigen levels and stimulating local inflammation [23], and its use is rapidly expanding in both infectious diseases and cancer vaccination. We found that this approach was safe, well tolerated and significantly increased antibody induction [24].
We report here the effect of our DOM-epitope vaccine on T-cell immunity and clinical outcome. The vaccine reproducibly induces T-cell immunity to PSMA27 and significantly increases PSA-DT, and in spite of the small sample size, we identified a trend to increased time to next treatment compared to a control group of unvaccinated HLA-A2− patients. Taken together, these data support further randomized testing of the vaccine.
Patients and methods
Patient population and regulatory information
Patients with biochemically recurrent prostate cancer, rising PSA (<50 ng/mL, PSA-DT >3 months) without radiological evidence of distant disease by CT scan, bone scan and/or MRI were eligible. Pelvic nodal enlargement up to 2 cm was allowed. Tumor PSMA expression was confirmed immunohistochemically at Southampton Cellular Pathology Laboratory. Other inclusion and exclusion criteria have been reported previously [24]. Patients were HLA-typed in NHS laboratories. The vaccine encodes an HLA-A2-restricted epitope; only HLA-A2+ patients were vaccinated. HLA-A2− patients who fulfilled all other entry criteria formed the control group and were followed for the evaluation of time to next treatment and survival only.
Regulatory approval for the study was given by the UK Medicines and Healthcare Regulatory Authority (MHRA), the Gene Therapy Advisory Committee and local Research Ethics committees. The study was registered in the database of gene therapy trials in the UK. All patients gave written informed consent to participate in the study between March 2005 and February 2008 at the University Hospitals Southampton and the Royal Marsden Hospital.
Study design
The study was a phase I/II, open-label, non-randomized, two-center, dose escalation study. DOM-PSMA27 vaccine [20, 22, 24] was injected into the thigh muscle 5 times at 0, 4, 8, 24 and 48 weeks. HLA-A2+ patients were recruited to two study arms (Fig. 1). In arm I, patients received DNA intramuscularly (i.m.), and in arm II, vaccine was delivered i.m. with EP using an Elgen Twinjector device [25] as described [24]. In each arm, the dose was escalated, with 5 patients per group: in arm I (without EP)—level 1: 800 μg, level 2: 1,600 μg, level 3: 3,200 μg per dose and in arm II (with EP)—level 1: 400 μg, level 2: 800 μg, level 3: 1,600 μg. If in the absence of safety concerns the immunological data supported this, patients were allowed to cross over between arms of the study after the first 3 vaccinations and receive the dose of the matched level in the opposite arm.
Follow-up on study was at weeks 0, 2 and 4 following vaccination, monthly to week 32 and then 2 monthly to week 72. At each visit, PSA levels were measured. For safety evaluation, full blood counts, clotting, serum biochemistry, LDH (lactate dehydrogenase), CK (creatine kinase) and autoimmune profiles of serum were monitored. PBMC were stored in liquid nitrogen for immunological assessment.
Clinical follow-up
PSA values were available up to the date of consent, and during the 72-week study follow-up for the vaccinated cohort; ethical permission to collect time-point-matched PSA values for the unvaccinated patients was not obtained. PSA values used to calculate the PSA-DT were evaluated by a study-independent, blinded reviewer. Using only evaluable PSA values, PSA-DT was calculated using an algorithm calculator (http://mskcc.org/applications/nomograms/prostate/PsaDoublingTime.aspx). PSA-DT was calculated for each patient for the period pre-study, for 6-month periods on study and for the overall 72-week study period (calculated up to week 72 or until treatment). Time to next treatment and survival (assessed up to 31/12/2010) were recorded for all patients.
Immunological evaluations
MIATA (Minimal Information About T-cell Assays; http://www.miataproject.org) guidelines were used to report immunological data on T-cell responses [26, 27] (Online Resource 1). PBMC were isolated from heparinized blood samples collected at each study visit. Recovery and viability were calculated using a manual hemocytometer and trypan blue exclusion. PBMC were cryopreserved and stored in LN2 vapor phase (Section 1, Online Resource 1). PBMC were assessed for immunological responses using assays validated to GCP for laboratories, and laboratory compliance was verified by external audit [28].
ELISPOT
PBMC from all follow-up time-points from each patient were assessed for IFNγ production in response to stimulation with recombinant FrC protein (20 μg/mL) [28] or PSMA27 (VLAGGFFLL) peptide (10 μg/mL, Protein Peptide Research, UK). The validated ELISPOT method used is described in detail in Section 2, Online Resource 1.
Cultured ELISPOT
PSMA27-specific CD8+ T cells were cultured in vitro for 8 days. As cell number was limiting, samples from different time-points were pooled and cultured in the following groups: baseline, weeks 8, 10 and 12, weeks 16, 20 and 24, weeks 26, 28 and 32 and weeks 50, 52 and 60. Cells were cultured with 10 μg/mL PSMA27 peptide or with a pool of viral peptides or a control peptide, HIV. IL-2 was added on days 3 and 6 and cells were harvested, washed and rested overnight on day 8. Following re-stimulation with 10 μg/mL peptide, IFNγ production was measured by ELISPOT. Full details are provided in Section 2, Online Resource 1.
Statistical analysis
Median values are presented throughout, where appropriate with 25 and 75 % interquartile box with ranges. Significance was determined by either a two-sided, nonparametric Wilcoxon signed rank test or a Mann–Whitney test. A value of p < 0.05 was considered significant.
Results
Patient demographics
Sixty-four patients were eligible for the study (Fig. 1; Table 1). Thirty-two HLA-A2+ patients were vaccinated and 32 HLA-A2− patients formed the control group for clinical follow-up. Two patients with adverse events (AE) after two vaccinations were replaced per study protocol and included in the safety but not in the immunological analyses (Fig. 1). One patient received three vaccinations before disease progression and commenced androgen suppression but remained evaluable for immune responses. After the initial 3 vaccinations with either DNA or DNA + EP, all but 4 patients went on to receive booster vaccines with EP (weeks 24 and 48). Twenty-nine patients completed vaccination and 72-week study follow-up (Fig. 1).
Safety and adverse events
Safety evaluation in the first two dose groups has been reported [24]. Full data for all patients on the study and a summary of AEs recorded are listed in Online Resource 2. The vaccine was safe and well tolerated. Most AEs were grade 1 or 2 and ranged from injection site reactions to flu-like symptoms, back pain and nail changes. Vaccination was discontinued due to AEs in two patients: one experienced grade 3 worsening of a pre-existing psoriasis, with causality assessed as likely vaccine related, and a second grade 3 AE was identified as worsening of pre-existing Parkinson’s disease, assessed as unlikely to be vaccine related. Two serious AEs were observed: one patient developed grade 2 peripheral edema and a second was admitted for a TURP. Both events resolved fully and the patients continued on study with no recurrence.
Previously, we reported the safety of EP in dose groups 1 and 2 by the measurement of muscle damage markers CK and LDH [24]. Patients in dose group 3 showed no increase (>twofold baseline) in either CK or LDH, and any increase observed at days 1 and 5 after vaccination returned to baseline level by day 14 (data not shown).
Clinical outcome
PSA-DT is widely used as an indicator of outcome [29] and was evaluated for vaccinated patients. PSA-DT showed significant increases during the study period (Fig. 2a), with an increase from 11.98 months (range −356.6 to 67.9) pre-study to 17.26 months (range −117.4 to 129.4) for the 24- to 48-month period post-vaccination (p = 0.0020 (Fig 2a)). This was a slow increase, not evident at the 0- to 24-month period. Over the whole study period (0–72 months), PSA-DT showed a significant increase (p = 0.0417) to 16.82 months (range −169.2 to 62.38), indicating a slowing of disease progression. Individual patient data are provided in Online Resource 3. Compared to baseline, PSA-DT increased in 24/30 patients at one or more time-points during the study and in 19/30 the PSA-DT increase continued to week 72. An increase of ≥200 % in PSA-DT at any point during the study was observed in 14/24, with 4/24 patients retaining this effect out to 72 weeks. Figure 2b shows time to next treatment in vaccinated patients compared to the control group. With a hazard ratio of 0.7352 (95 % confidence interval 0.37–1.45), time to next treatment was 243.3 weeks in the vaccinated group and 184.0 weeks in the control group (p = 0.3785).
Clinical responses. a Shows a box and whiskers plot of PSA-DT calculated for each patient pre-treatment, for 6-month periods on study and overall for the whole 72-week study follow-up. Data represent the median and range for all HLA-A2+, vaccinated patients (n = 30). PSA-DT at weeks 24–48 and over the 72-week follow-up period is significantly increased over pre-treatment (p = 0.0020 and p = 0.0417, respectively). b A Kaplan–Meier plot of the time to next treatment. Gray shading indicates the on-study period. The small vertical tick marks show censored times. The dashed line represents vaccinated HLA-A2+ patients (n = 30), and solid line shows the unvaccinated HLA-A2− control group (n = 32)
There was no objective reduction in PSA. At a median of 4.6 years’ follow-up, 5 vaccinated patients compared to 6 control group patients have died. No effect of DNA dose on outcome was detected.
Immunological responses
Immune monitoring was carried out on all patients, and responses are shown in Table 2. FrC-specific CD4+ and PSMA27-specific CD8+ T cells were evaluated using IFNγ ELISPOT. Ex vivo FrC-specific responses were used to assess vaccine operation and the effect of delivery modality. Of 30 patients, 29 had a significant CD4+ response to FrC following vaccination, in keeping with an expansion of a memory T-cell population detectable in the baseline samples. The median CD4+ T-cell response more than doubled by week 72 compared to baseline; baseline median IFNγ response was 34 spots/million (range 0–153) increasing to a median of 72 spots/million (range 1–306) at week 72 (p = 0.0208) (Fig. 3a).
Immune responses. a and b Represent data from all patients who completed vaccination (n = 29) displayed as a box and whiskers plot and show the median and range of CD4+ and CD8+ IFNγ responses to FrC protein and PSMA27 peptide at baseline (solid) and post-final vaccination (checked). c Shows the time to next treatment for 14 patients that required additional treatment and compares patients who made a PSMA27-specific CD8+ response (responder, n = 7) with those that did not have a detectable response (non-responder, n = 7). d and e, Scatter plots, represent patients who made a significant response up to week 24, comparing patients receiving vaccination without (−EP) or with (+EP) EP. d Compares CD4+ responses to FrC at baseline and at week of max response (n = 11 and n = 13 for −EP and +EP, respectively). e Compares CD8+ responses to PSMA27 at baseline (solid) and at week of max response (n = 7 and n = 6 for −EP and +EP, respectively). All CD8+ responses have been assessed after short term in vitro culture
T-cell responses against PSMA27 were assessed in circulating lymphocytes. Effector CD8+ T cells are unlikely to persist in blood, and as expected, we found only low levels ex vivo (6/30 positive responses detected, 3/6 being observed at 2 or more time-points). To detect central memory cells, we cultured blood T cells with peptide/IL-2 for 8 days in vitro [30]; IFNγ-producing PSMA27-specific T cells were detected in 55 % (16/30) of patients. The median CD8+ response had increased 9.6-fold by week 72 compared to baseline (from 27 spots/million (range 0–2,373) to 260 spots/million (range 0–8,233) (p = 0.0222)) (Fig. 3b). There was a trend for patients with detectable PSMA27-specific T cells to have an increased time to next treatment (Fig. 3c, p = 0.7925); we identified no link between PSA-DT and detection of circulating peptide-specific CD8+ T cells. There was no apparent effect of DNA dose on immunogenicity.
Effect of delivery on immune responses
The effect of vaccine delivery can be interpreted for the first 24 weeks, during which the 2 arms of the study remained independent. Thereafter, 11/15 patients crossed over to vaccination with EP for 2 doses per protocol based on an improvement in antibody responses to DOM with EP [24]. Figures 3d, e show CD4+ and CD8+ peak T-cell responses up to week 24, respectively. For both CD4+ and CD8+ responses, the delivery of vaccine ± EP generated a significant response compared to baseline. The effect of adding EP during delivery was not dramatic but there was a trend toward induction of higher levels of both CD4+ and CD8+ T-cell responses (p = 0.2128 for CD4+ T cells and p = 0.1014 for CD8+ T cells) (Fig. 3d, e). Clearly, larger numbers are required but this weak effect contrasts with the significant increase in humoral anti-DOM responses by adding EP [24].
Discussion
In HLA-A2 transgenic mice, pDOM-PSMA27 epitope vaccination stimulates strong peptide-specific CD8+ T-cell responses [22]. The PSMA27 epitope is processed from PSMA, and induced T cells can kill human target cells, confirming PSMA27 as a useful target for CD8+ T-cell attack. The phase I/II study we present here takes these observations to the clinic. In HLA-A2+ prostate cancer patients at biochemical failure, with low disease burden, vaccination significantly increased PSA-DT compared to pre-vaccination. We compared time to next treatment in vaccinated patients with a synchronous group of HLA-A2− patients. The data suggest that pDOM-PSMA27 vaccination could affect the natural history of prostate cancer and the suggestion that time to next treatment can be extended will need evaluation in a larger, randomized study. Whether HLA-A2 in its own right is an adverse prognostic factor has not been answered definitively, though there is a suggestion of link to prostate cancer incidence [31], increased proportion of large tumors (T3b–T3c) and higher post-operative Gleason sums compared to the HLA-A2− control group [32]. An adverse effect of HLA-A2 on outcome would strengthen a clinical effect of vaccination.
The increase in PSA-DT became visible after >24 weeks after first vaccination, and in 14/30 patients, the increase was 200 % or greater. From a baseline of 12 months, PSA-DT increased to 17 months. While caution is needed in the absence of randomized controls [33], a consistent story supporting an effect of vaccination at biochemical recurrence is emerging, where vaccination significantly increases PSA-DT [6, 9, 34–36]. Within the limits of comparability between studies, it appears that our DNA vaccine, targeting a single PSMA epitope, is at least as effective as other more complex DNA- or peptide-based vaccines.
T cells against the DOM helper sequence expanded in almost all (29/30, 97 %) patients, demonstrating patients’ immunocompetence and the immunological performance of the vaccine. pDOM-PSMA27 induced CD8+ T-cell responses in 16/30 (55 %) of patients, using pre-defined assay criteria and a single round of in vitro culture. Comparison of immunogenicity between trials is hampered by widely varying assay systems used for immune monitoring, and additionally, only few studies are available that report this data in comparable clinical settings [6, 9]. The dataset by McNeel et al. [9] with a full-length DNA vaccine encoding PAP is most similar to our own, and in this study, 3/22 patients had measurable CD8+ T-cell responses compared to 6/30 patients in our dataset ex vivo.
Incorporation of full-length antigen sequence into the DNA vaccine seems attractive since it would allow vaccination of all rather than to the 40 % of patients who carry HLA-A2 [9]. However, there are cogent reasons for using a peptide-focused vaccine since the inductive power of the repositioned peptide is generally considerably higher than from full-length sequence [37]. CD8+ T cells specific for a single epitope are clearly capable of suppressing even an acute viral infection [38]. Should escape from focused attack occur, a second vaccine against a different epitope could be used [39], and we are exploring double attack in our current clinical trial against the WT-1 antigen [40]. Although our vaccine design could readily incorporate tumor-derived MHC class II-binding epitopes, there is no clear evidence that these are required for the maintenance of cytotoxic T cells and there is a danger that regulatory T cells might be induced [13, 41].
Viral vector–based vaccines have the problem of pre-existing or induced antiviral immunity. However, an MVA-MUC-1 vaccine induced an IFNγ+ T-cell response to MUC-1 after short-term culture in 7/34 patients with prostate cancer [6]. Pox viral delivery in metastatic disease also generated PSA peptide-specific CD8+ T-cell responses in 13/29 patients following PSA-TRICOM vaccination [42] and in 9/24 patients following MVA-Trovax vaccination [43]. It appears that our approach has at least comparable immunogenicity. We would contend, however, that avoiding blocking immunity, likely to arise from MVA [44], will be important for repeated vaccinations required to maintain attack on cancer. A concern at the outset of our study had been whether T-cell responses would be durable, as with some vaccines approaches CD8+ T-cell responses can be lost rapidly and then not re-expand after repeated injection [18]. Our data argue that with DNA vaccination this is not a problem with T-cell responses maintained to the end of the follow-up period.
To examine whether our DNA vaccine had sufficient potency to be scaled from mouse to human, we examined the delivery of our DNA vaccine using the Inovio Elgen100 device for the first time in the clinic. We had found pre-clinically [22, 45] that EP increased antibody responses, with lesser increase in CD8+ T-cell responses to our DNA fusion vaccine. In the clinic, this dichotomy is also evident with clear increases in antibody [24] but only a trend for increase in both CD4+ and CD8+ T-cell responses with EP. After cross-over of 11/15 patients to EP boosting, there is a significant and durable increase to the end of the study but we can no longer assess the impact of the individual delivery modalities. It is intriguing to speculate why EP has an apparently smaller effect on T-cell responses compared to humoral responses. In the trial, this may simply be a reflection of very small patient numbers treated without electroporation, and a randomized dataset needs to evaluate the comparative question further. A possible explanation for both the murine and human data could be that unlike B-cell responses, where the increased muscular antigen expression after electroporation leads to higher humoral responses [24], for T cells there may not be such a strict correlation with the quantity of antigen expressed by the muscle cells.
In summary, the pDOM-PSMA27 vaccine is safe, generates anti-PSMA responses in the majority of patients and is associated with an increase in PSA-DT. Use of EP was well tolerated and may increase T-cellular vaccine efficacy. These findings merit further testing in a randomized setting. Examining the vaccine-induced T cells for their ability to home to the tumor will be a critical component of further evaluation and may offer the tool to better identify a link between vaccine-induced immunity and clinical outcome.
References
Rosenberg SA (2004) Shedding light on immunotherapy for cancer. N Engl J Med 350(14):1461–1463
Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel JC, Akerley W, van den Eertwegh AJ, Lutzky J, Lorigan P, Vaubel JM, Linette GP, Hogg D, Ottensmeier CH, Lebbe C, Peschel C, Quirt I, Clark JI, Wolchok JD, Weber JS, Tian J, Yellin MJ, Nichol GM, Hoos A, Urba WJ (2010) Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 363(8):711–723
Robert C, Thomas L, Bondarenko I, O’Day S, Weber J, Garbe C, Lebbe C, Baurain JF, Testori A, Grob JJ, Davidson N, Richards J, Maio M, Hauschild A, Miller WH Jr, Gascon P, Lotem M, Harmankaya K, Ibrahim R, Francis S, Chen TT, Humphrey R, Hoos A, Wolchok JD (2011) Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. New England J Med 364(26):2517–2526
Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, Redfern CH, Ferrari AC, Dreicer R, Sims RB, Xu Y, Frohlich MW, Schellhammer PF (2011) Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med 363(5):411–422
Drake CG (2010) Prostate cancer as a model for tumour immunotherapy. Nat Rev Immunol 10(8):580–593
Dreicer R, Stadler WM, Ahmann FR, Whiteside T, Bizouarne N, Acres B, Limacher JM, Squiban P, Pantuck A (2009) MVA-MUC1-IL2 vaccine immunotherapy (TG4010) improves PSA doubling time in patients with prostate cancer with biochemical failure. Investig New Drugs 27(4):379–386
Roos AK, King A, Pisa P (2008) DNA vaccination for prostate cancer. Methods Mol Biol 423:463–472
Kantoff PW, Schuetz TJ, Blumenstein BA, Glode LM, Bilhartz DL, Wyand M, Manson K, Panicali DL, Laus R, Schlom J, Dahut WL, Arlen PM, Gulley JL, Godfrey WR (2010) Overall survival analysis of a phase II randomized controlled trial of a Poxviral-based PSA-targeted immunotherapy in metastatic castration-resistant prostate cancer. J Clin Oncol 28(7):1099–1105
McNeel DG, Dunphy EJ, Davies JG, Frye TP, Johnson LE, Staab MJ, Horvath DL, Straus J, Alberti D, Marnocha R, Liu G, Eickhoff JC, Wilding G (2009) Safety and immunological efficacy of a DNA vaccine encoding prostatic acid phosphatase in patients with stage D0 prostate cancer. J Clin Oncol 27(25):4047–4054
Waeckerle-Men Y, Uetz-von Allmen E, Fopp M, von Moos R, Bohme C, Schmid HP, Ackermann D, Cerny T, Ludewig B, Groettrup M, Gillessen S (2006) Dendritic cell-based multi-epitope immunotherapy of hormone-refractory prostate carcinoma. Cancer Immunol Immunother 55(12):1524–1533
Murphy GP, Tjoa BA, Simmons SJ, Ragde H, Rogers M, Elgamal A, Kenny GM, Troychak MJ, Salgaller ML, Boynton AL (1999) Phase II prostate cancer vaccine trial: report of a study involving 37 patients with disease recurrence following primary treatment. Prostate 39(1):54–59
Wolchok JD, Gregor PD, Nordquist LT, Slovin SF, Scher HI (2003) DNA vaccines: an active immunization strategy for prostate cancer. Semin Oncol 30(5):659–666
Disis ML (2010) Immune regulation of cancer. J Clin Oncol 28(29):4531–4538
Bilusic M, Heery C, Madan RA (2011) Immunotherapy in prostate cancer: emerging strategies against a formidable foe. Vaccine 29(38):6485–6497
Perambakam S, Xie H, Edassery S, Peace DJ (2010) Long-term follow-up of HLA-A2+ patients with high-risk, hormone-sensitive prostate cancer vaccinated with the prostate specific antigen peptide homologue (PSA146-154). Clin Dev Immunol 2010:473453
Uemura H, Fujimoto K, Mine T, Uejima S, de Velasco MA, Hirao Y, Komatsu N, Yamada A, Itoh K (2010) Immunological evaluation of personalized peptide vaccination monotherapy in patients with castration-resistant prostate cancer. Cancer Sci 101(3):601–608
Schwartzentruber DJ, Lawson DH, Richards JM, Conry RM, Miller DM, Treisman J, Gailani F, Riley L, Conlon K, Pockaj B, Kendra KL, White RL, Gonzalez R, Kuzel TM, Curti B, Leming PD, Whitman ED, Balkissoon J, Reintgen DS, Kaufman H, Marincola FM, Merino MJ, Rosenberg SA, Choyke P, Vena D, Hwu P (2011) gp100 peptide vaccine and interleukin-2 in patients with advanced melanoma. N Engl J Med 364(22):2119–2127
Rezvani K, Yong AS, Mielke S, Jafarpour B, Savani BN, Le RQ, Eniafe R, Musse L, Boss C, Kurlander R, Barrett AJ (2011) Repeated PR1 and WT1 peptide vaccination in Montanide-adjuvant fails to induce sustained high-avidity, epitope-specific CD8+ T cells in myeloid malignancies. Haematologica 96(3):432–440
Kaufman HL, Wang W, Manola J, DiPaola RS, Ko YJ, Sweeney C, Whiteside TL, Schlom J, Wilding G, Weiner LM (2004) Phase II randomized study of vaccine treatment of advanced prostate cancer (E7897): a trial of the Eastern cooperative oncology group. J Clin Oncol 22(11):2122–2132
Rice J, Ottensmeier CH, Stevenson FK (2008) DNA vaccines: precision tools for activating effective immunity against cancer. Nat Rev Cancer 8(2):108–120
Lu J, Celis E (2002) Recognition of prostate tumor cells by cytotoxic T lymphocytes specific for prostate-specific membrane antigen. Cancer Res 62(20):5807–5812
Vittes GE, Harden EL, Ottensmeier CH, Rice J, Stevenson FK (2011) DNA fusion gene vaccines induce cytotoxic T-cell attack on naturally processed peptides of human prostate-specific membrane antigen. Eur J Immunol 41(8):2447–2456
Ahlen G, Soderholm J, Tjelle T, Kjeken R, Frelin L, Hoglund U, Blomberg P, Fons M, Mathiesen I, Sallberg M (2007) In vivo electroporation enhances the immunogenicity of hepatitis C virus nonstructural 3/4A DNA by increased local DNA uptake, protein expression, inflammation, and infiltration of CD3+ T cells. J Immunol 179(7):4741–4753
Low L, Mander A, McCann K, Dearnaley D, Tjelle T, Mathiesen I, Stevenson F, Ottensmeier CH (2009) DNA vaccination with electroporation induces increased antibody responses in patients with prostate cancer. Hum Gene Ther 20(11):1269–1278
Tjelle TE, Salte R, Mathiesen I, Kjeken R (2006) A novel electroporation device for gene delivery in large animals and humans. Vaccine 24(21):4667–4670
Britten CM, Janetzki S, van der Burg SH, Huber C, Kalos M, Levitsky HI, Maecker HT, Melief CJ, O’Donnell-Tormey J, Odunsi K, Old LJ, Pawelec G, Roep BO, Romero P, Hoos A, Davis MM (2011) Minimal information about T cell assays: the process of reaching the community of T cell immunologists in cancer and beyond. Cancer Immunol Immunother 60(1):15–22
Janetzki S, Britten CM, Kalos M, Levitsky HI, Maecker HT, Melief CJ, Old LJ, Romero P, Hoos A, Davis MM (2009) “MIATA”-minimal information about T cell assays. Immunity 31(4):527–528
Mander A, Chowdhury F, Low L, Ottensmeier CH (2009) Fit for purpose? A case study: validation of immunological endpoint assays for the detection of cellular and humoral responses to anti-tumour DNA fusion vaccines. Cancer Immunol Immunother 58(5):789–800
Arlen PM, Bianco F, Dahut WL, D’Amico A, Figg WD, Freedland SJ, Gulley JL, Kantoff PW, Kattan MW, Lee A, Regan MM, Sartor O (2008) Prostate Specific Antigen Working Group guidelines on prostate specific antigen doubling time. J Urol 179(6):2181–2185; discussion 2185-2186
Todryk SM, Pathan AA, Keating S, Porter DW, Berthoud T, Thompson F, Klenerman P, Hill AV (2009) The relationship between human effector and memory T cells measured by ex vivo and cultured ELISPOT following recent and distal priming. Immunology 128(1):83–91
De Petris L, Bergfeldt K, Hising C, Lundqvist A, Tholander B, Pisa P, van der Zanden HG, Masucci G (2004) Correlation between HLA-A2 gene frequency, latitude, ovarian and prostate cancer mortality rates. Med Oncol 21(1):49–52
Hueman MT, Dehqanzada ZA, Novak TE, Gurney JM, Woll MM, Ryan GB, Storrer CE, Fisher C, McLeod DG, Ioannides CG, Ponniah S, Peoples GE (2005) Phase I clinical trial of a HER-2/neu peptide (E75) vaccine for the prevention of prostate-specific antigen recurrence in high-risk prostate cancer patients. Clin Cancer Res 11(20):7470–7479
Smith MR, Kantoff PW (2010) Changes in PSA kinetics after DNA vaccine therapy-not so fast! J Clin Oncol 28 (4):e58; author reply e59
Feyerabend S, Stevanovic S, Gouttefangeas C, Wernet D, Hennenlotter J, Bedke J, Dietz K, Pascolo S, Kuczyk M, Rammensee HG, Stenzl A (2009) Novel multi-peptide vaccination in Hla-A2+ hormone sensitive patients with biochemical relapse of prostate cancer. Prostate 69(9):917–927
DiPaola R, Chen Y, Bubley G, Hahn N, Stein M, Schlom J, Gulley L, Lattime E, Carducci M, Wilding G (2009) A phase II study of PROSTVAC-V (vaccinia)/TRICOM and PROSTVAC-F (fowlpox)/TRICOM with GM-CSF in patients with PSA progression after local therapy for prostate cancer: results of ECOG 9802. In: ASCO Genitourinary Cancers Symposium, 2009:abstract 108
North SA, Graham K, Bodnar D, Venner P (2006) A pilot study of the liposomal MUC1 vaccine BLP25 in prostate specific antigen failures after radical prostatectomy. J Urol 176(1):91–95
Rice J, Buchan S, Stevenson FK (2002) Critical components of a DNA fusion vaccine able to induce protective cytotoxic T cells against a single epitope of a tumor antigen. J Immunol 169(7):3908–3913
Bartholdy C, Stryhn A, Christensen JP, Thomsen AR (2004) Single-epitope DNA vaccination prevents exhaustion and facilitates a broad antiviral CD8+ T cell response during chronic viral infection. J Immunol 173(10):6284–6293
Liu J, Ewald BA, Lynch DM, Nanda A, Sumida SM, Barouch DH (2006) Modulation of DNA vaccine-elicited CD8+ T-lymphocyte epitope immunodominance hierarchies. J Virol 80(24):11991–11997
Chaise C, Buchan SL, Rice J, Marquet J, Rouard H, Kuentz M, Vittes GE, Molinier-Frenkel V, Farcet JP, Stauss HJ, Delfau-Larue MH, Stevenson FK (2008) DNA vaccination induces WT1-specific T-cell responses with potential clinical relevance. Blood 112(7):2956–2964
Antony PA, Piccirillo CA, Akpinarli A, Finkelstein SE, Speiss PJ, Surman DR, Palmer DC, Chan CC, Klebanoff CA, Overwijk WW, Rosenberg SA, Restifo NP (2005) CD8+ T cell immunity against a tumor/self-antigen is augmented by CD4+ T helper cells and hindered by naturally occurring T regulatory cells. J Immunol 174(5):2591–2601
Gulley JL, Arlen PM, Madan RA, Tsang KY, Pazdur MP, Skarupa L, Jones JL, Poole DJ, Higgins JP, Hodge JW, Cereda V, Vergati M, Steinberg SM, Halabi S, Jones E, Chen C, Parnes H, Wright JJ, Dahut WL, Schlom J (2010) Immunologic and prognostic factors associated with overall survival employing a poxviral-based PSA vaccine in metastatic castrate-resistant prostate cancer. Cancer Immunol Immunother CII 59(5):663–674
Amato RJ, Drury N, Naylor S, Jac J, Saxena S, Cao A, Hernandez-McClain J, Harrop R (2008) Vaccination of prostate cancer patients with modified vaccinia ankara delivering the tumor antigen 5T4 (TroVax): a phase 2 trial. J Immunother 31(6):577–585
Smith CL, Dunbar PR, Mirza F, Palmowski MJ, Shepherd D, Gilbert SC, Coulie P, Schneider J, Hoffman E, Hawkins R, Harris AL, Cerundolo V (2005) Recombinant modified vaccinia Ankara primes functionally activated CTL specific for a melanoma tumor antigen epitope in melanoma patients with a high risk of disease recurrence. Int J Cancer 113(2):259–266
Buchan S, Gronevik E, Mathiesen I, King CA, Stevenson FK, Rice J (2005) Electroporation as a “prime/boost” strategy for naked DNA vaccination against a tumor antigen. J Immunol 174(10):6292–6298
Acknowledgments
This work was supported by the NIHR Southampton Experimental Cancer Medicine Centre, funded by Cancer Research UK and the Department of Health, UK. Clinical work was undertaken in the University Hospitals Southampton and at the Royal Marsden NHS Foundation Trust who received a proportion of its funding from the NHS Executive. The work was further supported by the Alan Willett Foundation, an unrestricted educational grant from Inovio Pharmaceuticals, the Institute of Cancer Research, the Bob Champion Cancer Trust and Cancer Research UK Section of Radiotherapy [CRUK] grant number C46/A2131. We acknowledge NHS funding to the NIHR Biomedical Research Centre and support by the Welcome Trust Clinical Research Facility, Southampton. Assay development and validation was in part supported by the Wallace Coulter Foundation.
Conflict of interest
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Chudley, L., McCann, K., Mander, A. et al. DNA fusion-gene vaccination in patients with prostate cancer induces high-frequency CD8+ T-cell responses and increases PSA doubling time. Cancer Immunol Immunother 61, 2161–2170 (2012). https://doi.org/10.1007/s00262-012-1270-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-012-1270-0