Abstract
Introduction
The development of Her-2 DNA vaccine has progressed through three phases that can be categorized as phase “A”: the pursuit of Her-2 as a tumor-associated “antigen”, phase “B”: tilting the “balance” between tumor immunity and autoimmunity and phase “C”: the on-going “clinical trials”.
Materials and methods
In phase “A”, a panel of human ErbB-2 or Her-2 plasmids were constructed to encode non-transforming Her-2 derivatives. The immunogenicity and anti-tumor activity of Her-2 DNA vaccines were tested in human Her-2 transgenic mice with or without the depletion of regulatory T cells (Tregs). However, Treg depletion or other immune modulating regimens may increase the risk of autoimmunity. In phase “B”, the balance between tumor immunity and autoimmunity was assessed by monitoring the development of experimental autoimmune thyroiditis (EAT). To test the efficacy of Her-2 DNA vaccines in cancer patients, clinical trials have been initiated in phase “C”.
Results and conclusions
Significant anti-Her-2 and anti-tumor activity was observed when Her-2 transgenic mice were electro-vaccinated after Treg depletion. Susceptibility to EAT was also enhanced by Treg depletion and there was mutual amplification between Her-2 immunity and EAT development. Although Tregs regulate both EAT and Her-2 immunity, their effector mechanisms may differ. It may be possible to amplify tumor immunity with improved strategies that can by-pass undue autoimmunity. Critical information will be revealed in the next decade to expedite the development of cancer vaccines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The development of a cancer vaccine generally progresses through three phases that can be categorized as phases “A, B and C”. In phase “A”, the effort is focused on the “antigen” of interest. Much debate goes into choosing the target molecule, whereas the vaccine formulation may be based on rational design or technical feasibility. An appropriate animal model is a must and determines the validity of the experimental approach. A less considered, but equally important issue is the “balance” between the induction of tumor immunity and autoimmune diseases or phase “B” of the study. Since tolerance to tumor associated antigen (TAA) is profound, strenuous immune modulation is required to achieve meaningful response. A predictable side effect of such immune modulation is inadvertent reactivity to self-antigens. Yet, the balance between tumor immunity and autoimmunity is often considered in a cursory manner in pre-clinical studies and autoimmune side effects are treated symptomatically in patients undergoing immunotherapy. When a “clinical trial” of the candidate vaccine is initiated in phase “C”, it can mark the beginning or the end of the effort. In this presentation, the “A, B and C” of Her-2 DNA vaccine development is summarized with our current perspective.
Phase A: Her-2 as the vaccine antigen
In the late 1990s, we chose Her-2 as our vaccine target because of the amplified expression on tumor cells and oncogenic activity [1–5]. This choice is now supported by the efficacy of anti-Her-2 mAb Trastuzumab (Herceptin) in Her-2 positive breast cancer therapy [6]. Naked DNA was selected as the vaccine formulation because of its stable and well-defined nature and because humoral and cellular immune responses to the entire repertoire of antigenic epitopes could be induced. Since it is free of confounding foreign entities, DNA vaccines can be administered repeatedly without losing activity. The feasibility of producing large quantities of pure DNA with simple tools is another major advantage. From intramuscular injection of Her-2 DNA, the vaccine regimen has evolved to include both Her-2 and cytokine DNA administered together by electroporation after regulatory T cell depletion [5, 7–16]. The activity of this improved regimen exceeded our initial expectation and Her-2 DNA vaccine is showing promise as a clinical vaccine candidate.
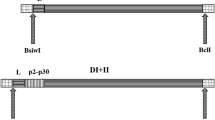
Her-2 DNA vaccine constructs
A panel of human ErbB-2 (E2) DNA constructs have been generated to encode recombinant Her-2 proteins that are free of tyrosine kinase activity and traffic to specific sub-cellular compartments [5, 7, 17]. Of the four basic constructs, pE2A encodes the full length Her-2 with a single substitution of aa Lys753 to Ala753 to remove the ATP binding lysine residue. pE2TM encodes the signal peptide, extracellular and transmembrane domains without the intracellular domain (ICD). psecE2 encodes the N-terminus aa 1–505 of the extracellular domain as a secreted protein. These three constructs induced both cellular and humoral immune responses and strong protective immunity in BALB/c and C57BL/6 mice. Another construct pcytE2, with truncated ER signal peptide, directs the synthesis of a full-length, short-lived cytoplasmic protein, which is promptly degraded by the proteasome [7]. Accordingly, immunization with pcytE2 activates CD8 T cells without humoral response. In the early studies, Her-2 DNA alone was administered intramuscularly (i.m.) [5, 7, 17]. Later, pGM-CSF was added to the formulation and electroporation was administered at the vaccination site to enhance gene expression and immune reactivity [15, 16, 18].
Although significant Her-2 immunity with complete tumor rejection was achieved in wild type mice, it was necessary to further evaluate vaccine activity in animals that express human Her-2 as a self-antigen to mimic immune tolerance in humans.
Her-2 transgenic mice
Several transgenic mouse strains that express either wild type or mutant rat neu had been developed [19, 20]. Before human Her-2 transgenic mice were available, rat neu transgenic mice were the next best choice and tumors derived from these mice continue to serve important functions in biological studies. Assessment of reactivity against neu induced tumors in neu transgenic mice induced by heterologous human Her-2 vaccine [16], however, may not mimic the events in humans and the results may even be misleading.
To test Her-2 vaccines in a more relevant system, Her-2 transgenic mice were generated in our lab using whey acid protein (WAP) promoter to drive the wild type human ErbB-2 gene [11]. The mice have been back-crossed into C57BL/6 background and are maintained as herterozygotes because homozygous pups are never born. Spontaneous tumors have not been detected in any organs. C57BL/6 Her-2 transgenic mice produce little to no antibodies (Ab) or T cells when immunized with Her-2 DNA, showing their profound immune tolerance to Her-2 [11]. This poor responsiveness verifies Her-2 as a self-antigen and these mice are invaluable for testing candidate Her-2 vaccines. Because these mice do not develop spontaneous tumors, syngeneic tumors expressing human Her-2 by transfection are tested in Her-2 transgenic mice. Additional backcrosses into other mouse strains are underway and their immune responses to Her-2 DNA vaccine are being investigated.
On the occasions when Her-2/neu induced spontaneous mammary tumors are required, we use tumors from BALB NeuT mice, which express a transforming rat neu and develop spontaneous mammary tumors between 17 and 19 weeks of age. When it is necessary to test DNA vaccines in these mice, rat neu DNA is used. Several mammary tumor lines have been derived from NeuT spontaneous tumors, such as TUBO [20] and Bam1a [21] which grow progressively in NeuT as well as normal BALB/c mice. These cell lines are convenient test systems for Her-2/neu targeted therapies.
Amplification of immune reactivity to Her-2 by depleting regulatory T cells (Tregs)
The weak response of Her-2 transgenic mice to DNA vaccine may result from a reduced T cell receptor repertoire via negative selection in the thymus or suppression of immune reactivity by peripheral regulatory cells. With reports documenting suppressive activity of CD4+CD25+ Tregs in autoimmune diseases [22], we tested the effect of Treg depletion on tumor immunity. In the initial experiment, BALB/c mice were injected i.p. with CD25 mAb, PC61, either 5 and 6 days before or 1 and 3 days after s.c. inoculation with TUBO or D2F2/E2 cells. D2F2/E2 cells were hormone-induced BALB/c mammary tumor cells stably transfected with human Her-2. Tumors developed in all mice, but >90% of the tumors in Treg depleted mice regressed completely, even after they reached the size of 180 mm3 [13, 15]. This dramatic tumor regression was induced simply by depleting Tregs, demonstrating in situ priming by a growing tumor. This finding challenges the long-standing paradigm that solid tumors are poor at priming the immune system, thus cannot be rejected effectively by immune cells. Rather, the immunogenicity of a tumor can be functional and powerful when the mice are free of negative regulation.
To test if anti-Her-2 immunity in tolerant mice was also under the control of Tregs [13–15], Her-2 transgenic mice were treated with anti-CD25 mAb 1 week before DNA electro-vaccination, then boosted three times every 2 weeks with the same DNA. Reduction in CD4+CD25hi cells in the peripheral blood was verified by flow cytometry. The levels of Her-2 Abs were enhanced from undetectable in mice with intact Tregs to 28 ± 27 μg/ml in Treg depleted mice. Therefore, Tregs suppressed Her-2/neu reactivity whether Her-2 was a foreign or self-antigen.
Antibodies (Abs) induced by Her-2 or neu DNA recognized only cognate antigen
After Her-2 and neu transgenic mice were both established, the activity of autologous versus heterologous Her-2/neu vaccines were tested. Wild type, Her-2 or neu transgenic mice were immunized with either human Her-2 or rat neu DNA vaccines. In normal BALB/c and C57BL/6 mice, immunization with Her-2 or neu DNA induced antigen specific IgG which did not cross-react with non-cognate Her-2 or neu [16]. This non-cross-reactive humoral response held true in Her-2 and neu transgenic mice [16]. Vaccination of Her-2 transgenic mice with self Her-2, but not neu induced anti-Her-2 Abs. Similarly, vaccination of NeuT transgenic mice with self neu but not heterologous Her-2 DNA induced anti-neu Abs.
T cells activated by Her-2 or neu DNA exhibited limited cross-reactivity
Compared to humoral response, T cell response induced by heterologous Her-2/neu was more promiscuous. After neu DNA vaccination, BALB/c mice generated T cells that recognized both Her-2 and neu and they rejected D2F2 tumors expressing either Her-2 or neu, showing T cell cross-reactivity when Her-2 and neu were foreign antigens. When NeuT mice were immunized with heterologous pE2TM, splenocytes reacted strongly to human Her-2 and moderately to self rat neu, with anti-neu reactivity at comparable or lower level than that induced by autologous neu DNA vaccine. Conversely, when Her-2 transgenic mice were immunized with heterologous pneuTM, neu-reactive T cells were generated, but they did not recognize autologous Her-2. Therefore, heterologous Her-2/neu vaccines induced Ab to cognate antigen only and induced T cells with varying levels of cross-reactivity to autologous antigens.
In NeuT mice, autologous pneuTM immunization induced T cells that reacted with neu expressing cells, but not the dominant neu epitope, N63, indicating a reduced or altered T cell repertoire in the tolerant host. This finding is consistent with the reported recognition of sub-dominant epitopes [23] or the presence of low avidity CD8 T cells [24] in the immunized FVBneuN transgenic mice. Similarly, CEA transgenic mice also recognized sub-dominant CEA epitopes and this was associated with the expression of CEA in thymic epithelial cells [25].
There have been a number of unidirectional studies on human Her-2 vaccines in rat neu transgenic mice. Immunization of NeuT mice with an adenoviral vector encoding Her-2 induced low-level cross-reactive Abs to neu and delayed tumor formation [26]. The adenoviral vector may induce a broader spectrum of Abs than naked DNA, thus the modest cross-reactivity with neu. In FVBneuN mice, spontaneous tumorigenesis was reduced by immunization with Her-2 DNA every month for 10 months [27]. It is possible that 10 monthly vaccinations with heterologous Her-2 induced enough cross-reactive T cells to autologous neu to exert anti-tumor effect. Tegerstedt et al. [28] reported delay of spontaneous tumorigenesis in BALB NeuT mice by immunization with a single dose of virus-like particle (VLP) displaying heterologous Her-2. It was unclear if cross-reactive Ab or T cells mediated the activity. In most reported vaccine studies including our own, spontaneous tumorigenesis in NeuT mice was controlled primarily by Ab, because NeuT tumors were highly sensitive to Ab even when T cell activity was too low to make an impact [16]. The sensitivity of NeuT tumors to anti-neu antibodies may reflect their exquisite dependence on neu-mediated signals for survival and proliferation.
Her-2/neu model systems recommended for vaccine studies
The limited and variable cross-reactivity between Her-2 and neu responses highlights the importance of using human Her-2 transgenic mice to evaluate human Her-2 vaccines in pre-clinical studies. Rat neu transgenic mice are valuable for establishing the principles of Her-2/neu targeted therapy, but should be used with caution in human vaccine development. Furthermore, all Her-2/neu positive tumor cells are not equally sensitive to Ab treatment. With the increasing use of Her-2 targeted drugs such as Herceptin or tyrosine kinase inhibitors, the surviving tumor cells may become more resilient, requiring stronger immune modulation to exert anti-tumor immunity.
Phase B: “balance” tumor immunity with autoimmunity
Autoimmune thyroiditis
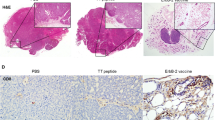
To address autoimmune side-effects during cancer immunotherapy, the induction of experimental autoimmune thyroiditis (EAT), a model of Hashimoto’s thyroiditis, was chosen as the indicator of inadvertent autoimmunity. Hashimoto’s thyroiditis, a hypothyroid syndrome, is one of the most prevalent autoimmune manifestations in humans, with 45% of women and 20% of men in USA showing focal thyroiditis at routine autopsy, although only 1% of women and 0.5% of men exhibit clinical symptoms. It is characterized by mononuclear cell infiltration and destruction of the thyroid, elevation of thyroid-stimulating hormone and decrease of thyroid hormones (T3 and T4). The production of autoantibodies to thyroglobulin and thyroid peroxidase [29], and T cell activation by thyroid antigens [30] are indicators of autoreactivity. Susceptibility to thyroiditis is strongly influenced by the haplotype of class II MHC [31]. For example, human HLA-DRB1*0301 (DR3) or murine H2k confers susceptibility to autoimmune thyroiditis [32, 33], whereas C57BL/6 H2b and BALB/c H2d are associated with resistance [34]. DR3, expressed in 24% of normal individuals, is also associated with type 1 diabetes [35] with approximately 20% of type 1 diabetic patients also developing autoimmune thyroid disease [36]. In susceptible individuals, clinical symptoms of thyroiditis are precipitated by endogenous or environmental factors, such as hormone stimulation, dietary iodide level, infection, irradiation, immunostimulatory cytokines, etc., some of these factors are consequences of cancer immunotherapy.
EAT is a well-studied mouse model and is inducible by immunization with mouse thyroglobulin (mTg), the 660 kD storage protein for iodinated thyroid hormone. To simulate humans with circulating thyroid antigens and experiencing various triggering factors, mouse EAT is induced by injecting mTg with an adjuvant such as LPS, or by repeated injections of soluble mTg [15, 37, 38]. Although thyroiditis patients can be treated effectively by hormone replacement therapy, EAT serves as a well-defined experimental system for mechanistic analysis and is a sensitive read-out of autoimmune complications in cancer therapy [39–41].
Tregs in EAT
Removal of suppressor T cells by early thymectomy and/or irradiation leading to low incidence of autoimmune diseases, including thyroiditis and gastritis, was shown in the mid-70s and CD4+ T cells were shown to mediate tolerance in EAT [42]. The CD25 marker enables the separation of Tregs [43, 44]. Removal of CD25+ Tregs enabled EAT resistant mice to develop thyroiditis upon stimulation and abrogated induced tolerance to EAT [15, 44, 45]. Other immune modulating agents, such as antagonist anti-CTLA-4 (Kong, unpublished), agonist anti-CD137 [44] or anti-GITR mAb [46] interfered with the establishment of EAT tolerance. During long-term cancer immunotherapy with repeated blockade of Tregs and/or co-stimulation of T effctors, different autoimmune diseases could manifest themselves [47–52].
Concurrent induction of tumor immunity and autoimmunity by Treg depletion
In BALB/c mice inoculated with TUBO tumor, treatment with anti-CD25 mAb induced tumor regression and neu specific T cells [15]. When the same mice received mTg by chronic i.v. injections, they produced mTg specific Ab and T cells with inflammatory infiltration in the thyroids [15]. The immune responses to neu or mTg were greater in mice undergoing TUBO tumor rejection and mTg injection than in those experiencing either alone. This was the first experimental study to assess amplification of tumor immunity and possible exacerbation of auto-reactivity. To further analyze the concurrent immune responses to Her-2/neu and mTg, we examined genetic regulation of the response in Her-2 tolerant mice.
Genetic regulation of tumor immunity and autoimmunity
A mouse model that expressed both mTg and human Her-2 as self-antigens and expressed HLA-DR3 was established to query the development of EAT during Her-2 vaccination. Heterozygous C57BL/6 Her-2 transgenic mice were mated with homozygous DR3+Abo mice (provided by Dr Chella David, Mayo Clinic, Rochester, MN), which expressed the HLA-DR3 transgene in the absence of endogenous mouse MHC II. The pups were either Her-2+DR3+ or Her-2−DR3+. The parental B6 Her-2 transgenic mice and the Her-2+DR3+ F1 mice both expressed Her-2 as a self-antigen, but with or without DR3, which dictated susceptibility to EAT. IAb of C57BL/6 mice which lack IE, mediated a resistant phenotype to EAT [32]. It has been shown in F1 mice that the parental susceptibility allele was dominant over parental resistant allele [53]. DR3 was expressed in ∼20% of DR3Abo PBL and in 10–15% of F1 PBL.

To measure immune reactivity to Her-2 DNA vaccine, mice were electro-vaccinated with pE2TM and pGM-CSF encoding the extracellular and transmembrane domains of Her-2 and the murine GM-CSF, respectively. To induce EAT, mice received mTg i.v. with or without LPS. Depletion of Tregs enhanced immune reactivity to Her-2 as well as mTg, verifying control of both Her-2 and mTg responses by Tregs [18]. Her-2+ × DR3 and Her-2− × DR3 mice expressing H2b × DR3 haplotype developed more profound mTg response and thyroid pathology than Her-2 or C57BL/6 mice which expressed the EAT resistant H2b haplotype. On the contrary, Her-2 reactivity was comparable whether mice expressed HLA-DR3 or not. Therefore, induction of Her-2 immunity was independent of HLA-DR3 but development of EAT was dictated by this allele, whereas Tregs control the responses to both self-antigens.
These results, however, cannot be taken to indicate MHC independence in Her-2 reactivity. Our preliminary data with Her-2 transgenic mice in C57BL/6 versus BALB/c background suggested a significant difference in their reactivity to Her-2 DNA vaccination (not shown). Although the susceptibility to autoimmunity can be predicted, in part, by class II MHC haplotype, genetic regulation of reactivity to cancer vaccine remains to be determined.
Phase C: “clinical trials”
Her-2 DNA vaccine trials
Several Her-2 DNA vaccine trials have been initiated. A pilot clinical trial testing pVAX-E2A was conducted at the Karolinska Institute, Stockholm, Sweden, in stage IV breast cancer patients. The trial entitled “Vaccine immunization with nucleic acid coding for the gene Her-2/neu together with low doses GM-CSF (Leucomax*) and IL-2 (Proleukin*) as adjuvant in patients with metastatic breast carcinoma” showed no adverse effect. In industry sponsored trials, V930 encoding Her-2 and CEA, generated by Merck, is tested in a phase I trial “V930 First in Man (FIM) Study”. The patients in this study included Stages II, III, IV breast, colon, ovarian or non-small cell lung cancer patients with detectable Her-2 and/or CEA expression (http://clinicaltrials.gov/ct/show/NCT00250419?order = 1). Bavarian Nordic’s subsidiary BN ImmunoTherapeutics (BNIT) started a “Phase I trial of a fixed dose of MVA-BN-HER2 following first- or second-line chemotherapy for HER-2-positive metastatic breast cancer” with MVA-BN-HER-2, a highly attenuated non-replicating vaccinia virus, MVA-BN®, engineered to encode a modified form of the Her-2 protein. http://clinicaltrials.gov/ct/show/NCT00485277?order = 1.
Autoimmune side effects in cancer immunotherapy trials
In cancer patients more strenuous effort than one-time Treg depletion may be required to overcome immune regulatory mechanisms before adequate vaccination efficacy can be induced, with increasing risk of autoimmunity from each new component. Our results showed that even genetically resistant BALB/c mice became susceptible to EAT after Tregs depletion, particularly during tumor regression. Patients expressing high risk HLA haplotypes will require close monitoring of their autoreactivity when their immune regulatory mechanisms are dampened. Severe autoimmune symptoms have already surfaced in cancer immunotherapy trials. In a reported clinical trial testing Her-2 peptide vaccine combined with systemic Flt-3 ligand, 2 of 15 subjects developed elevated thyroid stimulating hormone with symptoms of grade 2 hypothyroidism [39]. In another reported trial, patients with metastatic melanoma received gp100 peptide vaccines along with antagonistic mAb to CTLA-4 [48, 51, 52]. Patients with grade III/IV autoimmune manifestations were observed, including dermatitis, enterocolitis, hepatitis, hypophysitis, hypothyroidism and uveitis. The patients with objective cancer regression all developed severe autoimmune symptoms requiring intervention.
Based on the clinical experience and our findings in EAT model, patients receiving immunomodulating agents, particularly those with susceptible HLA haplotypes, should be closely monitored for autoimmune pathology. Once the importance of balancing tumor immunity with the risk of autoimmunity is recognized, novel strategies can be designed to tilt the balance toward tumor immunity. As an example, direct manipulation of the tumor microenvironment may favor immune priming in situ, thus converting the tumor into a vaccine reservoir without perturbing immune reactivity to most organ-associated self-antigens. This type of strategies to focus immunity to TAA should lead to a safer and more effective vaccine regimen.

Concluding remarks
Her-2 DNA vaccine progressed from a lab innovation to a test agent in clinical trials within a decade. With the available immune modulating tools to complement vaccination, there is optimism that Her-2 vaccine will become a reality. It will be prudent to consider potential side effect at this time, with autoimmunity as the primary concern, and to design counter measures. Although both tumor immunity and autoimmunity are immune responses to self-antigens, the pathology of autoimmunity may not equal the mechanisms of tumor rejection, thus the opportunity to dampen one without compromising the other. It may be further advantageous to deliver immune modulating agents directly into the tumor to exploit the reservoir of tumor antigens in situ, without confronting the entire immune system. Finally, the experience and insight from developing Her-2 vaccine should guide the design of the next vaccine. Surface molecules expressed in abundance and with critical functions, such as Her-2, are desirable targets, whether the molecules are expressed by tumor cells or stromal cells. With the available knowledge and technology, much will be revealed in the next decade and decisive answers to cancer vaccines can be expected.
References
Hung MC, Lau YK (1999) Basic science of HER-2/neu: a review. Semin Oncol 26(12 Suppl 4):51–59
Slamon DJ, Godolphin W, Jones LA et al (1989) Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science 244:707–712
Ben-Levy R, Paterson HF, Marshall CJ et al (1994) A single autophosphorylation site confers oncogenicity tothe Neu/ErbB-2 receptor and enables coupling to the MAP kinase pathway. EMBO J 13:3302–3311
Wada T, Qian XL, Greene MI (1990) Intermolecular association of the p185neu protein and EGF receptor modulates EGF receptor function. Cell 61:1339–1347
Wei WZ, Shi WP, Galy A et al (1999) Protection against mammary tumor growth by vaccination with full-length, modified human ErbB-2 DNA. Int J Cancer 81:748–754
Romond EH, Perez EA, Bryant J et al (2005) Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med 353:1673–1684
Pilon SA, Piechocki MP, Wei WZ (2001) Vaccination with cytoplasmic ErbB-2 DNA protects mice from mammary tumor growth without anti-ErbB-2 antibody. J Immunol 167:3201–3206
Kiessling R, Wei WZ, Herrmann F et al (2002) Cellular immunity to the Her-2/neu protooncogene. Adv Cancer Res 85:101–144
Piechocki MP, Pilon SA, Wei WZ (2002) Quantitative measurement of anti-ErbB-2 antibody by flow cytometry and ELISA. J Immunol Methods 259:33–42
Pilon SA, Kelly C, Wei WZ (2003) Broadening of epitope recognition during immune rejection of ErbB-2-positive tumor prevents growth of ErbB-2-negative tumor. J Immunol 170:1202–1208
Piechocki MP, Ho YS, Pilon S et al (2003) Human ErbB-2 (Her-2) transgenic mice: a model system for testing Her-2 based vaccines. J Immunol 171:5787–5794
Lindencrona JA, Preiss S, Kammertoens T et al (2004) CD4+ T cell-mediated HER-2/neu-specific tumor rejection in the absence of B cells. Int J Cancer 109:259–264
Wei WZ, Morris GP, Kong YM (2004) Anti-tumor immunity and autoimmunity: a balancing act of regulatory T cells. Cancer Immunol Immunother 53:73–78
Miller F, Jones RF, Jacob J et al (2004) From breast cancer immunobiology to her-2 DNA vaccine and autoimmune sequelae. Breast Dis 20:43–51
Wei WZ, Jacob JB, Zielinski JF et al (2005) Concurrent induction of antitumor immunity and autoimmune thyroiditis in CD4+ CD25+ regulatory T cell-depleted mice. Cancer Res 65:8471–8478
Jacob J, Radkevich O, Forni G et al (2006) Activity of DNA vaccines encoding self or heterologous Her-2/neu in Her-2 or neu transgenic mice. Cell Immunol 240:96–106
Piechocki MP, Pilon SA, Wei WZ (2001) Complementary antitumor immunity induced by plasmid DNA encoding secreted and cytoplasmic human ErbB-2. J Immunol 167:3367–3374
Jacob JB, Kong YM, Meroueh C et al (2007) Control of Her-2 tumor immunity and thyroid autoimmunity by MHC and regulatory T cells. Cancer Res 67:7020–7027
Ursini-Siegel J, Schade B, Cardiff RD et al (2007) Insights from transgenic mouse models of ERBB2-induced breast cancer. Nat Rev Cancer 7:389–397
Rovero S, Amici A, Carlo ED et al (2000) DNA vaccination against rat her-2/Neu p185 more effectively inhibits carcinogenesis than transplantable carcinomas in transgenic BALB/c mice. J Immunol 165:5133–5142
Piechocki MP, Yoo GH, Dibbley SK et al (2007) Breast cancer expressing the activated HER2/neu is sensitive to gefitinib in vitro and in vivo and acquires resistance through a novel point mutation in the HER2/neu. Cancer Res 67:6825–6843
Shimizu J, Yamazaki S, Sakaguchi S (1999) Induction of tumor immunity by removing CD25+CD4+ T cells: a common basis between tumor immunity and autoimmunity. J Immunol 163:5211–5218
Reilly RT, Gottlieb MB, Ercolini AM et al (2000) HER-2/neu is a tumor rejection target in tolerized HER-2/neu transgenic mice. Cancer Res 60:3569–3576
Singh R, Paterson Y (2007) In the FVB/N HER-2/neu transgenic mouse both peripheral and central tolerance limit the immune response targeting HER-2/neu induced by Listeria monocytogenes-based vaccines. Cancer Immunol Immunother 56:927–938
Bos R, van DS, van HT et al (2005) Expression of a natural tumor antigen by thymic epithelial cells impairs the tumor-protective CD4+ T-cell repertoire. Cancer Res 65:6443–6449
Gallo P, Dharmapuri S, Nuzzo M et al (2005) Xenogeneic immunization in mice using HER2 DNA delivered by an adenoviral vector. Int J Cancer 113:67–77
Pupa SM, Iezzi M, Di CE et al (2005) Inhibition of mammary carcinoma development in HER-2/neu transgenic mice through induction of autoimmunity by xenogeneic DNA vaccination. Cancer Res 65:1071–1078
Tegerstedt K, Lindencrona JA, Curcio C et al (2005) A single vaccination with polyomavirus VP1/VP2Her2 virus-like particles prevents outgrowth of HER-2/neu-expressing tumors. Cancer Res 65:5953–5957
Huang W, Kukes GD (1999) Hashimoto’s thyroiditis: an organ-specific autoimmune disease-pathogenesis and recent developments. Lab Invest 79:1175–1180
Canonica GW, Cosulich ME, Croci R et al (1984) Thyroglobulin-induced T-cell in vitro proliferation in Hashimoto’s thyroiditis: identification of the responsive subset and effect of monoclonal antibodies directed to Ia antigens. Clin Immunol Immunopathol 32:132–141
Vaidya B, Kendall-Taylor P, Pearce SHS (2002) Genetics of endocrine disease: the genetics of autoimmune thyroid disease. J Clin Endocrinol Metab 87:5385–5397
Kong YM, Lomo LC, Motte RW et al (1996) HLA-DRB1 polymorphism determines susceptibility to autoimmune thyroiditis in transgenic mice: definitive association with HLA-DRB1*0301 (DR3) gene. J Exp Med 184:1167–1172
Kong YM, David CS, Lomo LC et al (1997) Role of mouse and human class II transgenes in susceptibility to and protection against mouse autoimmune thyroiditis. Immunogenetics 46:312–317
Vladutiu AO, Rose NR (1971) Autoimmune murine thyroiditis: relation to histocompatibility (H-2) type. Science 174:1137–1139
Larsen CE, Alper CA (2004) The genetics of HLA-associated disease. Curr Opin Immunol 16:660–667
Levin L, Ban Y, Concepcion E et al (2004) Analysis of HLA genes in families with autoimmune diabetes and thyroiditis. Hum Immunol 65:640–647
Esquivel PS, Rose NR, Kong YM (1977) Induction of autoimmunity in good and poor responder mice with mouse thyroglobulin and lipopolysaccharide. J Exp Med 145:1250–1263
Elrehewy M, Kong YM, Giraldo AA et al (1981) Syngeneic thyroglobulin is immunogenic in good responder mice. Eur J Immunol 11:146–151
McNeel DG, Knutson KL, Schiffman K et al (2003) Pilot study of an HLA-A2 peptide vaccine using flt3 ligand as a systemic vaccine adjuvant. J Clin Immunol 23:62–72
Disis ML, Rinn K, Knutson KL et al (2002) Flt3 ligand as a vaccine adjuvant in association with HER-2/neu peptide-based vaccines in patients with HER-2/neu-overexpressing cancers. Blood 99:2845–2850
Shevach EM (2000) Regulatory T cells in autoimmmunity. Annu Rev Immunol 18:423–449
Kong YM, Giraldo AA, Waldmann H et al (1989) Resistance to experimental autoimmune thyroiditis: L3T4+ cells as mediators of boththyroglobulin-activated and TSH-induced suppression. Clin Immunol Immunopathol 51:38–54
Sakaguchi S, Sakaguchi N, Asano M et al (1995) Immunologic self-tolerance maintained by activated T cells expressing IL-2 receptor alpha-chains CD25). Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. J Immunol 155:1151–1164
Morris GP, Chen L, Kong YM (2003) CD137 signaling interferes with activation and function of CD4+CD25+ regulatory T cells in induced tolerance to experimental autoimmune thyroiditis. Cell Immunol 226:20–29
Morris GP, Yan Y, David CS et al (2005) H2A- and H2E-derived CD4+CD25+ regulatory T cells: a potential role in reciprocal inhibition by class II genes in autoimmune thyroiditis. J Immunol 174:3111–3116
Morris GP, Kong YM (2006) Interference with CD4(+)CD25(+) T-cell-mediated tolerance to experimental autoimmune thyroiditis by glucocorticoid-induced tumor necrosis factor receptor monoclonal antibody. J Autoimmun 26:24–31
Maker AV, Attia P, Rosenberg SA (2005) Analysis of the cellular mechanism of antitumor responses and autoimmunity in patients treated with CTLA-4 blockade. J Immunol 175:7746–7754
Blansfield JA, Beck KE, Tran K et al (2005) Cytotoxic T-lymphocyte-associated antigen-4 blockage can induce autoimmune hypophysitis in patients with metastatic melanoma and renal cancer. J Immunother 28:593–598
Attia P, Phan GQ, Maker AV et al (2005) Autoimmunity correlates with tumor regression in patients with metastatic melanoma treated with anti-cytotoxic T-lymphocyte antigen-4. J Clin Oncol 23:6043–6053
Maker AV, Phan GQ, Attia P et al (2005) Tumor regression and autoimmunity in patients treated with cytotoxic T lymphocyte-associated antigen 4 blockade and interleukin 2: a phase I/II study. Ann Surg Oncol 12:1005–1016
Robinson MR, Chan CC, Yang JC et al (2004) Cytotoxic T lymphocyte-associated antigen 4 blockade in patients with metastatic melanoma: a new cause of uveitis. J Immunother 27:478–789
Phan GQ, Yang JC, Sherry RM et al (2003) Cancer regression and autoimmunity induced by cytotoxic T lymphocyte-associated antigen 4 blockade in patients with metastatic melanoma. Proc Natl Acad Sci USA 100:8372–8377
Rose NR, Bacon LD, Sundick RS et al (1977) Genetic regulation in autoimmune thyroiditis. In: Talal N (ed) Autoimmunity: genetics, immunologic, virologic, and clinical aspects. Academic Press, New York, pp 63–87
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is a symposium paper from the conference “Progress in Vaccination against Cancer 2007 (PIVAC 7)”, held in Stockholm, Sweden, on 10–11 September 2007.
Rights and permissions
About this article
Cite this article
Wei, WZ., Jacob, J., Radkevich-Brown, O. et al. The “A, B and C” of Her-2 DNA vaccine development. Cancer Immunol Immunother 57, 1711–1717 (2008). https://doi.org/10.1007/s00262-008-0464-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-008-0464-y