Abstract
Background
Immunoglobulin G4-related disease (IgG4-RD) is a systemic, immune-mediated disease that can affect multiple organs, including the orbits, salivary glands, thyroid gland, lungs, aorta, pancreas, bile ducts, lymph nodes, and retroperitoneum. While timely diagnosis is particularly important given the efficacy of glucocorticoid treatment for IgG4-RD, accurate recognition can prove a challenge given the overlap between the imaging features of this disease and other entities.
Purpose
After a review of the epidemiology, pathophysiology, and clinical considerations (including treatment) associated with IgG4-RD, this pictorial review will showcase the variable imaging manifestations of this disease in the abdomen and pelvis. Post-treatment imaging appearance of these entities will be reviewed and mimickers of this disease in the abdomen and pelvis will be presented.
Conclusion
The presence of mass-like soft tissue with radiographic characteristics of fibrosis affecting multiple organs should raise suspicion for IgG4-RD, although definite diagnosis can only be made with appropriate clinical, serological, and pathologic data.
Graphical abstract














Similar content being viewed by others
References
Kamisawa, T., et al., IgG4-related disease. The Lancet, 2015. 385(9976): p. 1460-1471.
Smyrk, T.C., Pathological features of IgG4-related sclerosing disease. Current opinion in rheumatology, 2011. 23(1): p. 74-79.
Carruthers, M.N., et al., The diagnostic utility of serum IgG4 concentrations in IgG4-related disease. Annals of the rheumatic diseases, 2015. 74(1): p. 14-18.
Umehara, H., et al., A novel clinical entity, IgG4-related disease (IgG4RD): general concept and details. Modern rheumatology, 2012. 22(1): p. 1-14.
Wang, L., et al., Sex disparities in clinical characteristics and prognosis of immunoglobulin G4–related disease: a prospective study of 403 patients. Rheumatology, 2019. 58(5): p. 820-830.
Wallwork, R., et al., The association of smoking with immunoglobulin G4–related disease: a case–control study. Rheumatology, 2021. 60(11): p. 5310-5317.
Smerla, R.G., D. Rontogianni, and G.E. Fragoulis, Ocular manifestations of IgG4-related disease in children. More common than anticipated? Review of the literature and case report. Clinical Rheumatology, 2018. 37: p. 1721-1727.
Chen, Y., et al., Aberrant expansion and function of follicular helper T cell subsets in IgG4‐related disease. Arthritis & Rheumatology, 2018. 70(11): p. 1853-1865.
Ito, F., et al., IL-10+ T follicular regulatory cells are associated with the pathogenesis of IgG4-related disease. Immunology Letters, 2019. 207: p. 56-63.
Mattoo, H., et al., Clonal expansion of CD4+ cytotoxic T lymphocytes in patients with IgG4-related disease. Journal of Allergy and Clinical Immunology, 2016. 138(3): p. 825-838.
Zhang, P., et al., Phenotype, function and clinical significance of innate lymphoid cells in immunoglobulin G4–related disease. Rheumatology, 2022. 61(5): p. 2197-2209.
Mahajan, V.S., et al., IgG4-related disease. Annual Review of Pathology: Mechanisms of Disease, 2014. 9: p. 315-347.
LIU, L.J., et al., IgG subclass distribution, affinity of anti‐myeloperoxidase antibodies in sera from patients with Wegener's granulomatosis and microscopic polyangiitis. Nephrology, 2008. 13(7): p. 629-635.
Okazaki, K., et al., Recent advances in the concept and diagnosis of autoimmune pancreatitis and IgG4-related disease. Journal of gastroenterology, 2011. 46: p. 277-288.
Sah, R.P., et al., Differences in clinical profile and relapse rate of type 1 versus type 2 autoimmune pancreatitis. Gastroenterology, 2010. 139(1): p. 140-148.
Perugino, C.A. and J.H. Stone, IgG4-related disease: an update on pathophysiology and implications for clinical care. Nature Reviews Rheumatology, 2020. 16(12): p. 702-714.
Hamano, H., et al., Prevalence and distribution of extrapancreatic lesions complicating autoimmune pancreatitis. Journal of gastroenterology, 2006. 41: p. 1197-1205.
Wallace, Z.S., et al., IgG4‐related disease: clinical and laboratory features in one hundred twenty‐five patients. Arthritis & rheumatology, 2015. 67(9): p. 2466-2475.
Lanzillotta, M., G. Mancuso, and E. Della-Torre, Advances in the diagnosis and management of IgG4 related disease. Bmj, 2020. 369.
Fritz, S., Diagnosis and treatment of autoimmune pancreatitis types 1 and 2. British journal of surgery. 101(10): p. 1257-1265.
Hart, P.A., Clinical profiles and outcomes in idiopathic duct-centric chronic pancreatitis (type 2 autoimmune pancreatitis): the Mayo Clinic experience. Gut. 65(10): p. 1702-1709.
Hart, P.A., Long-term outcomes of autoimmune pancreatitis: a multicentre, international analysis. Gut. 62(12): p. 1771-1776.
Zhang, L., et al., Autoimmune pancreatitis (AIP) type 1 and type 2: an international consensus study on histopathologic diagnostic criteria. Pancreas, 2011. 40(8): p. 1172-1179.
Masamune, A., Nationwide epidemiological survey of autoimmune pancreatitis in Japan in 2016. Journal of gastroenterology. 55(4): p. 462-470.
Sahani, D.V., et al., Autoimmune pancreatitis: imaging features. Radiology, 2004. 233(2): p. 345-352.
Yang, D., et al., Autoimmune pancreatitis: radiologic findings in 20 patients. Abdominal imaging, 2006. 31: p. 94-102.
Vlachou, P.A., et al., IgG4-related Sclerosing Disease: Autoimmune Pancreatitis and Extrapancreatic Manifestations. Radiographics. 31(5): p. 1379-1402.
Carbognin, G., et al., Autoimmune pancreatitis: imaging findings on contrast-enhanced MR, MRCP and dynamic secretin-enhanced MRCP. La radiologia medica, 2009. 114(8): p. 1214-1231.
Suzuki, K., et al., CT findings in autoimmune pancreatitis: assessment using multiphase contrast-enhanced multisection CT. Clinical radiology, 2010. 65(9): p. 735-743.
Takahashi, M., Diagnostic imaging guide for autoimmune pancreatitis. Japanese journal of radiology. 38(7): p. 591-612.
Tang, C.S.W., N. Sivarasan, and N. Griffin, Abdominal manifestations of IgG4-related disease: a pictorial review. Insights into imaging, 2018. 9: p. 437-448.
Kim, H.J., et al., Pancreatic duct “Icicle sign” on MRI for distinguishing autoimmune pancreatitis from pancreatic ductal adenocarcinoma in the proximal pancreas. European radiology, 2015. 25: p. 1551-1560.
Martínez-de-Alegría, A., et al., IgG4-related disease from head to toe. Radiographics, 2015. 35(7): p. 2007-2025.
Ichikawa, T., et al., Duct-penetrating sign at MRCP: usefulness for differentiating inflammatory pancreatic mass from pancreatic carcinomas. Radiology, 2001. 221(1): p. 107-116.
Hirano, K., et al., Endoscopic evaluation of factors contributing to intrapancreatic biliary stricture in autoimmune pancreatitis. Gastrointestinal endoscopy, 2010. 71(1): p. 85-90.
Kawai, Y., et al., Autoimmune pancreatitis: assessment of the enhanced duct sign on multiphase contrast-enhanced computed tomography. European journal of radiology, 2012. 81(11): p. 3055-3060.
Hedgire, S.S., et al., The spectrum of IgG4-related disease in the abdomen and pelvis. American Journal of Roentgenology, 2013. 201(1): p. 14-22.
Muhi, A., et al., Mass-forming autoimmune pancreatitis and pancreatic carcinoma: differential diagnosis on the basis of computed tomography and magnetic resonance cholangiopancreatography, and diffusion-weighted imaging findings. Journal of magnetic resonance imaging. 35(4).
Hafezi-Nejad, N., et al., MR Imaging of Autoimmune Pancreatitis. Magnetic Resonance Imaging Clinics of North America, 2018. 26(3): p. 463-478.
Huggett, M.T., et al., Type 1 autoimmune pancreatitis and IgG4-related sclerosing cholangitis is associated with extrapancreatic organ failure, malignancy, and mortality in a prospective UK cohort. The American journal of gastroenterology, 2014. 109(10): p. 1675.
Culver, E.L. and G. Webster, IgG4-related sclerosing cholangitis. Biliary Disease: From Science to Clinic, 2017: p. 243-261.
Khosroshahi, A., A clinical overview of IgG4-related systemic disease. Current opinion in rheumatology. 23(1): p. 57-66.
Ghazale, A., Immunoglobulin G4-associated cholangitis: clinical profile and response to therapy. Gastroenterology (New York, N.Y. 1943). 134(3): p. 706-715.
Zheng, Y., et al., IgG4-related disease in the abdomen and pelvis: atypical findings, pitfalls, and mimics. Abdominal Radiology, 2020. 45: p. 2485-2499.
Tan, T.J., et al., Extrapancreatic findings of IgG4-related disease. Clinical radiology, 2014. 69(2): p. 209-218.
Horger, M., et al., Systemic IgG4-related sclerosing disease: spectrum of imaging findings and differential diagnosis. American Journal of Roentgenology, 2012. 199(3): p. W276-W282.
Madhusudhan, K.S., et al., IgG4-related sclerosing cholangitis: a clinical and imaging review. American Journal of Roentgenology, 2019. 213(6): p. 1221-1231.
Fujinaga, Y., et al., Characteristic findings in images of extra-pancreatic lesions associated with autoimmune pancreatitis. European journal of radiology, 2010. 76(2): p. 228-238.
Nikiphorou, E., Overview of IgG4-related aortitis and periaortitis. A decade since their first description. Autoimmunity reviews. 19(12).
Neild, G.H., Hyper-IgG4 disease: report and characterisation of a new disease. BMC medicine. 4(1).
Zen, Y., Retroperitoneal fibrosis: a clinicopathologic study with respect to immunoglobulin G4. The American journal of surgical pathology. 33(12): p. 1833-1839.
Hamano, H., Hydronephrosis associated with retroperitoneal fibrosis and sclerosing pancreatitis. Lancet. 359(9315): p. 1403-1404.
Stone, J.R., Aortitis, periaortitis, and retroperitoneal fibrosis, as manifestations of IgG4-related systemic disease. Current opinion in rheumatology. 23(1): p. 88-94.
Khosroshahi, A., Rethinking Ormond's disease: "idiopathic" retroperitoneal fibrosis in the era of IgG4-related disease. Medicine (Baltimore). 92(2): p. 82-91.
Kim, J.H., et al., Atypical manifestations of IgG4-related sclerosing disease in the abdomen: imaging findings and pathologic correlations. American Journal of Roentgenology, 2013. 200(1): p. 102-112.
Cohan, R.H., et al., Imaging appearance of fibrosing diseases of the retroperitoneum: can a definitive diagnosis be made? Abdominal Radiology, 2018. 43: p. 1204-1214.
Perugino, C.A., Large vessel involvement by IgG4-related disease. Medicine (Baltimore). 95(28).
Peng, L., IgG4-related aortitis/periaortitis and periarteritis: a distinct spectrum of IgG4-related disease. Arthritis research & therapy. 22(1).
Ozawa, M., et al., Clinical features of IgG4-related periaortitis/periarteritis based on the analysis of 179 patients with IgG4-related disease: a case–control study. Arthritis research & therapy, 2017. 19: p. 1-9.
Fragoulis, G.E., Vasculitis beyond aortitis in IgG4-related disease (IgG4-RD): case report and review of the literature. Clinical rheumatology. 40(3): p. 1167-1173.
Inoue, D., IgG4-related disease: dataset of 235 consecutive patients. Medicine (Baltimore). 94(15).
Inoue, D., Immunoglobulin G4-related periaortitis and periarteritis: CT findings in 17 patients. Radiology. 261(2): p. 625-633.
Oyama-Manabe, N., et al., RadioGraphics Update: IgG4-related Cardiovascular Disease from the Aorta to the Coronary Arteries. RadioGraphics, 2020. 40(7): p. E29-E32.
Lanzafame, L.R., et al., Multimodality Imaging Evaluation of Coronary IgG4-Related Disease: A “Tumor-Like” Cardiac Lesion. Diagnostics, 2022. 12(11): p. 2814.
Mizushima, I., et al., Clinical course after corticosteroid therapy in IgG4-related aortitis/periaortitis and periarteritis: a retrospective multicenter study. Arthritis research & therapy, 2014. 16(4): p. 1-11.
Cheuk, W., et al., Lymphadenopathy of IgG4-related sclerosing disease. The American journal of surgical pathology, 2008. 32(5): p. 671-681.
Zen, Y. and Y. Nakanuma, IgG4-related disease: a cross-sectional study of 114 cases. The American journal of surgical pathology, 2010. 34(12): p. 1812-1819.
Saegusa, H., et al., Hilar and pancreatic gallium-67 accumulation is characteristic feature of autoimmune pancreatitis. Pancreas, 2003. 27(1): p. 20-25.
Bookhout, C.E. and M.A. Rollins-Raval, Immunoglobulin G4–Related Lymphadenopathy. Surgical Pathology Clinics, 2016. 9(1): p. 117-129.
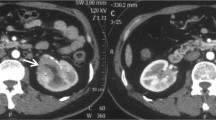
Saeki, T., et al., Clinicopathological characteristics of patients with IgG4-related tubulointerstitial nephritis. Kidney international, 2010. 78(10): p. 1016-1023.
Ling, J., et al., Clinical and imaging features of IgG4-related kidney disease. Abdominal Radiology, 2020. 45: p. 1915-1921.
Kim, B., et al., IgG4-related kidney disease: MRI findings with emphasis on the usefulness of diffusion-weighted imaging. European journal of radiology, 2014. 83(7): p. 1057-1062.
Yoshimura, Y., et al., IgG4-associated prostatitis complicating autoimmune pancreatitis. Internal Medicine, 2006. 45(15): p. 897-901.
Liu, H., et al. Prostate and pancreas involvement are linked in IgG4-related disease. in Seminars in Arthritis and Rheumatism. 2020. Elsevier.
Buijs, J., et al., Immunoglobulin G4-related prostatitis: a case-control study focusing on clinical and pathologic characteristics. Urology (Ridgewood, N.J.). 83(3): p. 521-526.
Jazdarehee, A., et al., IgG4-related prostatitis manifesting as urinary obstruction in a 28-year-old male. BMC urology, 2022. 22(1): p. 35.
Bourlon, M.T., et al., IgG4-related autoimmune prostatitis: is it an unusual or underdiagnosed manifestation of IgG4-related disease? Case reports in urology, 2013. 2013.
Nishimori, I., et al., IgG4-related autoimmune prostatitis: two cases with or without autoimmune pancreatitis. Internal Medicine, 2007. 46(24): p. 1983-1990.
Vadi, S.K., et al., IgG4-related disease simulating carcinoma colon with diffuse peritoneal carcinomatosis on 18F-FDG PET/CT. Clinical nuclear medicine, 2018. 43(7): p. e247-e249.
Coulier, B., et al., Small bowel obstruction caused by peritoneal immunoglobulin g4-related disease mimicking carcinomatosis: case report. Korean Journal of Radiology, 2014. 15(1): p. 66-71.
González-Moreno, J., et al., Serosal involvement in IgG4-related disease: report of two cases and review of the literature. Rheumatology international, 2016. 36: p. 1033-1041.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Suzanne Czerniak, Aditya Rao, and Mahan Mathur declares that they have no conflicts of interest
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Czerniak, S., Rao, A. & Mathur, M. Multimodality pictorial review of IgG4-related disease in the abdomen and pelvis. Abdom Radiol 48, 3147–3161 (2023). https://doi.org/10.1007/s00261-023-03996-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-023-03996-w