Abstract
The innovative techniques in ultrasound have added a new dimension to investigating superficially located areas such as the contents of the scrotal sac. High frequency transducers, improved technology with the addition of elastography, contrast enhanced ultrasound and microvascular imaging has resulted in a further improvement in diagnostic capabilities. The ability to clearly demonstrate the presence or absence of vascularity within the area under investigation adds an additional dimension to operator confidence in establishing the presence of infarction, global or segmental, or the walls and cavity of an abscess in the testis or epididymis. Increased vascularity of a tumor aids the differential diagnosis based on the flow dynamics of the microbubble contrast, benign lesions likely to retain contrast. Elastography has the ability to ascertain the stiffness of tissue, and when used in conjunction with other ultrasound methods adds to the understanding of the likelihood of a malignant abnormality being present. All the different techniques come under the umbrella term ‘multiparametric ultrasound’, with the application in the scrotal sac detailed in this article.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The ability of ultrasound to assess the superficial structure is unique, with high frequency transducers providing high resolution imaging, with recent advances in transducer technology coupled with advances in ultrasound techniques, termed multiparametric ultrasound, improving the imaging capabilities [1], transforming the ability to assess scrotal contents. High frequency, and with it better resolution, combined with broadband capabilities renders ultrasound assessment of scrotal contents the first line and often only imaging technique needed for diagnosis. Earlier addition of color and spectral Doppler techniques to the conventional B-mode ultrasound, were useful in assessing vascularity of focal lesions, inflammation and the extent of vascularity in the traumatized testis and added important information to the examination, particularly in assessing epididymal inflammation and the possibility of spermatic cord torsion [2,3,4]. Newer ultrasound techniques, including microvascular imaging (MVI) [5] elastography [6, 7] and contrast enhanced ultrasound (CEUS) [8] has further improved capabilities for the assessment of the scrotum [9]. Recent guidelines for the use of these newer ultrasound techniques, allows for the incorporation into clinical practice for better patient care [10,11,12].
The article will describe the application of ultrasound to the diagnosis of scrotal disease, by assessing presenting symptoms and clinical scenarios, incorporating new ultrasound techniques to allow for confident diagnosis and patient management without recourse to other imaging techniques. The use of all these methods in an ultrasound examination is ascribed to an umbrella term of multiparametric ultrasound (MPUS) [1].
Newer techniques in ultrasound
Contrast enhanced ultrasound
The most widely used microbubble contrast agent for the assessment of scrotal disease is Lumason™/SonoVue™ (Bracco SpA, Milan), used off license when applied to the scrotal contents but with justification and supported by regulatory authorities, when beneficial to the patient [13]. The examination requires a full dose of the microbubble agent (normally 4.8mls of Lumason™/SonoVue™), as the physics of the harmonic response of the microbubble is governed by the acoustic properties in the insonating ultrasound field, with the smaller microbubbles required to interact with the higher frequency beam found at a smaller concentration in the injected dose [14, 15]. The technique is a natural extension of a liver CEUS examination, with the advantage of absence of movement of the scrotal contents. The important aspect of a CEUS examination in the scrotum is the arterial phase, with meaningful information obtained within 2 min of injection. With new software available the possibility to use multiple intensity projection methods of summation of the signal is useful, as often the intensity of the enhancement in the non-inflamed testis is limited. The appraisal of the vascularity of a focal intra-testicular lesion often requires the addition of time intensity curves for assessment of the perfusion and washout of these lesions [16, 17]. The ability to distinguish vascularized from non-vascularized components of the scrotal contents is key to the success of a CEUS examination, often improving the diagnostic yield of the ultrasound examination as establishing avascular tissue is paramount for the interpretation [11, 12]. Areas of infarction or abscess content will be readily identified, as absence of flow is clearly depicted. The excellent capabilities of CEUS to depict vascular flow to the capillary level combined with the novelty of being a truly intravascular contrast agent without leaking into the extra-vascular space, a hallmark of other imaging contrast agents, allows for confidence to interpret absent flow.
Elastography
The ability to assess the stiffness of tissue is the basis of tissue elastography, and represents the “surgeon’s” hand when assessing scrotal abnormalities. The hallmark of malignant tissue is increased stiffness, potentially allowing for the differentiation of benign and malignant lesions within the testis parenchyma and out with the clinical examination. There are two methods of elastography in clinical use. Strain elastography, where pressure applied by the transducer is converted to a color map of stiffness, with a strain ratio applied between normal and abnormal tissue. The other method, shear wave elastography, which does not require external transducer pressure, has predominantly been used in the assessment of liver stiffness as a measure of liver fibrosis [18]. With shear wave elastography the ultrasound transducer generates a shear wave which can quantify stiffness in m/sec or kPa. This can be quantified using point shear wave elastography or 2-D elastography where a volume measurement is obtained, color coded, and region of interest drawn at the site of measurement [10] Elastography measurements, well established in assessing liver disease, are commonly used clinically in the assessment of breast and thyroid abnormalities [10, 19]. The use of strain elastography color maps have been investigated more thoroughly in the assessment of intra-testicular lesions, whereas the measurement of shear wave velocities have been used predominantly in the testis parenchyma in infertility [20, 21]. There is no specific advantage of either technique, with color mapping giving a visual overview, which aids interpretation. There is considerable overlap in the reported values for the measurement of stiffness in different testicular conditions, with a reported range for the normal testis of between 2.0 and 2.9 kPa (median 2.4 kPa) and oligoasthenoteratospermia between 1.8 and 2.5 kPa (median 2.1 kPa) [22].
s.
Microvascular imaging
The development of Doppler US techniques has developed considerably, with the newest technique of increased sensitivity with reduction of artifacts, termed microvascular imaging, showing great promise in many areas [5]. Applications in the scrotal sac are not well documented, but with potential in many areas where vascularity is paramount to the diagnosis. This may be a useful tool when evaluating the presence of vascularity in a focal intra-testicular lesion, prior to the application of microbubble contrast. Movement artifact is an issue with microvascular techniques, with interrogation of the scrotal sac less problematic with absence of respiratory movement and a superficial location.
Clinical applications
A description of the various abnormalities in the scrotal sac suitable for a multiparametric ultrasound examination will be detailed according to clinical scenarios. The European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) guidelines on the use of CEUS for the testis, limits the application to some well-defined investigations; (i) detailing the presence or absence of vascularity in focal testicular tumors, (ii) ascertaining viable tissue in trauma, (iii) detailing the extent of a segmental infarction and (iv) ascertaining the configuration and site of an abscess [11]. Tissue elastography has a limited role as a stand-alone technique in the testis, and EFSUMB recommends that this technique should be used in conjunction with other ultrasound techniques when evaluating testicular abnormalities [10].
Scrotal pain
Scrotal pain may be chronic, low level and often related to the presence of a varicocele, or acute and presenting as a surgical emergency, with spermatic cord torsion a consideration in the appropriate clinical setting. The patients age is crucial to the underlying cause, as is a detailed clinical history. Testicular tumors rarely present with pain, although this will be the anxiety of the person presenting with symptoms. Ultrasound is the imaging technique of choice and the addition of the many newly available techniques improve the diagnosis and management.
Spermatic cord torsion
This most often presents at the onset of puberty as the testicular volume increases, and is thought to be associated with the bell clapper deformity, although the prevalence of this deformity is far higher than the incidence of spermatic cord torsion [23]. The hallmark of the clinical symptoms is the sudden onset of pain, which is relentless, and constitutes a surgical emergency [24]. The time dependent testis salvage rate requires emergent surgery, and unless ultrasound is readily available, imaging should not delay surgery. Ultrasound is useful in determining the absence or presence of testicular color Doppler flow, or the presence of epididymitis or orchitis [25,26,27]. Absence of flow on color Doppler is considered the “standard” for the presence of a spermatic cord torsion, but this has a number of pitfalls; observer experience, ability to perform the examination accurately in the presence of severe pain, technical limitations of the equipment and importantly, intermittent spermatic cord torsion may present with normal color Doppler flow [3]. The addition of CEUS alters the confidence in establishing the absence of flow; areas of infarction will be clearly depicted [28]. The CEUS examination is particularly useful for a “missed” torsion when the patient presents days after the acute episode, with diminished pain, but an enlarged heterogenous testis, with poor color Doppler signal; absence of flow is unequivocal on CEUS [29]. The addition of tissue elastography in the pathway for assessing spermatic cord torsion has limitations and varies according to the duration of ischemic changes, but may have a role in the acute stages when there is intermittent blood flow compromise [30] (Fig. 1).
Presentation following several days of testicular pain in an 18 year old; spermatic cord torsion. A B-mode transverse view of the testis, demonstrating an enlarged heterogenous left testis (arrow). B Tissue elastography demonstrates a heterogenous color map, predominantly blue, which indicates increased stiffness (arrow). C A contrast enhanced ultrasound examination, using maximum intensity projection, confirms absence of flow in the left testis (arrow), confirming a “missed” spermatic cord torsion
Segmental infarction
An area of segmental infarction in the testis has no specific pre-disposing factors, may be related to infection, sickle cell disease, vasculitis or idiopathic, affecting an older age group than that of spermatic cord torsion [4, 31]. Color Doppler flow is normally absent, and visualized more accurately on MVI, but clearly depicted on the CEUS examination [32, 33] (Fig. 2). In the presence of severe epididymitis, venous drainage from the testis may be compromised, resulting in areas of segmental infarction, and in some severe cases, complete testicular infarction [34, 35] (Fig. 3). Conservative clinical management is advocated for areas of segmental infarction, early use of CEUS will allow confident diagnosis with follow-up advocated when areas of avascular tissue on CEUS reason against the presence of tumor, and elastography changes will mimic the changes in tissue stiffness over a time period [33].
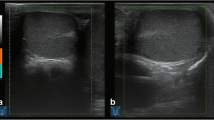
Presentation with acute testicular discomfort in a 62 year old; segmental testicular infarction. A B-mode longitudinal view of the left testis demonstrating a irregular focal lesion in the lower aspect of the testis (arrow). B Microvascular imaging shows color surrounding the lesion with possible internal faint color Doppler flow (arrow). C Tissue elastography demonstrates a mixed stiffness lesion, predominantly of increased stiffness (arrow); this will evolve over time. D The contrast enhanced ultrasound examination confirms an avascular lesion with surrounding hyperemia (arrow)
Acute and severe epididymitis and venous infarction of the left testis in a 58 year old. A The B-mode transvers view demonstrates the left testis (arrow) with a septations in a pyocoele (small arrows) in a patient with severe pain and underlying epididymitis. B The microvascular imaging image does not demonstrate any color flow in the left testis (arrow). C On the contrast enhanced ultrasound examination, with a maximum intensity projection, the right testis is adequately perfused (arrow) whilst the left testis (star) has no perfusion following global infarction associated with severe epididymitis
Infection
The presence of uncomplicated epididymitis is a clinical diagnosis and readily responds to medical treatment without resorting to imaging. Intractable symptoms whist on treatment warrants imaging [36]. The ability to differentiate orchitis, epididymitis and epididymis-orchitis is readily ascertained on ultrasound imaging and may alter management strategy [37]. Complications that arise that benefit from MPUS include abscess formation, both within the epididymis or in an intra-testicular location (Fig. 4), segmental infarction and global venous infarction [38, 39]. Color Doppler ultrasound and MVI will depict the hyperemic borders of an abscess, with an echo-poor center adequately, but the addition of CEUS will depict clear separation of viable and non-viable tissue, and allow for serial follow-up to resolution or expediate surgical intervention. Septations within an abscess cavity or within a chronic pyocoele may be seen with a CEUS examination. The presence of an echogenic pyocoele may obscure the underlying testis, and testicular viability can be assessed using CEUS. Serial elastography of an abscess will depict changes that vary with the resolution, and liquefication will be recognized on elastography with the classic ‘blue-green-red’ sign [40, 41]. Orchitis demonstrates a variable appearance on ultrasound, often with areas of low reflectivity, as infarcted areas interspersed with viable infective parenchyma [42], with CEUS and MVI adding further vascular information, and elastography demonstrating increased testis stiffness. An ‘end-stage’ complication of severe epididymitis is the development of venous outflow obstruction, a consequence of oedema and occlusion of the veins draining the testis, resulting in global venous testicular infarction [35].
Focal abscess in the right testis in a 42 year old, following severe epididymitis. A Oblique view on B-mode ultrasound demonstrates a heterogenous focal lesion in the inferior aspect of the right testis (arrow). B Color Doppler ultrasound demonstrates an avascular area with some increased flow around the peripheral aspect of the lesion (short arrows). C Contrast enhanced ultrasound demonstrates the abscess cavity as an avascular area, with enhancement of a septation (long arrow). There is a second pocket of abscess formation demonstrated (arrowhead)
Torsion of an appendix testis
There are four testicular appendages present, two of which are visible on an ultrasound examination; the testis appendix and the epididymal appendix, with variation in size and appearance, and when cystic is known as the Hydatid of Morgagni [43]. Torsion of an appendix usually occurs in the pre-adolescent boy, and is an important differential for acute testicular pain, as management is conservative [44, 45]. Although color Doppler is used to ascertain loss of blood supply, CEUS has been reported in a case series to be of benefit to ascertain the perfusion to improve imaging diagnosis [46].
Scrotal lumps
Intratesticular tumors
The presentation of a malignant testicular tumour follows the detection of a ‘lump’ by the patient whilst self-examining, and invariably the vast majority of palpable testicular tumors are malignant germ cell tumors, classical seminomas the most common. Orchidectomy is the standard management of the large tumors, with staging by whole body CT and assessment of biochemical tumour markers [47]. Presently a number of focal testicular lesions are detected following an ultrasound for an unrelated reason, and these incidental lesions are nearly always benign, up to 80% [48]. The dilemma is to ensure that an unnecessary orchidectomy is not performed with benign disease [49], with recommendations directed towards using MPUS to ascertain the nature of the lesion to prevent this occurring [16, 50, 51]. The guidelines from EFSUMB indicate that applying CEUS and elastography to focal indeterminate lesions of the testis should be used in combination with B-mode and color Doppler techniques for a comprehensive diagnosis [11]. The current suggestion is that CEUS assessment of a malignant lesion is likely to demonstrate less intense enhancement and early washout (Fig. 5), whereas the benign lesions of Leydig cell hyperplasia (Fig. 6) are more intensely enhancing, with prolonged washout [16, 17, 52, 53]. The application of elastography as a stand-alone technique is more varied, and this has been demonstrated in recent studies with much overlap between benign and malignant lesions [7, 54], although early studies were more optimistic [55,56,57]. The combination of techniques is more accurate in establishing the diagnosis [58]. An example of this is the benign epidermoid cyst, a true cyst, which is avascular on color Doppler ultrasound, demonstrates no enhancement with CEUS but is of increased stiffness on elastography (Fig. 7) [59]. This is different from the rare intra-testicular adrenal rest tumors seen in congenital adrenal hyperplasia, where the focal lesion mimics a germ cell tumour, with increased vascularity, increased stiffness and marked enhancement on CEUS; a clinical history is vital (Fig. 8) [60]. Recent multi-center follow-up study on the management of the incidental discovered < 1 cm lesion may be safely followed up looking for incremental growth; >2 mm in 6 months suggests malignancy, although there is some overlap with benign lesions [61].
Stage 1 seminoma in a 51-year old. A Transverse view B-mode ultrasound of the testes demonstrating afocal heterogenous lesion in the right testis (arrow). B Longitudinal color Doppler view of the lesion showing intra-lesional color Doppler flow (arrows). C Tissue elastography demonstrates increase stiffness of the lesion, which is predominantly blue (arrows). D A contrast enhanced ultrasound examination demonstrating enhancement of the focal lesion (arrows) with a pocket of avascularity corresponding to an area of tumor necrosis
Incidental lesion in a 54 year old imaged for non-specific testicular pain. Testis sparing surgery with excision of the lesion showed Leydig cell hyperplasia. A A longitudinal image of the right testis demonstrating a 4 mm low reflective lesion (arrow). B The color Doppler image indicates increased vascularity of the focal lesion (arrow). C On the microvascular imaging there is intense vascularization present (arrow). D The tissue elastography image shows that the lesion is not stiffer than the surrounding normal tissue (arrows). E A contrast enhanced ultrasound examination, with maximum intensity projection, demonstrates a highly vascular lesion (arrow) that retains microbubble contrast at 90 s post contrast injection
A 46-year-old with a right testicular lump, with a epidermoid cyst. A A longitudinal image of the right testis, with a heterogenous (arrow) occupying the central aspect of the testis, with an echogenic border, and areas of calcification. B The microvascular image demonstrating color flow (arrow) around the heterogenous lesion but no internal flow. C The tissue elastography image shows that the lesion is stiffer than the surrounding normal tissue (arrows). D A contrast enhanced ultrasound examination shows an avascular epidermoid cyst (large arrow) with artifact (small arrows) of high reflectivity from echogenic areas; there is no vascular flow present
A 18-year old with known congenital adrenal hyperplasia undergoing screening ultrasound of the testis with bilateral adrenal rest cells noted. A Longitudinal view of the right testis on B-mode demonstrating a focal low reflective intra-testicular tumor (arrow) mimicking a primary germ cell tumor. B The microvascular image demonstrating color flow (arrow) within the tumor, disordered and intense in comparison to the normal testis parenchyma. C The tissue elastography image shows that the lesion is stiffer than the surrounding normal tissue (arrows). D A contrast enhanced ultrasound examination, with maximum intensity projection, demonstrates a highly vascular lesion (arrow)
The rare presentation of intra-testicular lymphoma may also be interrogated with MPUS; B-mode images demonstrate low reflective lesions which may be bilateral, with increase color Doppler flow [62], with the addition of elastography demonstrating increased stiffness, and CEUS demonstrating linear non-branching vessels with early washout [63].
Intratesticular abscess formation is seen less often, and is normally a consequence of severe epididymo-orchitis, and the CEUS examination reflects the avascular components of areas of necrosis and surrounding increased enhancement form the inflamed abscess wall, with septations noted [9, 34] (Fig. 4). Chronic non-pyogenic abscesses and pseudo tumors may be difficult to diagnose with confidence on MPUS [64, 65].
Extra testicular
In the adult nearly all extra-testicular abnormalities are benign, with epididymal abscess formation (Fig. 9) following infection the most common painful focal lesion, and with painless lesions most commonly cystic or a spermatocele, and with solid lesions likely a lipoma (Fig. 10) or an adenomatoid tumour [66, 67]. The application of MPUS in extra-testicular lesions adds information, with B-mode findings alone nearly always diagnostic. Rarely is an extra-testicular lesion in the adult a malignant rhabdomyosarcoma or a mesothelioma, with presentation as a painless mass [68]. In children, an extra-testicular lesion is often a rhabdomyosarcoma and warrants urgent investigation.
Epididymal abscess in a 56 year old. A Longitudinal view of the right testis demonstrating an echogenic lesion in the epididymal tail (arrow)in epididymitis, with surrounding increase in color Doppler signal. B A contrast enhanced ultrasound examination demonstrates no vascularization in the center of the lesion (arrow) with increased contrast enhancement surrounding the avascular cavity confirming an epididymal abscess
Palpable mass in the left epididymis in a 48-year old, with characteristics of a benign lipoma. A A longitudinal B-mode image of the left testis demonstrating an echogenic lesion in the epididymis (arrow). B Microvascular imaging demonstrates some vascular flow in the periphery of the lesion, but no central flow (arrow). C On elastography the echogenic lesion demonstrates increased stiffness (arrows). D On the contrast enhanced ultrasound examination, internal microbubble signal is observed (arrow) indicating some vascularization of the lipoma
Inguinal lesions
The presence of an undescended inguinal testis can be documented in adult patients and an ultrasound examination is often confirmatory. The addition of color Doppler techniques will confirm viability of the testis, and addition of CEUS in patients with recent pain, establishes the possibility of vascular compromise [69]. An inguinal spermatic cord mass in an adult is rare, and abnormalities of the spermatic cord may arise at this site, sometimes benign, a cavernous hemangioma or with leiomyosarcomas reported [70,71,72,73]. The presence of abnormal color Doppler flow alerts the examiner to possibility of malignancy, with increased stiffness on elastography a hallmark of malignancy [74].
Trauma
Trauma to the scrotal sac is invariably a result of a sporting injury or a motor vehicle injury in a young man [75]. The contents of the scrotal sac may be involved, with testicular fracture and rupture most concerning, with an intact tunica albuginea essential to testicular viability; rupture requires surgical correction [76, 77]. Epididymal rupture and tears also occur and often require surgical management [78, 79]. An isolated intra-testicular hematoma may ensue, and may also be iatrogenic from a testicular biopsy procedure.
Intra-testicular hematoma
The presence of a hematoma is readily identified on an ultrasound examination, and is often seen in the context of recent blunt scrotal trauma [80]. With trivial or forgotten trauma, confusion with a primary germ cell tumour is a possibility, and the importance of MPUS in establishing the benign nature of the lesion, allowing conservative management is recognized [81]. The ability of a CEUS examination to exclude the presence of vascularity in the lesion, and the use of elastography to exclude increased stiffness, allows for serial examinations to demonstrate regression of the lesion [82, 83]. This avoids an unnecessary orchidectomy. Following testicular biopsy, usually for investigation of infertility, monitoring a complicating hematoma with MPUS, alleviates both patient and physician anxiety (Fig. 11).
Post-biopsy pain, biopsy performed for investigation of infertility in a 45 year old, with an intra-testicular hematoma and arterio-venous fistula. A A transverse image on B-mode, demonstrating a focal low reflective lesion in the mid aspect of the left testis (long arrow). The biopsy tract is seen as a linear low reflective area (short arrow). B An oblique color Doppler ultrasound showing the presumedhaematoma (short arrow), with increased flow (long arrow) in a arterio-venous fistula. C On elastography the stiffness is intermediate (arrows), and will evolve with the stage of the liquefication of the hematoma. D On the contrast enhanced ultrasound examination, the hematoma (short arrow) is clearly depicted, with the arterio-venous fistula obvious (long arrow)
Testicular fracture
The B-mode ultrasound often depicts the site of rupture of the tunica albuginea, with herniation of testicular tissue, allowing for targeted surgical repair. The viability of the underlying testis on color Doppler US alone is not conclusive, and adding a CEUS examination clearly depicts the viable perfused testicular tissue [84]. A CEUS examination could dictate the possibility of a partial orchidectomy to preserve viable testicular tissue and future fertility prospects [85].
Epididymal trauma
B-mode ultrasound will evaluate the epididymis in trauma with the addition of color Doppler ascertaining the vascularity. Addition of CEUS allows for the identification of a hematoma, extent of the epididymal injury and will allow for confident management [75].
Testicular microlithiasis
There has been extensive interest in the epidemiology of testicular microlithiasis and the association with primary germ cell tumors of the testis, with debate on the association and the need for ultrasound surveillance [86,87,88]. Studies on the application of elastography in testicular microlithiasis have demonstrated slight increase in stiffness compared with the normal testis, but less than in the presence of a germ cell tumor [89]. There is no role for color Doppler ultrasound in testicular microlithiasis. Areas of macrocalcification are occasionally encountered, may be associated with a higher prevalence of tumors that microlithiasis [90], and may demonstrate the “twinkle” artifact on color Doppler ultrasound [91]. The B-mode appearances are well documented, and subtle areas of limited testicular microlithiasis may be better depicted using a technique that accentuates areas of calcification, more often used for subtle calcification seen on breast ultrasound (Fig. 12).
Longitudinal images of the left testis, with classical microlithiasis. The MicroPure™ (Canon Medical Systems) demonstrates the areas of microlithiasis within the testis (arrows) with background suppression, making the testicular microlithiasis more obvious. A primary germ cell tumor is present (star)
Conclusion
The addition of the newer ultrasound techniques, including elastography and CEUS add another dimension to the evaluation of scrotal diseases. The ability to ascertain the presence or absence of vascularity on a CEUS examination is crucial in establishing the viability of the testicular or epididymal tissue, identifying a hematoma or abscess or establishing a infarction. Assessment of the pattern of enhancement of a neoplastic lesion of the testis can differentiate the benign from the malignant neoplastic testicular lesion, allowing testis sparing surgery, watchful waiting and in the clinical context, preserves fertility [92]. The combination with elastography gives added information, with a caveat that no US technique should be used as a stand-alone imaging technique but the combination will yield a more comprehensive outcome in terms of diagnosis and management both in the adult and pediatric patient [9, 93].
Data availability
No datasets were generated or analysed during the current study.
References
Sidhu PS (2015) Multiparameteric ultrasound (MPUS) imaging: Terminology describing the many aspects of ultrasonography. Ultraschall in Med 36:315–317
Sidhu PS (1999) Clinical and imaging features of testicular torsion: role of ultrasound. Clinical Radiology 54:343–352
Bertolotto M, Salomon G, Pavan N et al (2023) Testicular torsion: an avascular testis at color Doppler ultrasound is not enough to prove the diagnosis. Minerva Urol Nephrol 75:289–296
Bilagi P, Sriprasad S, Clarke JL, Sellars ME, Muir GH, Sidhu PS (2007) Clinical and ultrasound features of segmental testicular infarction: Six-year experience from a single centre. European Radiology 17:2810–2818
Aziz MU, Eisenbrey JR, Deganello A et al (2022) Microvascular Flow Imaging: A State-of-the-Art Review of Clinical Use and Promise. Radiology 305:250–264
Fang C, Huang DY, Sidhu PS (2019) Elastography of focal testicular lesions: current concepts and utility. Ultrasonography 38:302–310
Konstantatou E, Fang C, Romanos O et al (2019) Evaluation of Intratesticular Lesions With Strain Elastography Using Strain Ratio and Color Map Visual Grading: Differentiation of Neoplastic and Nonneoplastic Lesions. Journal of Ultrasound in Medicine 38:223–232
Jaffer OS, Sidhu PS (2013) Contrast-enhanced ultrasonography of the testes. Ultrasound Clin North Am 8:509–523
Huang DY, Pesapane F, Rafailidis V, Deganello A, Sellars ME, Sidhu PS (2020) The role of multiparametric ultrasound in the diagnosis of paediatric scrotal pathology. British Journal of Radiology 93:20200063
Sâftoiu A, Gilja OH, Sidhu PS et al (2019) The EFSUMB Guidelines and Recommendations for the Clinical Practice of Elastography in Non-Hepatic Applications: Update 2018. Ultraschall in Med 40:425–453
Sidhu PS, Cantisani V, Dietrich CF et al (2018) The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Long Version). Ultraschall in Med 39:e2-e44
Sidhu PS, Cantisani V, Dietrich CF et al (2018) The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Short Version). Ultraschall in Med 39:154–180
Sidhu PS (2008) The EFSUMB guidelines for contrast-enhanced ultrasound are comprehensive and informative for good clinical practice: will radiologists take the lead? British Journal of Radiology 81:524–525
Burns PN, Hope Simpson D, Averkiou MA (2000) Nonlinear imaging. Ultrasound in Medicine and Biology 26:S19-S22
Wilson SR, Burns PN (2010) Microbubble-enhanced US in body imaging: What role? Radiology 257:24–39
Huang DY, Sidhu PS (2012) Focal testicular lesions: colour Doppler ultrasound, contrast-enhanced ultrasound and tissue elastography as adjuvants to the diagnosis. Br J Radiol 85:S41-S53
Isidori AM, Pozza C, Gianfrilli D et al (2014) Differential diagnosis of nonpalpable testicular lesions: qualitative and quantitave contrast-enhanced US of benign and malignant testicular tumors. Radiology 273:606–618
Dietrich CF, Bamber J, Berzigotti A et al (2017) EFSUMB Guidelines and Recommendations on the Clinical Use of Liver Ultrasound Elastography, Update 2017 (Short Version). Ultraschall in Med 38:377–394
Dietrich CF, Bamber J, Berzigotti A et al (2017) EFSUMB Guidelines and Recommendations on the Clinical Use of Liver Ultrasound Elastography, Update 2017 (Long Version). Ultraschall in Med 38:e16-e47
Illiano E, Trama F, Ruffo A et al (2021) Testicular shear wave elastography in oligo-astheno-teratozoospermic individuals: a prospective case-control study. Int Urol Nephrol 53:1773–1783
Roy C, de Marini P, Labani A, Leyendecker P, Ohana M (2020) Shear-wave elastography of the testicle: potential role of the stiffness value in various common testicular diseases. Clinical Radiology 75:560–560
Rocher L, Criton A, Gennisson JL et al (2017) Testicular Shear Wave Elastography in Normal and Infertile Men: A Prospective Study on 601 Patients. Ultrasound Med Biol 43:782–789
Caesar RE, Kaplan GW (1994) Incidence of bell-clapper deformity in an autopsy series. Pediatric Urology 44:114–116
Williamson RCN (1976) Torsion of the testis and allied conditions. British Journal of Surgery 63:465–476
Amaechi I, Sidhu PS (2008) Ultrasound in the assessment of the “on-call” acute scrotum. Imaging 20:131–138
Barloon TJ, Weissman AM, Kahn D (1996) Diagnostic imaging of patients with acute scrotal pain. American Family Physician 53:1734–1750
Hricak H, Lue TF, Filly RA, Alpers CE, Zeineh SJ, Tanagho EA (1983) Experimental study of the sonographic diagnosis of testicular torsion. Journal of Ultrasound in Medicine 2:349–356
Yamagucji A, Hayashi Y, Kojima Y, Miyagawa H, Ito M, Kohri K (2005) Testicular torsion: usefulness of contrast-enhanced power Doppler sonography. Int J Urol 12:849–851
Moschouris H, Stamatiou K, Lampropoulou E, Kalikis D, Matsaidonis D (2009) Imaging of the acute scrotum; is there a place for contrast-enhanced ultrasonography? Int Braz J Urol 35:702–705
Herek D, Herek O, Akbulut M, Ufuk F (2016) Role of strin elastography in the evaluation of testicular torsion. An experimental study. J Ultrasound Med 35:e75-e84
Sriprasad S, Kooiman GG, Muir GH, Sidhu PS (2001) Acute segmental testicular infarction: differentiation from tumour using high frequency colour Doppler ultrasound. Brit J Radiol 74:965–967
Bertolotto M, Derchi LE, Sidhu PS et al (2011) Acute segmental testicular infarction at contrast-enhanced ultrasound: early features and changes during follow-up. AJR Am J Roentgenol 196:834–841
Patel K, Huang DY, Sidhu PS (2014) Metachronous Bilateral Segmental Testicular Infarction: Multi-parametric Ultrasound imaging with Grey-scale Ultrasound, Doppler Ultrasound, Contrast Enhanced Ultrasound (CEUS) and Real-time Tissue Elastography (RTE). J Ultrasound 17:233–238
Lung PF, Jaffer OS, Sellars ME, Sriprasad S, Kooiman GG, Sidhu PS (2012) Contrast enhanced ultrasound (CEUS) in the evaluation of focal testicular complications secondary to epidiymitis. AJR Am J Roentgenol 199:W345-W354
Yusuf T, Sellars ME, Kooiman GG, Diaz-Cano S, Sidhu PS (2013) Global testicular infarction in the presence of epididymitis. Clinical features, appearances on grayscale, color Doppler, and contrat-enhanced sonography, and histologic correlation. J Ultrasound Med 32:175–180
Yusuf GT, Sidhu PS (2013) A review of ultrasound imaging in scrotal emergencies. J Ultrasound 16:171–178
Lung PF, Sidhu PS (2011) Role of ultrasound in the diagnosis of testicular lesions. Imaging Med 3:587–595
Drudi FM, Laghi A, Iannicelli E et al (1997) Tubercular epididymitis and orchitis: US patterns. European Journal of Radiology 7:1076–1078
Rencken RK, DuPlessis DJ, DeHaas LS (1990) Venous infarction of the testes - a cause of non-response to conservative therapy in epididymo-orchitis: a case report. South African Medical Journal 78:337–338
Ophir J, Cespedes I, Ponnekanti H, Yazdi Y, Li K (1991) Elastography: a quantitative method for imaging the elasticity of biological tissues. Ultrason Imaging 13:111–134
Ozturk A, Grajo JR, Dhyani M, Anthony BW, Samir AE (2018) Principles of ultrasound elastography. Abdominal Radiology
Cook JL, Dewbury K (2000) The changes seen on high-resolution ultrasound in orchitis. Clinical Radiology 55:13–18
Sellars MEK, Sidhu PS (2003) Utrasound appearances of the testicular appendages: pictorial review. Eur Radiol 13:127–135
Baldisserotto M, de Souza JCK, Pertence AP, Dora MD (2005) Color Doppler Sonography of Normal and Torsed Testicular Appendages in Children. American Journal of Roentgenology 184:1287–1292
Yang DM, Lim JW, Kim JE, Kim JH, Cho H (2005) Torsed Appendix Testis: Gray Scale and Color Doppler Sonographic Findings Compared With Normal Appendix Testis. Journal of Ultrasound in Medicine 24:87–91
Fukuzawa H, Minoda N, Okamoto M, Tsuruno Y, Watanabe A (2024) Contrast-enhanced ultrasonographic findings in torsion of the appendix testis or epididymis in children: a case series. J Med Ultrason (2001) 51:125–131
Patrikidou A, Cazzaniga W, Berney D et al (2023) European Association of Urology Guidelines on Testicular Cancer: 2023 Update. Eur Urol 84:289–301
Croghan SM, Malak JW, Rohan P et al (2023) Diagnosis and management of indeterminate testicular lesions. Nature Reviews Urology. https://doi.org/10.1038/s41585-023-00786-3
Scandura G, Verrill C, Protheroe A et al (2017) Incidentally detected testicular lesions < 10 mm in diameter: can orchidectomy be avoided? BJU International 121:575–582
Rocher L, Ramchandani P, Belfield J et al (2016) Incidentally detected non-palpable testicular tumours in adults at scrotal ultrasound: impact of radiological findings on management Radiologic review and recommendations of the ESUR scrotal imaging subcommittee. Eur Radiol 26:2268–2278
Shah A, Lung PF, Clarke JE, Sellars ME, Sidhu PS (2010) New Ultrasound Techniques for Imaging of the Indeterminate Testicular Lesion May Avoid Surgery Completely. Clin Radiol 65:496–498
Drudi FM, Valentino M, Bertolotto M et al (2016) CEUS time intensity curves in the differentiation between Leydig cell carcinoma nd seminoma: a multicenter study. Ultraschall in Med 37:201–205
Lock G, Schmidt C, Helmich F, Stolle E, Dieckmann K (2011) Early experience with contrast enhanced ultrasound in the diagnosis of testicular masses; a feasibility study. Urology 77:1049–1053
Pozza C, Gianfrilli D, Fattorini G et al (2016) Diagnostic value of qualitive and strain ratio elastography in the differential diagnosis of non-palpable testicular lesions. Andrology 4:1193–1203
Goddi A, Sacchi A, Magistretti G, Almolla J, Salvadore M (2012) Real-time elastography for testicular lesion assesment. Eur Radiol 22:721–730
Aigner F, De Zordo T, Pallwein-Prettner L et al (2012) Real-time sonoelastography for the evaluation of testicular lesions. Radiology 263:584–589
Marsaud A, Durand M, Raffaelli C et al (2015) Apport del Elastographie en temps reel pour la caractrisation des masses testiculaires. Proges en Urologie 25:82
Auer T, De Zordo T, Dejaco C et al (2017) Value of Multiparametric US in the Assessment of Intratesticular Lesions. Radiology 285:640–649
Patel K, Sellars ME, Clarke JL, Sidhu PS (2012) Features of testicular epidermoid cysts on contrast enhanced ultrasound and real time elastography. J Ultrasound Med 31:1115–1122
Mansoor NM, Huang DY, Sidhu PS (2022) Multiparametric ultrasound imaging characteristics of multiple testicular adrenal rest tumours in congenital adrenal hyperplasia. Ultrasound 30:80–84
Bertolotto M, Campo I, Freeman S et al (2024) Follow-up of non-palpable testicular incidentalomas under 1 cm: does growth rate differentiate malignant and non-malignant lesions? Eur Radiol. https://doi.org/10.1007/s00330-024-10981-4
Bertolotto M, Derchi LE, Secil M et al (2015) Grayscale and color Doppler features of testicular lymphoma. J Ultrasound Med 34:1139–1145
Kachramanoglou C, Rafailidis V, Philippidou M et al (2017) Multiparametric Sonography of Hematologic Malignancies of the Testis: Grayscale, Color Doppler, and Contrast-Enhanced Ultrasound and Strain Elastographic Appearances With Histologic Correlation. J Ultrasound Med 36:409–420
Lung PFC, Fang C, Jaffer OS et al (2020) Vascularity of Intra-testicular Lesions: Inter-observer Variation in the Assessment of Non-neoplastic Versus Neoplastic Abnormalities After Vascular Enhancement With Contrast-Enhanced Ultrasound. Ultrasound in Medicine & Biology 46:2956–2964
Stewart VR, Sidhu PS (2007) The testis: the unusual, the rare and the bizarre. Clinical Radiology 62:289–302
Rafailidis V, Huang DY, Sidhu PS (2021) Paratesticular lesions: Aetiology and appearances on ultrasound. Andrology 9:1383–1394
Rafailidis V, Robbie H, Konstantatou E et al (2016) Sonographic imaging of extra-testicular focal lesions: comparison of grey-scale, colour Doppler and contrast-enhanced ultrasound. Ultrasound 24:23–33
Secil M, Bertolotto M, Rocher L et al (2017) Imaging Features of Paratesticular Masses. J Ultrasound Med 36:1487–1509
Satchithananda K, Aziz ZA, Sidhu PS (2002) High frequency colour Doppler US of spermatic cord vessels: resistive index parameters in a cohort of 51 healthy men. Eur Radiol 12:328
Berner JE, Yeats R, Crowley TP et al (2020) Sarcomas in the groin and inguinal canal: A 16-year single-centre experience. Journal of Plastic, Reconstructive & Aesthetic Surgery
Coleman J, Brennan MF, Alektiar K, Russo P (2003) Adult Spermatic Cord Sarcomas: Management and Results. Annals of Surgical Oncology 10:669–675
Naser-Tavakolian A, Gulati M, Duddalwar V, Chopra S, Aron M, Djaladat H (2018) Contrast-Enhanced Ultrasound of Spermatic Cord and Retroperitoneal Liposarcoma. Ultrasound Q 34:292–296
Secil M, Kefi A, Gulbahar F, Aslan G, Tuna B, Yorukoglu K (2004) Sonographic Features of Spermatic Cord Leiomyosarcoma. Journal of Ultrasound in Medicine 23:973–976
Stewart VR, Sriprasad S, Pomplun S, Walsh K, Sidhu PS (2007) Sonographic Features of a Spermatic Cord Capillary Hemangioma. Journal of Ultrasound in Medicine 26:139–142
Ramanathan S, Bertolotto M, Freeman S et al (2021) Imaging in scrotal trauma: a European Society of Urogenital Radiology Scrotal and Penile Imaging Working Group (ESUR-SPIWG) position statement. European Radiology 31:4918–4928
Buckley JC, McAninch JW (2006) Diagnosis and management of testicular ruptures. Urol Clin North Am 33:111–116
Guichard G, El Ammari J, Del Coro C et al (2008) Accuracy of ultrasonography in diagnosis of testicular rupture after blunt scrotal trauma. Urology 71:52–56
Bhatt S, Dogra VS (2008) Role of US in testicular and scrotal trauma. Radiographics 28:1617–1629
Nicola R, Carson N, Dogra VS (2014) Imaging of traumatic injuries to the scrotum and penis. AJR Am J Roentgenol 202:W512-W520
Purushothaman H, Sellars ME, Clarke JL, Sidhu PS (2007) Intra-testicular haematoma: differentiation from tumour on clinical history and ultrasound appearances in two cases. Br J Radiol 80:e184-e187
Marko J, Wolfman DJ, Aubin AL, Sesterhenn IA (2017) Testicular Seminoma and Its Mimics: From the Radiologic Pathology Archives. Radiographics 37:1085–1098
Yusuf GT, Konstantatou E, Sellars ME, Huang DY, Sidhu PS (2015) Multiparametric sonography of testicular hematomas. Features on grayscale, color Doppler, and contrast-enhanced sonography and strain elastography. J Ultrasound Med 34:1319–1328
Yusuf GT, Rafailidis V, Moore S et al (2020) The role of contrast-enhanced ultrasound (CEUS) in the evaluation of scrotal trauma: a review. Insights into Imaging 11:68
Hedayati V, Sellars ME, Sharma DM, Sidhu PS (2011) Contrast-enhanced ultrasound in testicular trauma: Role in directing debridement and aiding organ salvage. Br J Radiol 1:1–1
Lotti F, Maggi M (2015) Ultrasound of the male genital tract in relation to male reproductive health. Human Reproduction Update 21:56–83
Miller FNAC, Rosairo S, Clarke JL, Sriprasad S, Muir GH, Sidhu PS (2006) Testicular calcification and microlithiasis: association with primary intra-testicular malignancy in 3,477 patients. Euro Radiol 17:363–369
Patel KV, Navaratne S, Bartlett E et al (2016) Testicular microlithiasis: Is sonographic surveillance necessary? Single centre 14 year experience in 442 patients with testicular microlithiasis. Ultraschall in Med 37:68–73
Miller FNAC, Sidhu PS (2002) Does testicular microlithiasis matter? A review. Clin Radiol 57:883–890
Pedersen MR, Møller H, Osther PJS, Vedsted P, Holst R, Rafaelsen SR (2017) Comparison of Tissue Stiffness Using Shear Wave Elastography in Men with Normal Testicular Tissue, Testicular Microlithiasis and Testicular Cancer. Ultrasound Int Open 3:E150-e155
Pedersen MR, Bartlett EC, Brown C, Rafaelsen SR, Sellars ME, Sidhu PS (2018) Is Testicular Macrocalcification a Risk for Malignancy?: Tumor Development on Ultrasonographic Follow-up of Preexisting Intratesticular Macrocalcification. Journal of Ultrasound in Medicine 37:2949–2953
O’Flynn EA, Sidhu PS (2009) The Sonographic Twinkling Artifact in Testicular Calcification. Journal of Ultrasound in Medicine 28:515–517
Huang DY, Alsadiq M, Yusuf GT, Deganello A, Sellars ME, Sidhu PS (2024) Multiparametric Ultrasound for Focal Testicular Pathology: A Ten-Year Retrospective Review. Cancers (Basel) 16:2309
Pozza C, Tenuta M, Sesti F et al (2023) Multiparametric Ultrasound for Diagnosing Testicular Lesions: Everything You Need to Know in Daily Clinical Practice. Cancers (Basel) 15:5332
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work; drafted the work or revised it critically for important intellectual content; approved the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.PSS Wrote the main text and prepared the figuresPSS, GTY, MES, AD, CF, DYF Collected data, involved in clinical cases, reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sidhu, P.S., Yusuf, G.T., Sellars, M.E. et al. A review of multiparametric ultrasound imaging in the clinical setting: scrotal contents. Abdom Radiol (2024). https://doi.org/10.1007/s00261-024-04587-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00261-024-04587-z